The vast majority of people who attempt suicide show some sort of warning sign or risk factor. Knowing and recognizing warning signs and risk factors allows healthcare providers, family, and friends to intervene before suicidal thinking turns into action.
2.1 Overview of Warning Signs
Warning signs are indications of suicidal ideation and behavior that are observed by or reported to another, and indicate risk for suicide within minutes, hours, or days.
In general, suicide warning signs are often accompanied by increased anxiety, agitation, sleeplessness, and mood swings. A previous suicide attempt and a history of substance abuse are red flags for another attempt. Feelings of hopelessness, feeling there is no reason to live, and withdrawing from family and friends are often present. Other general warning signs might include:
- increasing alcohol or drug abuse
- expressing feelings of rage, anger, or aggression
- engaging in risky activities
- feeling trapped
2.2 Overview of Risk Factors
Risk factors are characteristics, attributes, or exposures within an individual that increase the likelihood of developing a disease or injury. Risk factors can accumulate to increase an individual’s vulnerability to suicidal behavior.
Especially for young people, increased risk has been associated with a family history of suicide, exposure to previous suicidal behavior by others, a history of depression, or mental health problems. Additional risk factors associated with completed suicide include:
- incarceration
- easy access to lethal means
- alcohol and drug use
- loss of residential mobility
Among these various risk factors, three stand out:
- mental illness
- substance abuse
- medical issues
Individuals at a greater risk for completed suicide have been found to be older men, those with a family history of suicide, and people who have previously attempted suicide. Other risk factors include:
- impulsiveness
- multiple physical ailments
- psychiatric illness
- history of violence (Hassamal et al., 2015)
Patients admitted for inpatient treatment in specialized mental health facilities have a 50-to-200 times increased suicide risk compared to the population at large. In psychiatric inpatients, an array of risk factors for suicide has been identified including a family history of suicide, prior suicide attempts, and social or relationship problems. Other risk factors include:
- deliberate self-harm
- suicidal ideation
- depression, hopelessness
- agitation (Fosse et al., 2017)
2.3 More Information About Suicide Risk Factors
2.3.1 Having Mental Health Issues or a Mental Illness
Suicide is overrepresented in people with mental illness although most people with mental health conditions do not commit suicide. Impulsivity (particularly angry impulsivity) and disinhibition are strongly related to suicidal ideation and behaviors. Impulsivity is associated with bipolar disorder, substance abuse, and certain personality disorders as well as a history of early child abuse.
The odds for suicide in severe depression, schizophrenia, and bipolar disorder are approximately 3–10 times that of the general population, with a higher increased risk in males than females. However, keep in mind that despite these statistics, suicide does not occur in 95% to 97% of people with mental illness (Fosse et al., 2017).
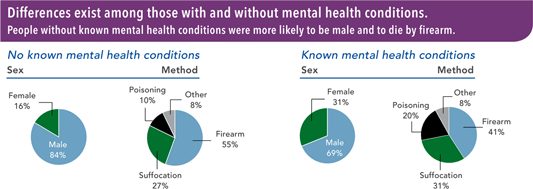
Source: CDC, 2018, June 7. Public domain.
2.3.2 Being a Survivor of Human Trafficking
Survivors of human trafficking and sexual violence are at increased risk of developing substance use disorders to cope with the traumatic experience and symptoms of post-traumatic stress disorder. For these individuals, treating the substance use disorder without addressing the PTSD is ineffective. PTSD symptoms frequently reappear when people stop using drugs or alcohol, leading to relapse. Survivors of human trafficking are at higher risk of suicidal ideation, suicide attempts, and suicide (Akee et al., 2024).
2.3.3 Having a Substance Abuse Disorder
People with substance use disorders often seek treatment at times when their substance use difficulties are at their peak—a vulnerable period that may be accompanied by suicidal thoughts and behaviors. Screening for suicidal thoughts and behaviors is important during intake and at specific points during the course of treatment. Compared with the general population, people being treated for alcohol use disorder are at about 10 times greater risk for suicide while people who inject drugs are at about 14 times greater risk (CSAT, 2015).
Abstinence should be a primary goal of any patient with a substance use disorder and suicidal thoughts or behaviors. For most patients, abstinence reduces risk, although some individuals remain at risk even after achieving this goal (CSAT, 2015).
Substance Use Disorder (SUD)
The presence of a substance use disorder in the past year is assessed based on criteria specified in the Diagnostic and Statistical Manual of Mental Disorders, 5th edition (DSM-5).
