Mental health has traditionally been within the purview of psychiatrists and specifically trained mental health practitioners. Now it is not uncommon for a variety of healthcare providers to find themselves at the front lines of identifying serious mental health issues that require screening and referral. Because of these changes, it is important to be knowledgeable about suicide risk factors and warning signs, understand suicide screening tools, and know when, where, and how to refer a patient who is at risk for self-harm.
A web of biological, psychological, social, environmental, and situational concerns influences suicidal ideation and behaviors. Childhood trauma, substance abuse, poverty, and untreated mental health problems are common risk factors. Unfortunately, many people are not able to get help because of provider shortages, stigma, and the cost of care.
In 2022, more than 49,000 Americans died from suicide—the highest number ever recorded in the U.S.—making it the eleventh leading cause of death overall. Remarkably, each year there are more than twice as many suicides as homicides in the United States (NCHS, 2023).
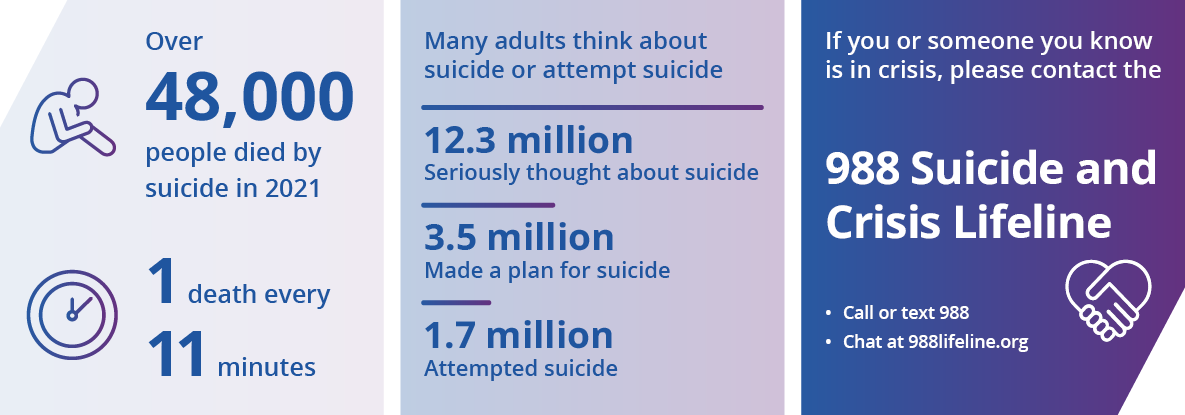
Source: CDC, 2023, May 8.
During the COVID pandemic, there was a record increase in homicides and a spike in the number of drug overdose deaths. It was assumed that suicide rates would follow a similar pattern—particularly after the number of suicides had risen every year between 2004 and 2019. However, between 2018 and 2019, there was a minor decline in suicide, and this decline continued both males and females into the pandemic year of 2020 (CDC, 2021, November 5).
Suicide Rates in the United States
(by state; per 100,000 population; 2021)
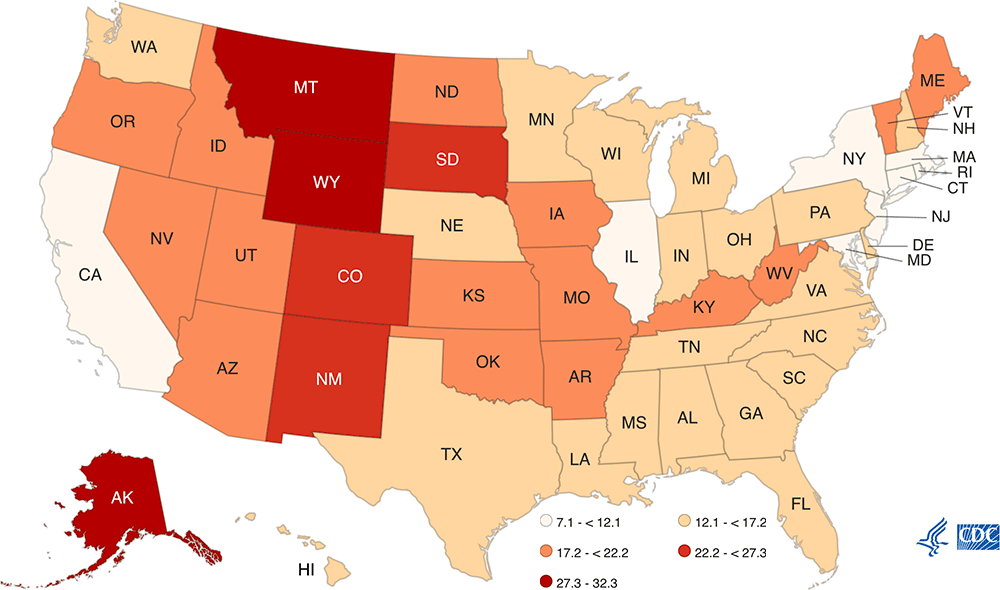
Suicide rates vary from state to state. In general, the Western states (excluding California), have some of the highest rates of suicide in the country. Source: CDC, 2023, May 1.
