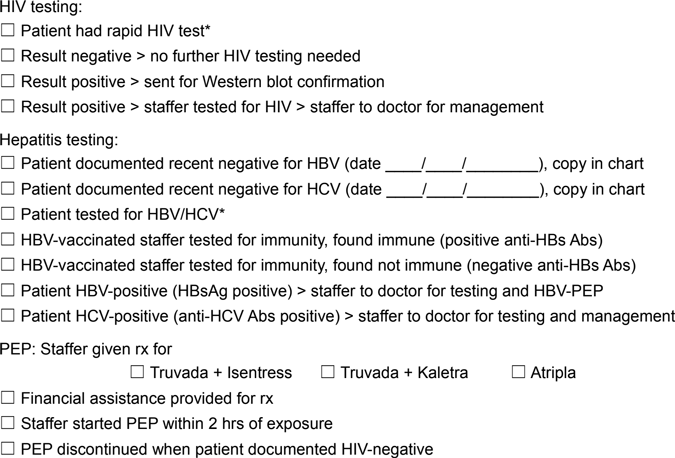
Jennifer’s needle stick protocol checklist included the incident report, exposed employee date of birth and contact info, her own risk status and information about her date, time and route of exposure. The required HIV testing included the following on the infection control nurse’s checklist:
Source: Needle stick protocol, occupy-medical.org. (n.d.).
When to Wear PPE
Personalized Protection Equipment (PPE) is specialized clothing or equipment worn by an employee for protection against hazards that remain after engineering controls and work practice controls are in place. PPE is not the first line of defense! Legally, the employer must provide PPE, ensure that the employee uses and must clean, repair, and replace this equipment as needed. You as the employee have the right to have PPE available to complete your job duties.
PPE includes gloves, gowns, laboratory coats, face shields or masks, eye protection, resuscitation masks, and other protective gear such as hats and booties. It may also include full protection suits, as were used for the Ebola patients. It must be readily accessible to employees and available in appropriate sizes. The hospital infection control process often determines the isolation requirements for patents including contact, droplet, and airborne and will require nurses and visitors to follow the protocol for each type of isolation.
The worker often must decide on their own when to wear PPE because exposure is likely. If exposure seems reasonably likely, you have the right to protect yourself with PPE.
An easy guideline to use is
If it is wet and not yours, stay out of it!
Gloves shall be worn when:
- It can reasonably be anticipated that the employee may have hand contact with blood, OPIM, mucous membranes and non-intact skin
- Performing all vascular access procedures or procedures involving uncontained blood, such as finger or heel sticks
- Gloves must be changed between patients (CDC, 2013)
Single use gloves cannot be washed or decontaminated for reuse. Utility gloves worn by engineering or housekeeping may be decontaminated if they are not compromised. They should be replaced when they show signs of cracking, peeling, tearing, puncturing, or deteriorating.
Traditionally, latex gloves are used to avoid contact with blood or OPIM. However, some workers are allergic to latex or vinyl. In most circumstances, nitrile or other glove alternatives may be used in place of latex gloves. Employers are required to provide non-latex alternatives to employees with sensitivities to latex and other materials. Sterile or nonsterile gloves are also available as PPE and dictated by the procedure.
Do’s and Don’ts of Glove Use | |
|---|---|
Do | Don’t |
Work from clean to dirty | Touch your face |
Limit opportunities for touch contamination | Adjust the PPE with a contaminated glove |
Double glove if changing a very soiled bed/bowel movement | Touch environmental surfaces except as necessary during patient care |
Change gloves if torn, heavily soiled and between patients | Wash or reuse gloves |
Employees should wear eye and mouth protection such as goggles and masks, glasses with solid side shields, and masks or face shields when splashes, sprays, splatters, or droplets of blood or OPIM pose a hazard to eyes, nose, or mouth.
