Ischemic Stroke Therapies
Ischemic stroke, resulting from thrombotic or embolic occlusion of an intracranial artery, accounts for 87% of all strokes (Go et al., 2014). The administration of intravenous fibrinolysis with recommended tissue plasminogen activator (rt-PA) within 3 to 4.5 hours of onset is the only current treatment shown to reduce disability from ischemic stroke.
Recombinant tissue plasminogen activator (rt-PA) is the only drug approved by the FDA for acute ischemic stroke and is ideally given intravenously within 3 hours of time of onset (the last time the patient was seen to be normal) of stroke symptoms; however, the best outcomes are associated with a door-to-treatment time of 60 minutes or less.
This window is often referred to as the golden hour of ischemic stroke treatment because during this time a focused diagnostic workup must be completed to rule out conditions that may mimic stroke as well as contraindications to rt-PA administration (Jauch, 2014). Additional procedures, such as interventional radiology and mechanical removal of the clot, have increased the time frame for ischemic stroke treatment (Gesensway, 2010).
Thrombolytics
The FDA approved the use of rt-PA in 1996, partly on the basis of a study done by the National Institutes of Neurological Disorders and Stroke (NINDS, 1995). The study, published in New England Journal of Medicine in 1995, showed neurologic improvement was achieved in 31% to 50% of patients treated with rt-PA compared with 20% to 38% of patients given a placebo. The major risk of treatment was symptomatic intracranial hemorrhage (NINDS, 2009).
The 1995 NINDS study was a major breakthrough in the treatment of ischemic stroke. The FDA, the AHA, the National Stroke Association (NSA), and the media touted the effectiveness of rt-PA (also known as alteplase). The AHA launched a nationwide campaign that encouraged use of the term brain attack instead of stroke, largely based on the purported effectiveness of alteplase.
A 1998 follow-up analysis of the NINDS trial found that after their initial hospitalization, people who received rt-PA were less likely to require inpatient rehabilitation or nursing home care. The authors estimated that this lower dependency on long-term care would translate into a savings to the healthcare system of more than $4 million for every one-thousand individuals treated with rt-PA (NINDS, 2009).
Because rt-PA interferes with blood clotting and has also been shown to increase leaking along the blood-brain barrier, it carries a risk of intracerebral hemorrhage. According to the original NINDS study, hemorrhage is most likely to occur in the first 3 hours after infusion but may occur up to 36 hours later. In the original study, intracranial hemorrhage occurred within 36 hours of treatment in 6.4% of the NINDS patients who received tPA as compared to 0.6% who received the placebo (NINDS, 1995). Nearly half of those hemorrhages were fatal.
Subsequent studies have demonstrated that using rt-PA more liberally than is recommended in the NINDS protocol resulted in a higher rate of intracranial hemorrhage. Complications are more likely when rt-PA is used in patients over 70 years old, those with more severe stroke (NIHSS over 15), or those with glucose over 300 mg/dl. Therefore, rt-PA is not recommended for patients who do not meet the inclusion and exclusion criteria. Because brain cells rapidly die as they are deprived of oxygen and because the risk of rt-PA-induced hemorrhage increases over time from stroke onset, its use is limited to the first 3 hours (in most cases) after the start of stroke symptoms (NINDS, 2009).
Thrombolytic agents are used to treat an ongoing acute ischemic stroke by restoring blood flow in the affected area, which may lead to improvements or resolution of neurologic deficits. rt-PA is a genetically engineered form of tPA, a thrombolytic or clot-busting substance made naturally by the body. It should be used only after it has been confirmed that the patient has suffered an ischemic stroke (NINDS, 2015b).
In an ischemic stroke, there is an area of irreversibly damaged brain tissue surrounded by an area of at-risk but viable tissue called the penumbra. During the first 3 to 4.5 hours after the onset of symptoms, reperfusion therapy can save this viable tissue by using clot-busting drugs (thrombolytics) to dissolve the clot. The longer therapy is delayed, the more brain cells will die (NINDS, 2009).
rt-PA is currently the only drug approved by the FDA for use in acute ischemic stroke (Rivera-Bou, 2014). It has a 30% recanalization rate when given within 3 hours of symptom onset in the acute setting, and has been shown to improve overall recovery rates at 1 year post stroke (Cronin, 2011).