Suicide is not limited to any gender, age, socioeconomic, or ethnic group. Among children, teenagers, and young adults, suicide is the second leading cause of death, while among middle-aged adults (age 35 to 54), suicide is the fifth leading cause of death (NCHS, 2022, March 3).
Definitions
Suicide: death caused by self-directed injurious behavior with intent to die.
Suicide attempt: when someone harms themself with any intent to end their life but does not die.
Suicide ideation: thinking about, considering, or planning suicide.
1.1 Suicide is a Major Public Health Concern
Many factors contribute to suicide among people with and without mental health concerns. More than half of people who die by suicide do not have a known diagnosed mental health condition at the time of death. Relationship problems or loss, substance misuse, physical health problems, and job, money, legal or housing stress often contribute to an increased risk for suicide.
In the United States, among youth and young adults aged 10-34, suicide is the second leading cause of death. Suicide rates for females in all age groups over age 25 showed recent declines, while rates for those aged 10–14 and 15–24 have generally increased (Garnett et al., 2022).
Suicide attempts are more frequent among women although men have a higher rate of completed suicides. Men often use particularly lethal methods such as shooting by firearm, hanging, or suffocation, while women often attempt suicide by poisoning, wrist cutting, or falling from heights. From 2000-2020, the suicide rate for males was 3–4 times the rate for females (Garnett et al., 2022).
Percentage of Suicide Deaths by Method in the United States (2020)
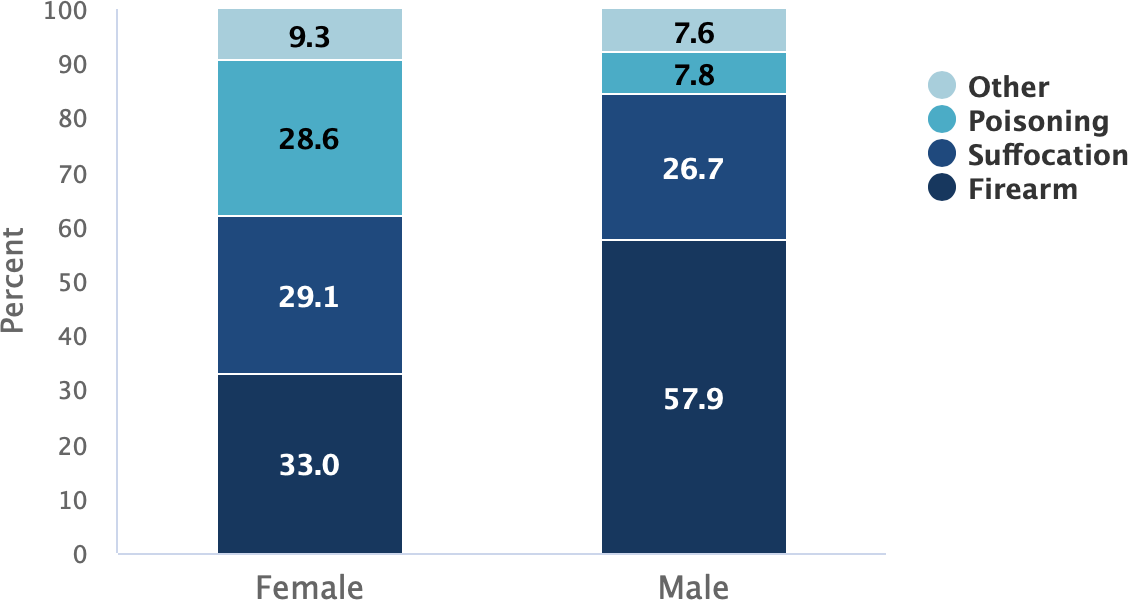
Source: nimh.nih.gov. May, 2023.
