The onset of dementia and its gradual progression often leads to changes in personality and behavior. Geriatrics specialists refer to these changes as behavioral and psychological symptoms of dementia (BPSD) or neuropsychiatric symptoms of dementia (NSP).
The Human Brain
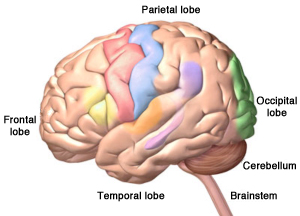
The four lobes of the cerebrum, plus the cerebellum and the brainstem. Alzheimer’s disease starts in the hippocampus, located in the temporal lobe. ©Zygote Media Group, Inc. Used with permission.
A symptom is a change in the body or the mind while a behavior is how we act, move, and react to our environment. Symptoms change as dementia progresses, often affecting behavior. For some people, symptoms can worsen quickly. For others, symptoms progress more gradually—over 10 to 20 years.
One way to describe the progression of Alzheimer’s disease, as well as other types of dementia, is in stages. Stages are usually described as mild, moderate, and severe or early, middle, and late. Even though disease progression differs from person to person, we nevertheless associate certain symptoms and behaviors with these stages. The type of dementia, along with a person’s underlying health, family support, and co-morbid conditions* can affect how fast and how far the dementia progresses from one stage to another.
*Co-morbid conditions: when someone has more than one disorder or illness at the same time.
2.1 Symptoms and Behavior Changes: Mild Dementia
The early or mild stage of dementia begins with mild forgetfulness, which might be the most obvious symptom at this stage, especially in Alzheimer’s disease. Logical thinking and judgment can be mildly affected, especially in certain types of dementia. These changes are thought to be related to the formation of plaques and tangles, beginning in the temporal lobes in and around the hippocampus.
Brain Changes in Mild Dementia
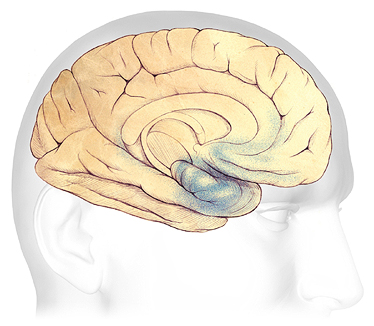
In the early stages of AD, before symptoms can be detected, plaques and tangles form in and around the hippocampus, an area of the brain responsible for the formation of new memories (shaded in blue). Source: The Alzheimer’s Association. Used with permission.
In the early stage of Alzheimer’s disease, as well as in other types of dementia, the first symptoms might be a little confusion and difficulty with complex, multi-step tasks. People naturally try to cover up mild confusion and friends, coworkers, and family members may not notice that something is changing. These changes can be frustrating and concerning for the person experiencing the first signs of cognitive change.
Even when symptoms are mild, a person’s behavior may begin to change, especially in Alzheimer’s disease. People with mild dementia often know something is wrong, which can cause depression, stress, anxiety, mood changes, and episodes of anger or aggressiveness. They still might be able to work, drive, and live independently, but they will begin to need some help from family or coworkers.
2.2 Symptoms and Behavior Changes: Moderate Dementia
As Alzheimer’s disease progresses from the mild to moderate stage, plaques and tangles spread forward to the areas of the brain involved with language, judgment, and learning. Spatial awareness*, and executive functions such as planning, judgment, and ethical thinking can be affected. Work and social life become more difficult and episodes of confusion increase. Many people are first diagnosed with Alzheimer’s disease in this stage.
*Spatial awareness: an awareness of where we are in relation to the things around us including distance, direction, and location.
Brain Changes in Moderate Dementia
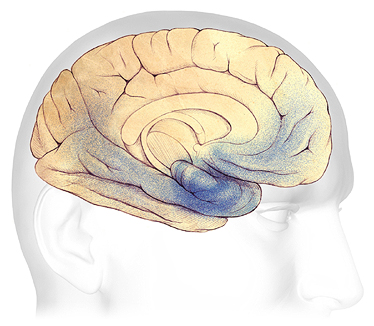
In mild to moderate stages, plaques and tangles (shaded in blue) spread from the hippocampus forward to the frontal lobes. Source: The Alzheimer’s Association. Used with permission.
In the moderate stage, behavior changes become more obvious to family members. Episodes of inappropriate behaviors such as cursing, kicking, hitting, and biting can occur. Some people may start to repeat questions over and over, call out, or demand your attention. Sleep problems, anxiety, agitation, and suspicion can develop.
A person with moderate dementia is often still able to walk. This is because the part of the brain that controls movement is not affected. If a person can still walk or if they can get around easily using a wheelchair, they might begin to wander. More direct monitoring is needed than during the early stage of dementia. People may no longer be safe on their own and caregiver responsibilities increase. This often increases stress, anxiety, and worry for family members and caregivers.
2.3 Symptoms and Behavior Changes: Severe Dementia
My mom is 96 years old and has pretty severe dementia. She lives at home with 24/7 care. If we put her in a nursing home, she would not survive. Loud noises, people that don’t know her needs and habits, boredom, loneliness—those things would drive her crazy. I’m sure she’d wander, yell, swear, shout, hit, and cry. At home she almost never does any of these things, but we work pretty hard to keep things quiet, warm, and steady for her.
Family Caregiver, Ft. Lauderdale, Florida
Brain Changes in Severe Dementia
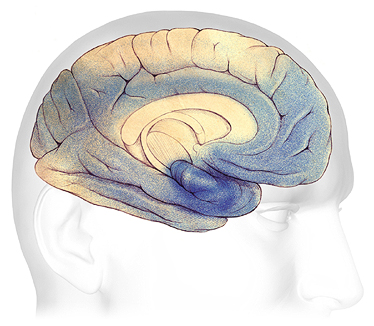
In advanced Alzheimer’s, plaques and tangles (shaded in blue) have spread throughout the cerebral cortex. Source: The Alzheimer’s Association. Used with permission
People with severe dementia lose most or all memory of recent events although they often remember events from long ago. They are easily confused, lose much of their ability to think logically and sequentially, and find decision-making very difficult. Speech, communication, and judgment are severely affected. Sleep disturbances are very common.
All sorts of challenging behaviors can occur in people with severe dementia—especially if caregivers and family members are untrained, easily frustrated, or highly stressed. Wandering, rummaging, or hoarding can occur. A person may become paranoid or have delusions or hallucinations. Screaming, swearing, crying, shouting, loud demands for attention, negative remarks to others, and self-talk are common. These outbursts are often triggered by frustration, boredom, loneliness, depression, cold or heat, loud noises, and pain.
2.4 Symptoms and Behavior Changes: End of Life
As a person with dementia approaches the end of their life, they may lose all memory—not just memory of recent events. They may be startled by loud noises and quick movements. They can no longer communicate their needs and desires using speech. At this stage, people can develop other illnesses and infections. They may experience agitation, psychosis,* delirium,** restlessness, and depression.
*Psychosis: loss of contact with reality.
**Delirium: a sudden, severe confusion that can be caused by infections, a reaction to medications, surgery, or illness.
At the end of life, people with dementia are often completely dependent on caregivers. They may refuse to eat, have difficulty swallowing fluids and medications, and will likely need close supervision for all activities of daily living. Weight loss, which may have been gradual over time, can rapidly increase.
A person with severe dementia may have medical complications that significantly increase the risk of acute conditions. One such condition is pneumonia, which is the most commonly identified cause of death among older adults who have Alzheimer’s or other dementias.
