[Unless otherwise cited, this section is taken from Patrick Berche, History of Measles, La Press Médicale, 2022.]
Measles is a morbillivirus, in the same family as distemper and rinderpest (a disease that afflicted domestic cattle and buffalo until it was eradicated in 2011). The current human measles virus adapted perfectly to humans from cattle around the 6th century BCE, though some scholars claim that a precursor of the disease began afflicting humans two centuries before that. The disease was widespread across Europe and Asia during the Middle Ages. Outbreaks were common in England and Scotland in the late 17th century.
3.1 History of Measles and Vaccine Development
Did You Know. . .
The genus Morbillivirus belongs to the virus family Paramyxoviridae, a group of enveloped viruses with non-segmented, negative strand RNA genomes. It contains viruses that are highly infectious, spread via the respiratory route, cause profound immune suppression, and have a propensity to cause large outbreaks associated with high morbidity and mortality in previously unexposed populations. In populations with endemic virus circulation, the epidemiology changes to that of a childhood disease and hosts that survive the infection normally develop lifelong immunity.
During the age of European colonial expansion, measles and smallpox led to high numbers of deaths among Indigenous populations. In 1529 (in what is now Cuba) measles killed two-thirds of the population that had previously survived smallpox. Two years later, half of the remaining population of Honduras succumbed to measles. In 1854, measles caused the deaths of 36,000 people out of a population of about 135,000.
In 1846, a Danish physician named Peter Ludwig Panum traveled to the Faroe Islands (in the North Atlantic) during a measles outbreak to study the disease. By tracing the index case for each village, he calculated the incubation period (10-12 days). His research disproved the “miasma theory,” which attributed diseases to bad air or foul smells, and posited that the disease was transmitted by something “imperceptible to the senses.” Panum noted that none of the older adults who had survived an epidemic that struck the island 60 years previously were ill. This supported a later finding that surviving measles confers lifelong immunity.
Over a hundred years later, in 1954, two scientists working for Boston Children’s Hospital, Thomas Chalmers Peebles and John Franklin Enders, went to a nearby elementary school that was suffering a measles outbreak. They took samples from a sick child, cultured them on a human kidney cell culture, and went on to lead a team that developed the vaccine that was approved in 1963.
Why Are We Seeing Measles Outbreaks? — Feb 2024 News [5:34]
Source: Dr. Paul Offit, Children’s Hospital of Philadelphia.
https://www.youtube.com/watch?v=Qu2AU7CRJRc&list=PLUv9oht3hC6Tzdut8u2aoJwdAyGEzDM0J&index=1
3.2 The Pathophysiology and Clinical Symptoms of Measles
The measles virus is transmitted by air as droplets infect the respiratory system. It is manifested in a widespread skin rash, typically starting at the hairline, then moving on to the face and neck and spreading downwards and outwards. It incubates for 10-12 days, with a rash setting in 7-21 days after exposure. It is communicable four days before through four days after the onset of the rash.
There are four stages of classic measles, which include incubation, prodrome (early signs indicating the onset of the disease), exanthem stage of rash, and recovery. In the incubation period, patients generally do not feel symptoms for 8 to 10 days and don’t know they have been infected.
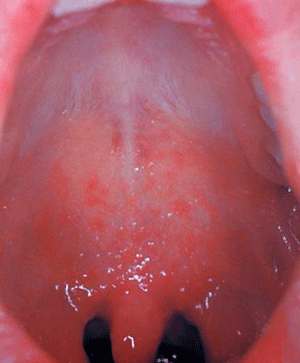
This patient presented with Koplik spots on palate due to pre-eruptive measles on day 3 of the illness. Source: CDC/PHIL.
The prodrome lasts from 2 to 8 days and includes the symptoms of fever, peaking as high as 105º F, followed by dry hacking cough, runny nose (coryza), and conjunctivitis, or pink eye (Gastañuduy, et al., 2024). These are known as the “three C’s” of classic measles infection. Red and white spots present on the mucous membrane of the mouth 1 to 2 days before the generalized body rash and are known as Koplik spots—identified by Henry Koplik, an American pediatrician, in 1896. On the palate, the spots look like grains of white sand on a hot red background. Koplik spots, which are specific to measles, generally appear about 48 hours before the rash appears.