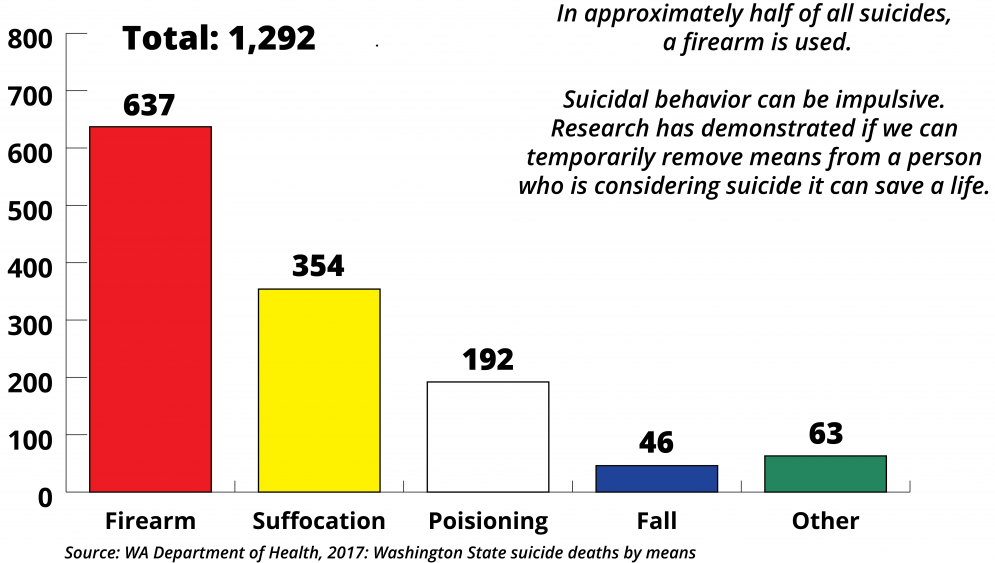
In Washington State, the suicide rate has been higher than the national average for more than 10 years. From 2010 to 2019, over 11,000 people in the state died as a result of suicide. The most common means were firearms, followed by suffocation and poisoning (deGrauw, 2021).
Statistics from 2018 showed that more than 40% of people who died by suicide in Washington State had a history of suicidal thoughts. About 19% had served in the military. About a third of those who died by suicide left a note. Additionally:
- 75% were male
- 65% occurred at home
- 48% involved a firearm (WSDOH, 2020, November)
Washington State Suicide Deaths by Means, 2017
Suicide rates vary in different parts of Washington. But because of the way rates are compared, a small difference may be statistically significant while a larger one is not. Statistical significance means the difference is very unlikely to be due to chance. From 2013 to 2017, suicide rates were higher than the state rate in six counties:
- Clallam
- Grays Harbor
- Okanogan
- Pierce
- Skamania
- Stevens (WSDOH, 2016)
Seven counties in Washington have small populations and had too few suicides to calculate a suicide rate. This does not mean that there are not suicides in these counties; county-level data do not always accurately reflect suicide losses in communities. For example, in 2013 both the Spokane Tribe of Indians and the Colville Confederated Tribes declared a suicide state of emergency because of high numbers of suicide deaths (WSDOH, 2016).
Clark County’s Battle Ground School District, located in a town of fewer than 18,000 residents, lost seven students to suicide between 2011 and 2013. Neither pattern of loss was clear from a glance at county data. The suicide rate in King County is lower than the state rate, but it has the largest population and the highest number of suicides in the state (WSDOH, 2016).
Key Points about Suicide
- Suicide is preventable, it is not a personal weakness or family failure.
- Prevention is not the responsibility of the health system alone.
- Silence and stigma harm individuals, families, and communities.
- Suicide does not affect all communities equally or in the same way.
- Prevention programs must reflect community needs and local cultures.
