In the previous section, we talked about different kinds of dementia. Each one has its own set of characteristics. A characteristic is a feature or quality you would expect to see in a disease. You now know that one characteristic of frontal-temporal dementia is that it starts at an earlier age than Alzheimer’s.
Symptoms and Behavior Changes by Stages
A symptom is a change in the body or the mind. Loss of memory is a symptom of dementia. Changes in judgment and logical thinking are also symptoms of dementia.
Behavior is how we act, move, and react to our environment. Anger and happiness are behaviors.
Symptoms and behaviors change as dementia gets worse. For some people symptoms can get worse really fast. For others, symptoms may get worse gradually—over 10 to 20 years.
Alzheimer’s disease occurs along a continuum:
- Pre-clinical
- Mild cognitive impairment due to Alzheimer’s disease (MCI)
- Mild dementia due to Alzheimer’s disease
- Moderate dementia due to Alzheimer’s disease
- Severe dementia due to Alzheimer’s disease
Alzheimer’s Association, 2023
A good way to understand symptoms and behaviors is to look at how things change in the pre-clinical, MCI, mild, moderate, and severe stages of dementia.
Symptoms and Behaviors in Preclinical Disease and MCI Due to AD
In the pre-clinical phase, there are measurable changes in the brain but no symptoms (such as memory loss). At this stage, the brain is able to compensate for any early changes. With mild cognitive impairment due to Alzheimer’s disease, there are measurable brain changes plus subtle changes in memory, language, and thinking (Alzheimer’s Association, 2023).
Symptoms and Behaviors in Mild Dementia
The early or mild stage of dementia begins with mild forgetfulness, especially memories of recent events. Forgetfulness might be the most obvious symptom at this stage, especially in Alzheimer’s disease.
Logical thinking and judgment are mildly affected, especially in frontal-temporal dementia. At this stage, you might notice a little confusion with complex tasks that take many steps to complete. People try to cover up mild confusion so friends, coworkers, and family might not notice that something is wrong.
Even when symptoms are mild, people’s behavior begins to change, especially in Alzheimer’s disease. People with mild dementia know something is wrong. They may begin to worry about the future or feel stress and anxiety. They may get depressed as they struggle with changes in their thinking. Mood changes might be most obvious in a person with vascular dementia.
People with mild dementia may occasionally become angry or aggressive. They might have difficulty making decisions. They will ask for help more often. They still might be able to work, drive, and live independently, but they will begin to need more help from family or coworkers.
Changes in the Brain During Mild Dementia
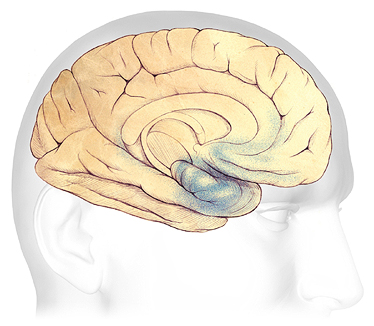
In the earliest stages of Alzheimer’s disease, before symptoms can be detected with current tests, damage (shaded in blue) begins in the areas of the brain involved in:
- Learning and memory
- Thinking and planning
Source: Courtesy of The Alzheimer’s Association. Used with permission.
Symptoms and Behaviors in Moderate Dementia
In the moderate stage of dementia, people are more forgetful. Confusion also gets worse. Speech and communication are obviously affected. Judgment and logical thinking are much worse than in the early or mild stage.
Because of memory problems and confusion, caregivers must take over tasks that the person with dementia was able to do in the past. In this stage, independent travel, work, and keeping track of personal finances are probably no longer possible.
In the moderate stage, behavior changes are much more obvious. Inappropriate behaviors such as cursing, kicking, hitting, and biting are not uncommon. Some people may repeat questions over and over, call out, or demand your attention. Sleep problems, anxiety, agitation, and suspicion can develop.
A person with moderate dementia is often still able to walk. This is because the part of the brain that controls movement is not damaged. If a person can still walk or if they can get around easily in a wheelchair, they might begin to wander. More direct monitoring is needed than during the early stage of dementia.