Did You Know. . .
Koplik spots are unique to measles and no other medical condition has them. Identifying oral mucosal spots in the posterior of the oral cavity can be helpful in distinguishing measles from other childhood conditions with fever and rash.
The measles exanthem rash is characterized as a maculopapular rash beginning at the head and mouth and progressing downward and outward (confluence) to the chest, hands, and feet, and lasting for less than 1 week. It usually spares the palms and soles of the feet. Initially the lesions blanch but by days 3 to 4 they do not blanch and may create fine desquamation and peeling of hands and feet. The lesions and rash disappear in the same order they appeared. Additional symptoms include anorexia, diarrhea, malaise, and generalized lymphadenopathy as the body works to kill and rid itself of the bloodborne virus. If the rash continues after 48 hours, it is a signal of potential complications.
Measles Rash Seen on Light and Dark Skin


Left: Child with classic measles rash after 4 days. Right: Skin sloughing off of a child healing from measles infection. Source: CDC.
About 30% of patients will experience complications, the most common of which is pneumonia. Pneumonia is also the cause of most of the deaths, which are one or two in 1,000. Encephalitis and brain swelling can cause convulsions or long-term disabilities. Toxic encephalopathy may occur in 1 in 200 people and is a serious complication leading to death.
Nausea, vomiting, febrile seizures, anorexia, and complications from dehydration may also occur. Patients may develop photosensitivity and should protect their eyes from light for the duration of the illness. Infection of the optic nerve leading to blindness is one of the more serious complications. Thrombocytopenia, or low blood platelet count, also affects the blood’s ability to clot, which may cause bleeding risk.
Atypical measles is found in persons vaccinated by the inactivated killed measles vaccine (KMV) between 1963 and 1967, which sensitized but didn’t protect recipients against the virus. The resultant illness from exposure creates the same clinical symptoms but the rash seems to be limited to the wrist and ankles.
It is recommended that those who received the killed measles vaccine during those years receive the second MMR.
People who were vaccinated between 1968 and 1989 may have only received one dose of the vaccine, instead of the two doses that are currently recommended. These adults should be revaccinated, especially those in a high-risk category, like health care workers, college students, people with weakened immune systems, international travelers, and people who come in close contact with members of these demographics (Penn State Health News, 2025).
Symptoms of Similar Childhood Diseases | |||
|---|---|---|---|
Name(s) | Pathogen / Age of Onset | Signs/symptoms | Treatment |
Rubeola Also known as “Classic measles” or “Red measles” | Rubeola virus / Any age | Fever, coryza, cough, conjunctivitis (3 C’s), Koplik spots, spreading maculopapular rash from head to feet, anorexia, malaise | Supportive: antipyretics for fever, hydration, isolation Antibiotics if bacterial infection develops |
Rubella Also known as “3-day measles” | Rubeola virus / Any age | Same as rubeola without high fever and no Koplik spots. Resolves on own in 72 hours. Joint pain and lymphadenopathy | Supportive for fever and hydration |
Erythema infectiosum Also known as “Fifth’s disease” | Human Parvovirus B19 / 5–14 years | “Slapped cheek” appearance, lacy exanthema on face, arms, legs, trunk and dorsum of feet. Not contagious after fever breaks. Rash may last up to 40 days. | Supportive for fever and hydration |
Roseola Infantum Also known as “Sixth disease” | Herpes virus 6 / | URI symptoms Small pink, flat bumps on trunk and extremities, high fever when rash develops that can last up to 8 days. | Supportive for fever and hydration |
Coxsackie virus Also known as “Hand-foot-and-mouth disease” | Coxsackie virus / Any age | Inflammation of soft palate of mouth and papulovesicular exanthem of hands and feet. Drooling, fever, malaise, poor appetite from painful mouth sores. | Supportive for fever, pain and hydration. |