Source: Washington State Department of Health, 2016
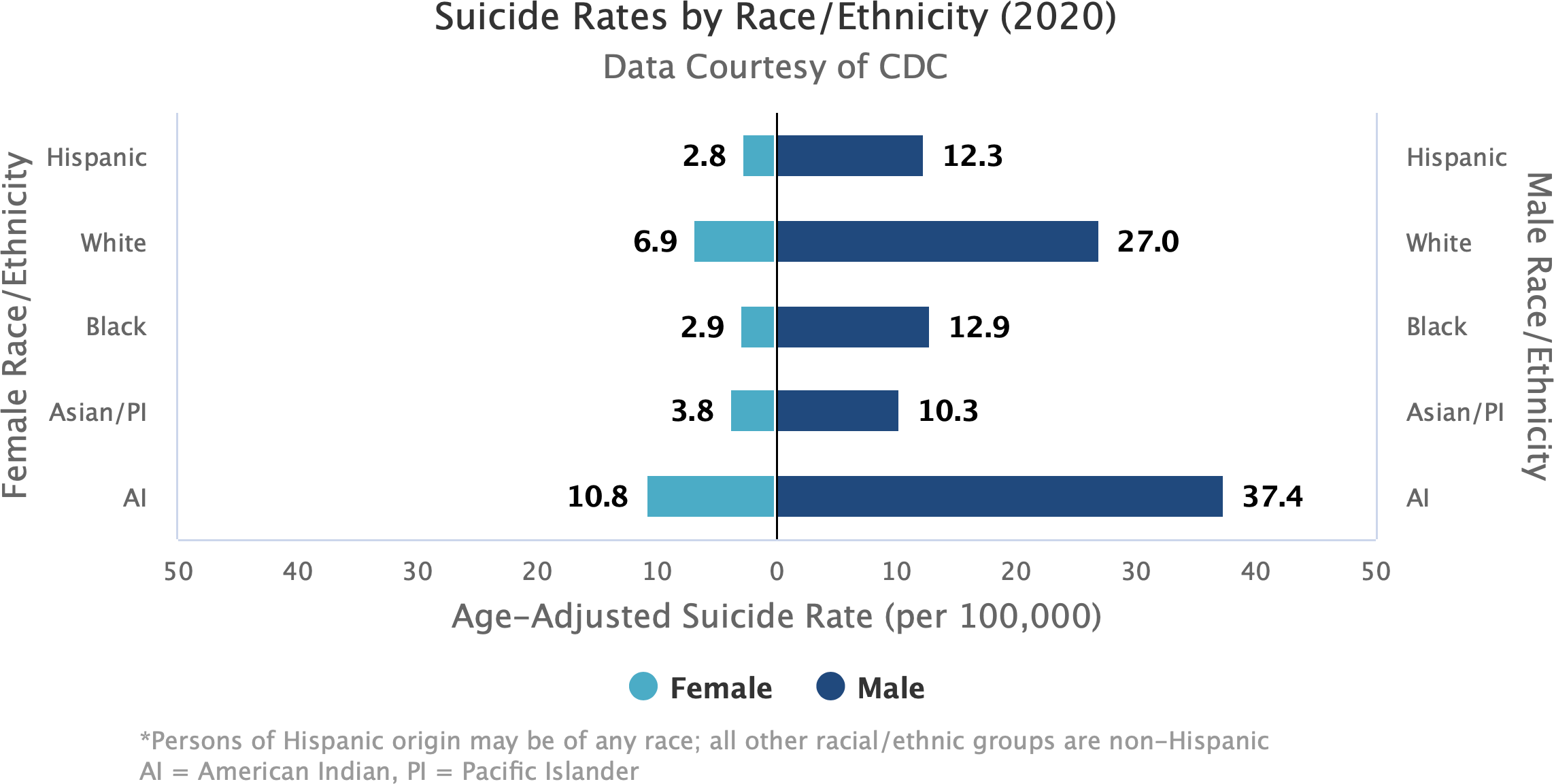
1.2 Suicide Rates by Race/Ethnicity, Age, and Gender
Suicide rates vary significantly by race, ethnicity, age, and gender. In 2019, Native American Indian and Alaska Native people had a suicide rate 60% greater than the general population (CDC, 2021 February 24).
The rates of suicide are highest for American Indian males, followed by White, non-Hispanic males. Among females the rates of suicide are highest for American Indian females and White, non-Hispanic females (NIMH, 2023, May).
For Native American Indian and Alaska Native peoples, sovereignty, community control, autonomy, cultural identification, language, spirituality, healing ways, kinship models, and family connectedness are all important protective factors in addressing high rates of suicide among Indigenous populations (Zero Suicide, 2022).
Did You Know. . .
Compared to non-Hispanic Whites, non-Hispanic Indigenous people who die by suicide are younger, live in more rural areas, are more likely to have a friend or family member who died by suicide, and are more likely to use alcohol (Leavitt, et al, 2018).