Gowns, aprons, surgical caps and hoods, shoe covers, or boots are needed when splash, spray, or gross contamination is expected. This may occur, for example, during labor and delivery, surgery and procedures with anticipated blood splash may occur.
Employers must provide the PPE and ensure that their workers wear it. This means that if a lab coat is considered PPE, it must be supplied by the employer rather than the employee. The employer also must clean or launder clothing and equipment and repair or replace it as necessary. This includes, but is not limited to dentistry, phlebotomy or processing of any body fluid specimen, and postmortem procedures.
Personal protective clothing and equipment must be appropriate for the level of protection needed for the expected exposure. For example, gloves would be sufficient for a laboratory technician who is drawing blood, whereas a pathologist conducting an autopsy would need considerably more protective clothing. Personal protective equipment may be required during the care of any patient, so it must be routinely available in patient-care areas, not just on isolation carts. You may need to wear a mask and eye protection during the care of a patient on Standard or Universal Precautions. Availability of PPE is required by the OSHA Standard. If you are not sure where to obtain it, ask your employer.
What PPE to Wear
Knowing what to wear for each different type of isolation is important for your protection. Factors influencing PPE selection include the fit, the type of exposure anticipated, durability, and appropriateness for the task.
Airborne | Contact | Droplet |
Gloves | Gloves | Gloves |
Gown | Gown | Gown |
N95 Respirator | Goggle/Face shield if splash anticipated, but not needed for standard contact isolation | Goggles/Face shield |
What PPE would you wear for these patient encounters? | |
|---|---|
Encounter | Type of PPE |
Giving a bed bath? | generally none |
Suctioning oral secretions? | gloves and mask/goggles or a face shield |
Transporting a patient in a wheelchair? | generally none |
Responding to an emergency where blood is spurting? | gloves, fluid-resistant gown, mask/goggles or a face shield |
Drawing blood from a vein? | gloves |
Cleaning an incontinent patient with diarrhea? | gloves and generally a gown |
Irrigating a wound? | gloves, gown, and mask/goggles or a face shield |
Taking vital signs? | generally none |
Exception
The employer shall ensure that the employee uses appropriate PPE unless the employer shows that the employee temporarily and briefly declined to use PPE when, under rare and extraordinary circumstances, it was the employee's professional judgment that in the specific instance its use would have prevented the delivery of healthcare or public safety services or would have posed an increased hazard to the safety of the worker or co-worker.
When the employee makes this judgment, the circumstances shall be investigated and documented in order to determine whether changes can be instituted to prevent such occurrences in the future. In other words, if using PPE would increase danger to the person receiving care or to the worker, then the worker may decline to use the PPE, but situations like this must be reported and investigated, and are rare.
Decontaminating and Disposing of PPE
Employees must remove personal protective clothing and equipment before leaving the work area or when the PPE becomes contaminated. If a garment is penetrated, workers must remove it immediately or as soon as feasible. Used protective clothing and equipment must be placed in designated containers for storage, decontamination, or disposal.
While use of PPE cannot prevent all exposures, wearing it properly and when needed can greatly reduce potential exposure to all bloodborne pathogens. The sequence for removing PPE is:
Gloves —> Goggles —> Gown —> Mask
Test Your Knowledge
Personal protective equipment:
- Should be purchased by employees who are in frequent contact with blood or other body fluids.
- Include only latex gloves, which have been shown to be the only type of glove that protects against bloodborne pathogens.
- Are devices that isolate or remove the bloodborne pathogen hazard from the workplace.
- Must be provided by the employer, who is required to clean, repair and replace it as needed.
Apply Your Knowledge
How diligent are you in using PPE’s in your facility? How meticulous are you in removing them correctly? Do you know the correct process to remove a gown, glove, and mask and do you follow it? What would you do if you saw a colleague using PPEs incorrectly with an isolation patient? How do you instruct and reinforce a visitor to wear PPEs in an isolation room when visiting?
Answer: D