Drugs include marijuana, cocaine (including crack), heroin, hallucinogens, inhalants, methamphetamine, and any use of prescription stimulants, tranquilizers or sedatives, and pain relievers. The DSM-5 SUD criteria in 2021 for prescription drugs applied to people who used but did not misuse prescription drugs in the past year, in addition to people who misused them.
Source: SAMSHA, 2023 January 4
2.3.4 Experiencing Medical Issues and Physical Illness
Physical illness is a commonly overlooked risk factor for suicide. Medical patients often experience significant stressors, such as feeling like a burden to family, having concerns about potential loss of employment, cost of medical care, and feeling alone and isolated. These powerful stressors can increase suicidal thoughts in vulnerable patients, particularly individuals who have a history of suicidal thoughts or behaviors (Horowitz et al, 2018).
Co-morbid conditions may increase the likelihood that a suicide attempt becomes a completed suicide. For example, if a person with a chronic condition such as hepatitis C swallows a bottle of acetaminophen, they are likely to suffer severe liver damage. By the same token, a person with severe anemia may not survive a suicide attempt involving a significant loss of blood.
In patients without known mental health disorders, thoughts of suicide are important to assess. For example, the vulnerability for suicide risk among individuals with cancer is highest in the first month after diagnosis, highlighting the critical need for early detection (Horowitz et al, 2018).
2.3.5 Being an Immigrant, Asylum Seeker, Refugee, or ICE Detainee
For immigrants, asylum seekers, and refugees, suicidal ideation and behaviors arise from a complex interaction between vulnerabilities and risk factors. Temporary visa status, exposure to trauma, exposure to detention settings, and social isolation can contribute to increased risk. The term “lethal hopelessness” has been used to describe the increased suicide risk in asylum seekers due to the combination of limited access to mainstream services, financial support, culturally safe healthcare, and working rights (Ingram et al., 2022).
Immigrants migrating to an unfamiliar country lose links with their country of origin and often experience language barriers, a loss of status and social network, and a sense of inadequacy. Unemployment, financial problems, a sense of not belonging, and feelings of exclusion can negatively affect a person’s desire and ability to enter relationships with others. This can lead to depression, anxiety, post-traumatic stress disorder, and abuse of alcohol or drugs. Feelings of isolation, loneliness, and hopelessness can increase the risk of suicidal behaviors (Ratkowska & De Leo, 2013).
Roughly one in seven residents of Washington State is an immigrant, accounting for nearly 14% of the state’s population (AIC, 2020). From 2010 to 2016, Washington State admitted more than 16,000 refugees from 46 countries; 72% came from just five countries: Iraq, Myanmar, Somalia, Bhutan, and Ukraine (McDermott, 2016). In 2018, the top countries of origin for immigrants to the state were Mexico (23%), India (8%), China (7%), the Philippines (6%), and Vietnam (6%) (AIC, 2020).
Immigrant population has increased by 29% in Washington state during 2010 to 2021, with a larger increase in the immigrant group of naturalized citizens (37%). In 2021, the total immigrant population was 1,149,000 (Yen, 2023).
The migration of a family member poses a risk not only for immigrants but also for their families who remain in the country of origin. For example, the next of kin of Mexican immigrants in the U.S. were at greater risk of suicidal ideation and suicide attempts than Mexicans without a family history of emigration. Emigration of a close family member can weaken family ties, cause feelings of loneliness and insecurity, and increase the risk of suicide among family members who remain at home (Ratkowska & De Leo, 2013).
A study of Chinese immigrants in the U.S. found that older adults experiencing linguistic and cultural barriers rely heavily on their adult children to have access to healthcare and social services. Their social networks predominantly consist of family members, and they are isolated from the community. Their perceived burdensomeness to children and their social isolation can lead to suicidal ideation (Li et al., 2022).
Refugees are perhaps the most vulnerable group of immigrants: they are often fleeing war, torture, and persecution, and suffer with PTSD, depression, and anxiety. Lack of adequate preparation, the way in which they are received in the destination country, poor living conditions, and lack of social support and isolation add to these vulnerabilities. Refugees may also feel guilt for leaving loved ones at home or for their death. The sense of guilt, together with isolation and pathologic symptoms due to trauma, can be a strong risk factor for suicide (Ratkowska & De Leo, 2013).
For migrants in U.S. Immigration and Customs Enforcement (ICE) detention, mental healthcare has historically been substandard. ICE detainees suffer from higher rates of anxiety, depression, and post-traumatic stress disorder and are especially susceptible to stressors (Erfani et al., 2021).