For patients with ischemic stroke who meet the inclusion and exclusion criteria, the American College of Chest Physicians’ evidence-based clinical practice guidelines recommend administration of IV rt-PA in a dose of 0.9 mg/kg (maximum of 90 mg), with 10% of the total dose given as an initial bolus and the remainder infused over 60 minutes (AHRQ, 2012).
Contraindications for treatment with rt-PA include recent hemorrhage, increased risk of hemorrhage, arterial puncture at a non-compressible site, and systolic pressure >185 mm Hg or diastolic pressure >110 mm Hg (Papadakis et al., 2015).
As mentioned earlier, treatment must be initiated within 3 to 4.5 hours of clearly defined symptom onset and all unnecessary delays must be avoided because the benefits of rt-PA therapy diminish rapidly over time.
Did you know. . .
For patients with extensive and clearly identifiable hypo-density on CT, the guideline developers suggest not using rt-PA (AHRQ, 2012).
Unfortunately, fibrinolytics may also cause symptomatic intracranial hemorrhage. Other complications include significant hemorrhage, angioedema, or other allergic reactions (Adams et al., 2007). Therefore, when considering thrombolytics for a stroke patient with symptom onset greater than 3 hours and less than 4.5 hours, a thorough review of the inclusion and exclusion criteria must be performed.
Exclusion criteria largely focus on identifying risk of hemorrhagic complications associated with fibrinolytic use. A sample of the AHA/ASA inclusion guidelines for administering rt-PA are as follows:
- Diagnosis of ischemic stroke causing measurable neurologic deficit
- Neurologic signs not clearing spontaneously to baseline
- Neurologic signs not minor or isolated
- Symptoms do not suggest subarachnoid hemorrhage
- No head trauma or prior stroke in the past 3 months
- No myocardial infarction in the past 3 months
- No GI/GU hemorrhage in previous 21 days
- No major surgery in past 14 days
- Systolic blood pressure <185 mmHg, diastolic blood pressure <110 mmHg
- Not taking oral anticoagulant, or if taking oral anticoagulant INR <1.7
- Platelet count >100,000/µL
- Blood Glucose >50 mg/dL
- CT scan does not show evidence of multi-lobe infarction or intracerebral hemorrhage
- Family understands the potential risks and benefits of therapy (Adams et al., 2007)
Involvement of team members having stroke expertise is critical for assessing risk/benefit considerations and educating decision makers regarding realistic expectations.
Note: In 2009 the American Heart Association (AHA) and the American Stroke Association (ASA) published a science advisory recommending that the time window for rt-PA administration be increased to 4.5 hours after onset of stroke symptoms, although this change has not been approved by the FDA (Slater, 2014). Despite the potential benefit of rt-PA extending out to 4.5 hours, it should be administered as early as possible for the best outcome (Saver, 2014).
Interventional Radiology
Interventional radiology offers a longer treatment window for some patients with acute ischemic stroke. Intra-arterial rt-PA can be given up to 6 hours after onset of stroke symptoms and has the same efficacy as intravenous rt-PA. Using x-ray guidance, a catheter is threaded through the femoral artery into the tiny arteries of the brain where rt-PA is delivered directly into the clot (Cronin, 2011). Because less rt-PA is used, there is less chance of intracranial bleeding.
Mechanical clot removal can be a treatment option for stroke patients who may arrive at the hospital too late, or who have contraindications to the use of rt-PA. The mechanical embolus removal in cerebral ischemia (MERCI) retriever can be used up to 8 hours after symptom onset. The device is threaded through the femoral artery to the site of the stroke to retrieve the clot. The retriever has received approval from the FDA for use in patients with persistent vessel occlusion after IV rt-PA (Lutsep, 2013).
