A key strategy in suicide prevention is the implementation of a minimum amount of training for suicide risk assessment and for treatment of suicidal behaviors. Suicide-specific training enhances the level of care that people who experience mental illness and suicide risk receive while also increasing provider competence and ability to provide effective, life-saving treatment.
American Foundation for Suicide Prevention, 2016
Suicide warning signs are indications of suicidal ideation and behavior that are observed by or reported to another, and indicate risk for suicide within minutes, hours, or days. Risk factors are characteristics, attributes, or exposures within an individual that increase the likelihood of developing a disease or injury (WHO, 2018). Most commonly, several risk factors act cumulatively to increase an individual’s vulnerability to suicidal behavior (WHO, 2014). Among these various risk factors, three stand out: mental illness, substance abuse, and medical issues.
Warning signs can be acute and urgent or simply red flags for concern. About 80% of people who attempt suicide show some sort of warning signs. Knowing and recognizing warning signs can help healthcare providers, family, and friends take action before suicidal thinking turns into action (WSDOH, 2016).
In general, suicide warning signs can include:
- Anxiety, agitation, sleeplessness, mood swings
- Purposelessness, hopelessness, feeling there is no reason to live
- Rage, anger, or aggression
- Recklessness, engaging in risky activities
- Increasing alcohol or drug abuse
- Withdrawing from family and friends
- Feeling trapped (U.S. Department of Veteran Affairs, 2016a)
Certain behavioral warning signs require immediate attention. Presence of one or more of these behaviors is a strong indication referral is acutely needed:
- Communicating suicidal thought verbally or in writing, especially if this is unusual or related to a personal crisis or loss
- Seeking access to lethal means such as firearms or medications, and
- Demonstrating preparatory behaviors such as putting affairs in order (USDVA, 2016b)
For young people increased risk has been associated with
- Family history of suicide
- History of depression
- Mental health problems
- Incarceration
- Easy access to lethal means
- Alcohol and drug use
- Exposure to previous suicidal behavior by others
- Loss of residential mobility (CDC, 2017b)
Individuals at a greater risk for completed suicide have been found to be
- Male
- Older
- Impulsive
- Having multiple physical ailments
- Prior suicide attempts
- Psychiatric illness
- History of violence
- Family history of suicide (Hassamal et al., 2015)
Clients admitted for inpatient treatment in specialized mental health facilities have a 50 to 200 times increased suicide risk compared to the population at large. In psychiatric inpatients, an array of risk factors for suicide has been identified:
- Prior suicide attempts
- Deliberate self-harm
- Family history of suicide
- Suicidal ideation
- Depression, hopelessness
- Agitation
- Social or relationship problems (Fosse et al., 2017)
Single studies have reported additional risk factors such as command hallucinations, delusions, mental disorders other than depression, coexisting physical illness, family history of mental illness, multiple admissions to inpatient treatment, unplanned discharge, and prescription of antidepressants (Fosse et al., 2017).
Mental Health Issues and Mental Illness
Suicide is overrepresented in people with mental illness (Fosse et al., 2017). The odds for suicide in severe depression, schizophrenia, and bipolar disorder are approximately 3 to 10 times that of the general population, with a higher increased risk in males than females. However, keep in mind that despite these statistics, suicide does not occur in 95% to 97% of people with mental illness (Fosse et al., 2017).
Impulsivity and disinhibition are overarching issues related to suicidal ideation and behavior. In fact, angry impulsivity has been repeatedly identified as a risk factor for suicidal behavior. Impulsivity is highly associated with bipolar disorder, substance abuse, and certain personality disorders as well as a history of early child abuse (Fawcett, 2012).
However, differences exist among those with and without mental health conditions. People without known mental health conditions were more likely to be male and to die by firearm. More than half of people who died by suicide did not have a known mental health condition (CDC, 2018).
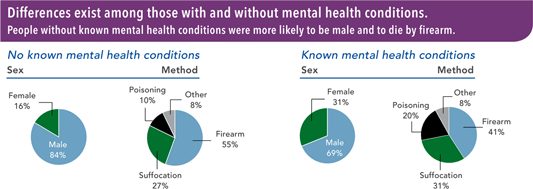
Source: CDC, 2018. Public domain.
Substance Abuse
People with substance use disorders often seek treatment at times when their substance use difficulties are at their peak—a vulnerable period that may be accompanied by suicidal thoughts and behaviors. Clients in treatment for substance abuse should be screened for suicidal thoughts and behavior routinely during intake and at specific points during the course of treatment. Compared with the general population, people being treated for alcohol use disorder are at about 10 times greater risk for suicide, while people who inject drugs are at about 14 times greater risk (CSAT, 2015).
Substance Use Disorder
The Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) refers to substance use disorders as mild, moderate, or severe to indicate the level of severity, which is determined by the number of diagnostic criteria met by an individual. The most common substance use disorders in the United States include:
- Alcohol Use Disorder (AUD)
- Tobacco Use Disorder
- Cannabis Use Disorder
- Stimulant Use Disorder
- Hallucinogen Use Disorder
- Opioid Use Disorder
Source: SAMSHA, 2015a.
Abstinence should be a primary goal of any client with a substance use disorder and suicidal thoughts or behaviors. For most clients abstinence reduces risk, although some individuals remain at risk even after achieving this goal (CSAT, 2015).
Key Point
Although a large proportion of suicides could be avoided with effective treatment of mental disorders, 50% to 75% of those in need receive inadequate treatment. The under-recognition of mental conditions seriously limits the potential to identify and appropriately treat individuals at risk for suicide.
Source: DVA/DOD, 2013).
Medical Issues and Physical Illness
Clients referred to physical or occupational therapy may be dealing with Illness, trauma, stressful life events, and injury. Chronic pain, cognitive changes, and challenges related to long-term conditions and limitations are associated with in increased risk of suicidal behavior (HHS, 2012).
Physical illness is a commonly overlooked risk factor for suicide. Medical patients often experience significant stressors, such as feeling like a burden to family, having concerns such as potential loss of employment or medical bills, or feeling alone and isolated. These powerful stressors can increase suicidal thoughts in vulnerable patients, particularly individuals who have a history of suicidal thoughts or behaviors. Thoughts of suicide are important to assess, especially in patients without known mental health disorders. For example, the vulnerability for suicide risk among individuals with cancer is highest in the first month after diagnosis, highlighting the critical need for early detection (Horowitz et al., 2016).
Co-morbid conditions may increase the likelihood that a suicide attempt becomes a completed suicide. For example, if a person with a chronic condition such as hepatitis C swallows a bottle of acetaminophen, they are likely to suffer severe liver damage. By the same token, a person with severe anemia may not survive a suicide attempt involving a significant loss of blood.
Warning Signs and Risk Factors for Suicide | |
|---|---|
Individual |
|
Relationship |
|
Community |
|
Societal |
|