For Black Americans, rates are lower than that of the non-Hispanic White population. Nevertheless, in 2020, suicide was the third leading cause of death for Blacks Americans, ages 15 to 24. The suicide death rate for Black men was more than four times greater than for Black women (OMH, 2022).
Among Asian Americans, suicide rates are generally lower than for other racial/ethnic groups although rates are high for Korean Americans. Among the six largest Asian American subgroups* Korean males have more than twice the frequency of death due to suicide (5%) compared to non-Hispanic Whites (2%). Suicide rates in Korean Americans have nearly doubled from 2003 to 2012 and exceed rates for all other Asian American subgroups (Kung et al., 2018).
*Asian Indians, Chinese, Filipinos, Japanese, Koreans, and Vietnamese.
The suicide rate for Hispanics/Latinos in the United States has increased significantly over the past decade. For Hispanic children 12 and younger, the rate increased 92.3% from 2010 to 2019 (KFF, 2024).
The COVID pandemic hit young Hispanics especially hard. Immigrant children are often expected to take more responsibility when their parents don’t speak English—even if they themselves are not fluent. Many reside in poorer households with some or all family members without legal residency. And cultural barriers and language may prevent many from seeking care in a mental health system that already has spotty access to services (KFF, 2024).
https://www.nimh.nih.gov/health/statistics/suicide. May, 2023.
Youth and young adults ages 10–24 years account for 15% of all suicides. Although the suicide rate is lower than for other age groups, suicide is the second leading cause of death for this age group. Additionally, suicide rates for youth and young adults increased more than 50% between 2000-2021 (CDC, 2023, May 9).
Among youth, non-suicidal, self-injurious behaviors* such as cutting, burning, hitting oneself, scratching to the point of bleeding or interfering with healing can occur together with suicidal behaviors. It is important to consider the nature of the link between these types of behavior (Grandclerc et al., 2016).
*Self-injury is deliberate harm inflicted on a person’s own body.
In Washington, men account for more than three-quarters of suicide deaths. From 2012 to 2014, men 75 and older had the highest rate of suicide while men 45 to 64 had the highest number of suicides. For older men, contributing factors include economic insecurity, loss of significant relationships, loneliness, fear of being a burden, and the physical and mental stresses of aging (WSDOH, 2016).
In recent years, suicide rates for middle-aged women have increased by more than 30%, exceeding the increases observed among middle-aged men. However, using data from the Nurses’ Health Study, researchers determined women who were socially well integrated* had a more than 3-fold lower risk for suicide over 18 years of follow-up (Tsai et al., 2015). Although more men die from suicide, more women attempt suicide.
*Social integration: measured with a 7-item index that included marital status, social network size, frequency of contact with social ties, and participation in religious or other social groups (Tsai et al., 2015).
Suicide Rates by Sex in the United States (2000–2020)
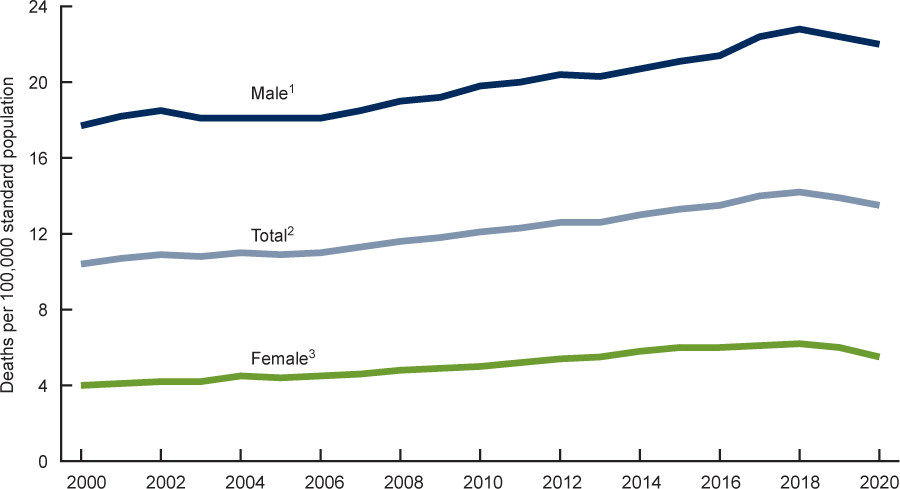
Source: Garnett et al. (2022).