One study showed recanalization occurred in 55% of patients who were treated with a MERCI device alone and in 68% of patients who were treated with a MERCI device plus adjuvant treatment (Lutsep, 2013).
Approved in 2007 by the FDA, the penumbra system uses aspiration to remove a clot. The system is threaded through the femoral artery via catheter to the thrombus site, where the radiologist breaks up the clot with a separator and then aspirates it. This system can be used up to 8 hours from symptom onset and has shown up to an 82% recanalization success rate (Cronin, 2011).
Antiplatelets
Antiplatelet therapy is used for both the prevention and management of acute ischemic stroke. Antiplatelet drugs inhibit the activity of cells called platelets, which stick to damaged areas inside blood vessels and lay the foundation for blood clots. Antiplatelets do not break up clots. Patients with ischemic stroke or TIA who are not on anticoagulation should be taking an antiplatelet agent such as aspirin. When patients are aspirin-intolerant, clopidogrel (Plavix), or a combination of low-dose aspirin and dipyridamole (Aggrenox), modified release, should be used. Dipyridamole may also be taken alone (AHRQ, 2010b).
Platelets Attached to Blood Vessels
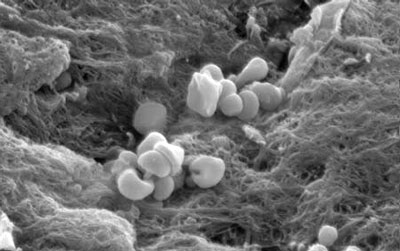
Platelets (magnified here thousands of times) cling to damaged areas of blood vessels and contribute to the formation of clots. Antiplatelet drugs can help reduce the risk of ischemic stroke. Source: NIH, n.d.
Aspirin is the oldest and most common antiplatelet medicine. In a meta-analysis of trials of aspirin in the secondary prevention of cardiovascular and cerebrovascular events, aspirin reduced the number of strokes by more than 20%. For patients with acute ischemic stroke who are not receiving thrombolysis, early aspirin therapy is recommended to stop the growth of the clot (initial dose of 150–325 mg) (AHRQ, 2010b). Aspirin has also been proven to be the most effective immediate treatment after an ischemic stroke to reduce the likelihood of another stroke. Aspirin should not be given within 24 hours of administration of rt-PA.
The maximal antiplatelet effect of aspirin may take several days when given in doses as low as 75 mg/day, so low doses are used for the long-term prevention of heart attacks and strokes. When immediate anti-clotting effects are needed, moderate doses of aspirin (160–325 mg) are used (medicinenet.com, 2009).
Anticoagulants
Anticoagulants reduce stroke risk by preventing the formation of clots and the extension of existing clots, but do not break them up. The most commonly used anticoagulants include warfarin (Coumadin), heparin, and enoxaparin (Lovenox) (NINDS, 2015a).
There have been several trials to test the efficacy of anticoagulants versus antiplatelet drugs. It has been found that, although aspirin is an effective therapy for the prevention of a second stroke in most patients with atrial fibrillation, some patients with additional risk factors do better on warfarin therapy. A recent study tested the effectiveness of low-molecular-weight heparin (enoxaparin) in stroke prevention. This study showed that heparin anticoagulants are not generally effective in preventing recurrent stroke or improving outcomes (NINDS, 2015a).
Warfarin (Coumadin)
Warfarin is often prescribed to prevent the possibility of clotting and stroke in patients with atrial fibrillation. Atrial fibrillation raises the risk of stroke 4 to 6 times. Some of these patients have a lower risk of stroke and are treated with aspirin, which reduces clotting but is not as strong as warfarin. Other treatments include medications such as beta blockers or calcium channel blockers to slow the heartbeat, and anti-arrhythmic drugs or electrical cardioversion to normalize the heartbeat (NINDS, 2009).
Although effective in prevention of clots, warfarin has many disadvantages. It carries many drug–drug and food–drug warnings that may result in either under- or over-coagulation of the blood as measured by the INR. Once patients on warfarin enter a period of instability with regard to their INR, they are subjected to frequent, occasionally daily, blood draws in order to prevent a dangerous bleed or clot from developing.