Time spent in immigration detention is a particular post-migration stressor. Widespread failures to provide mental healthcare to detainees and critical medical staff shortages put ICE detainees at an increased risk for suicide. Between 2018 and 2020, the proportion of deaths in ICE detention attributed to suicide approximately doubled since cause of deaths were last described in 2015 (Erfani et al., 2021).
2.3.6 Being a Veteran
During the wars in Iraq and Afghanistan, military suicide rates increased and surpassed the rates for society at large. The Marines had had the highest proportional number of suicides compared to the other services followed by the Army. However, the rates in all the services have been increasing in recent years (DVA, 2022, September).
Why U.S. military personnel and veterans are at increased risk for suicide compared to civilians is the focus of ongoing research. They experience both military- and non-military-related trauma, such as combat-related experiences, military sexual assault, difficulty reintegrating into civilian life, and access to guns. Some have a history of childhood abuse and intimate partner violence. Military personnel and veterans also experience high rates of posttraumatic stress disorder, a known risk factor for both suicidal ideation and behaviors (Holliday et al., 2020).
Elevated suicide risk can endure well beyond military service, with veterans carrying a much greater risk for suicide than their civilian counterparts. Veterans have identified suicide as the most formidable challenge they face. Sadly, approximately 17 veterans die by suicide every day (DVA, 2021, September).
PTSD
Posttraumatic Stress Disorder (PTSD) can occur after someone goes through a traumatic event like combat, assault, or disaster. A person experiencing PTSD can feel unsafe, have upsetting memories, feel on edge, or have trouble sleeping.
Research looking specifically at combat-related PTSD in Vietnam era veterans suggests that the most significant predictor of both suicide attempts and preoccupation with suicide is combat-related guilt. Many veterans experience highly intrusive thoughts and extreme guilt about acts committed during times of war. These thoughts can often overpower the emotional coping capacities of veterans (Hudenko, Homaifar, and Wortzel, 2022).
PTSD has been found to be a risk factor for suicidal ideation for veterans of the wars in Afghanistan and Iraq. Even mild PTSD carries risk. Among these veterans, those with subthreshold PTSD* were 3 times more likely to report hopelessness or suicidal ideation than those without PTSD (Hudenko, Homaifar, and Wortzel, 2022).
*Subthreshold PTSD: a collection of symptoms that aren’t complete enough or severe enough to earn a PTSD diagnosis.
Veterans with PTSD who feel they have purpose and meaning in life have better outcomes than those who do not. Social support is associated with lower PTSD symptom severity in trauma-exposed individuals. Disrupted sleep is a core symptom of PTSD, and research demonstrates that cognitive-behavioral treatments that reduce insomnia and nightmares can reduce other symptoms of PTSD (DeBeer et al., 2016).
Depression
Major depressive disorder, which is highly comorbid with PTSD, independently increases risk for suicidal ideation and attempts. Among veterans who died from suicide in 2020, the prevalence of depression diagnoses was more than 35% (DVA, 2021, September).
The risk of suicide is greater in veterans who have been diagnosed with PTSD and/or major depressive disorder. Nearly a third of veterans with PTSD and/or major depressive disorder reported current suicidal ideation and 28% reported a lifetime suicide attempt. Greater purpose in life, curiosity, and optimism were inversely associated with suicidal ideation (Fogle et al., 2020).
2.4 Communication Preferences for Veterans and Service Members
Despite the investment of public resources to address suicide among veterans and service members, little is known about how they communicate suicidal ideations or what interventions they are willing to receive. A survey of communication and intervention preferences for veterans and service members found that nearly 90% of respondents indicated that they were willing to speak to someone when having thoughts of suicide. Most indicated that family members and military friends would be their primary outreach (Beatty et al., 2023).
Many participants were open to receiving resources, suicide-specific mental health treatment, and some sort of lethal means safety intervention. The age, marital status, and the status of participants significantly impacted what interventions they were willing to allow (Beatty et al., 2023).
Veterans and service members indicated they were far less likely to talk about their thoughts of suicide with non-military friends than military friends. Respondents were also considerably less likely to talk about their thoughts of suicide with the Veterans Crisis Line or National Suicide Prevention Line, chaplains, veteran service organizations, other healthcare providers, or their boss. About 10% stated that they would not trust talking with anyone about their thoughts of suicide (Beatty et al., 2023).