During this stage, people are no longer safe on their own. Caregiver responsibilities increase. This causes stress, anxiety, and worry among family members and caregivers. Surprisingly, many people with dementia may not be diagnosed until they reach this stage.
Changes in the Brain During Mild to Moderate Dementia
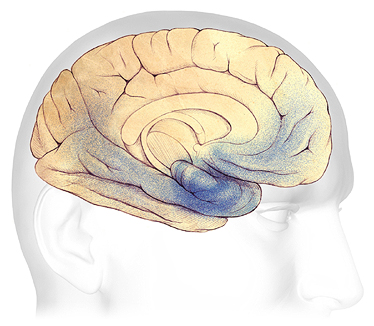
In mild to moderate stages, the parts of the brain involved with memory, thinking, and planning become more affected (shaded in blue).
Work or social life becomes more difficult. Confusion increases, and many people with Alzheimer’s are first diagnosed in this stage.
Damage spreads to the areas of the brain involved with:
- Speaking and understanding speech
- Logical thinking
- Safety awareness
Source: Courtesy of The Alzheimer’s Association. Used with permission.
Symptoms and Behaviors in Severe Dementia
My mom is 96 years old and has pretty severe dementia. She still lives at home because we provide 24/7 care. If we put her in a nursing home, I think she would go down pretty fast. Loud noises, too many people around, people that don’t know her needs and habits, boredom, loneliness—all those things would drive her crazy. At this stage I think she’d be really hard to handle in a nursing home. She’s kind of stubborn and independent and I’m sure she’d wander, yell, swear, shout, hit, and cry. At home she doesn’t do any of these things (well, a little now and then) but we work pretty hard to keep things quiet, warm, and steady for her.
Family Caregiver, Sarasota, Florida
People with severe dementia lose all memory of recent events although they may still remember events from long ago. They are easily confused and are unable to make decisions. Speech, communication, and judgment are severely affected. They cannot think logically. Sleep disturbances are very common.
All sorts of challenging behaviors occur in people with severe dementia. Screaming, swearing, crying, shouting, loud demands for attention, negative remarks to others, and self-talk are common. Outbursts can be triggered by boredom, loneliness, depression, cold or heat, loud noises, and pain.
Wandering, rummaging, or hoarding can occur. A person may become paranoid or have delusions or hallucinations.
In the severe stage, independence is lost. Around-the-clock care is needed. People at this stage need assistance with eating, bathing, walking, dressing, and all other daily living activities (ADLs).
Changes in the Brain During Severe Dementia
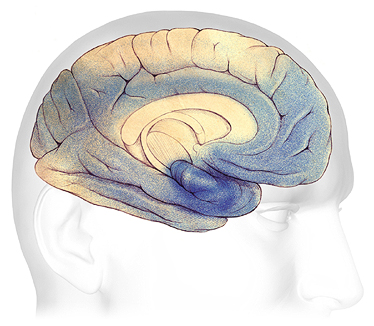
In advanced Alzheimer’s disease, most of the surface of the brain is severely damaged (shaded in blue). Individuals lose their ability to communicate, to recognize family and loved ones, and to care for themselves.
Source: Courtesy of The Alzheimer’s Association. Used with permission.
Symptoms and Behaviors at the End of Life
As people with dementia approach the end of life they may lose all memory—not just memory of recent events. The damage to their brains is so severe that they are in a constant state of confusion. They are startled by loud noises and quick movements. They can no longer communicate their needs and desires using speech.
At this stage, people can develop other illnesses and infections. They may experience agitation, psychosis*, delirium**, restlessness, and depression.
*Psychosis: loss of contact with reality.
**Delirium: a sudden, severe confusion that can be caused by infections, a reaction to medications, surgery, or illness.
At the end of life, people with dementia are completely dependent on caregivers. They may be unable to eat, swallow fluids, or move without help. Dementia becomes so severe that people may become bedridden.
Most commonly, people with Alzheimer’s disease or other types of dementia die of pneumonia or from complications of fractures, especially hip fractures.