Heparin and Enoxaparin (Lovenox)
Heparin is an effective anti-coagulant, but only when given via intravenous therapy. Enoxaparin is also an effective anticoagulant, however it must be given subcutaneously up to several times a week, and compared to either warfarin or heparin, the cost is prohibitive for ongoing use and may not be covered for use in the outpatient setting.
Searching for drugs that combined ease of use, decreased monitoring requirements, and effectiveness, in 2010 the Food and Drug Administration (FDA) allowed three new drugs to be used in the United States.
Dabigatran (Pradaxa)
Dabigatran is the first of the three newer agents and was approved by the FDA for use in the United States in 2010. Dabigatran is a direct inhibitor of thrombin and can prevent thrombus development. It may be used as an alternative to warfarin for the prevention of stroke and systemic thromboembolism in patients with either paroxysmal or permanent atrial fibrillation.
Rivaroxaban (Xarelto)
The second of the newer anticoagulants to be released is rivaroxaban. This was approved for use in the United States in 2011. Rivaroxaban is a Factor Xa inhibitor indicated to reduce the risk of stroke and systemic embolism in patients with non-valvular atrial fibrillation. The dose must be adjusted according to estimated creatinine clearance.
Apixaban (Eliquis)
Apixaban is also a Factor Xa inhibitor; it inhibits platelet activation, causing indirect inhibition of platelet aggregation induced by thrombin. Indications are substantially the same as those for the previous two agents. This drug received approval for use in the United States by the FDA in 2014.
Advantages of the New Agents
Advantages of these newer agents compared to warfarin is that they do not require routine coagulation monitoring tests and their onset of action is comparatively rapid. However, their anticoagulation effect declines quickly in the face of non-compliance (Gomez-Outes et al., 2012). Additional advantages are minimal drug and dietary interactions. These properties allow the newer agents to be administered in fixed doses without regular monitoring, making them more convenient to use in the outpatient setting (Eriksson et al., 2011).
Patients with acute ischemic stroke treated with rt-PA should not be treated with anticoagulation for at least 24 hours post thrombolysis (Cruz-Flores, 2015).
At the present time, patients with acute ischemic stroke treated with intravenous recombinant tissue plasminogen activator (rtPA) clearly should not be treated with anticoagulation for at least 24 hours post thrombolysis (Cruz-Flores, 2015).
Hemorrhagic Stroke Therapies
[This section taken largely from National Heart Lung and Blood Institute, 2014.]
Hemorrhagic stroke occurs if an artery in the brain leaks blood or ruptures. Patients with hemorrhagic stroke usually present with neurologic symptoms similar to ischemic stroke patients, but they tend to be sicker. The first step in treating a hemorrhagic stroke is to find the cause of bleeding in the brain and then control it.
Surgery may be needed to treat a hemorrhagic stroke. If an aneurysm is the cause of a stroke, aneurysm clipping or coil embolization may be done. An aneurysm clipping is done to block off the aneurysm from the blood vessels in the brain. During the procedure, a surgeon places a tiny clamp at the base of the aneurysm.
Coil embolization is a less complex procedure for treating an aneurysm. The surgeon inserts a catheter into an artery in the groin that is threaded to the site of the aneurysm. A tiny coil is then pushed through the tube and into the aneurysm, causing a blood clot to form, blocking blood flow through the aneurysm, and preventing it from bursting again.
If an arteriovenous malformation (a tangle of faulty arteries and veins that can rupture within the brain) is the cause of hemorrhagic stroke, a repair may be done to prevent further bleeding. Types of repair are:
- Surgery to remove the arteriovenous malformation
- Injection of a substance into the blood vessels of the arteriovenous malformation to block blood flow
- Radiation to shrink the blood vessels of the arteriovenous malformation
Did you know. . .
All strokes are treated as ischemic until a CT scan confirms otherwise. The reason is that, with an ischemic stroke, the staff must follow the strict timeline and protocol for possible rt-PA administration. If a hemorrhage is present, different treatment is required.
