Each year, we must decide whether to get vaccinated against the flu. Many of us get the vaccine without a second thought, while a significant percentage of Americans either choose not to get vaccinated or simply never get around to it.
Vaccine Hesitancy
For many individuals, the health benefits associated with vaccination is not a sufficient reason to embrace vaccination wholeheartedly. They doubt the benefits of vaccines, worry over their safety, and question the need for them, an attitude referred to as vaccine hesitancy. An attitude of hesitancy differs from an action of vaccine refusal. Even those who are vaccinated can harbor hesitancy toward certain aspects of vaccination (Yaqub et al., 2014).
While coverage rates are helpful for identifying those who reject, it does little to help us understand hesitant attitudes, their origins, and how to change them. Maintaining high coverage rates helps to ensure that vaccination benefits are delivered widely, but the very act of delivering wide-scale vaccination can make vaccines “victims of their own success.” As the ravages of disease become less familiar to people, it may become more challenging to articulate the desirability of vaccination (Yaqub et al., 2014).
Reasons for Refusing the Flu Vaccine
It is certainly reasonable to ask why so many people, both in and out of healthcare, decide not to get vaccinated against influenza each year. Studies that investigate why a segment of the population does not accept vaccination have highlighted lack of knowledge, misperceptions, and distrust of vaccines. Ironically, another reason cited is a low perceived risk because the incidence has declined as a result of vaccination programs (Herzog et al., 2013).
Surveys in Europe and the United States have found that low seasonal vaccination coverage rates are influenced by inadequate (or no) recommendation by general practitioners, poor public awareness of influenza and influenza vaccines, a lack of proactive reminder systems, and a fear of needles (Blank et al., 2012).
Examining misconceptions about vaccination provides some context about why many people forgo the influenza vaccine each year:
- Fear that the immune system will be “overloaded” by vaccines, especially in children.
- The belief that many common diseases have disappeared and it is no longer necessary to vaccinate against them.
- The belief that more vaccinated than unvaccinated people get sick.
- The belief that hygiene and better nutrition are responsible for the reduction in disease rates, not vaccination.
- The belief that natural immunity is better than vaccine-acquired immunity. (The College of Physicians of Philadelphia, 2016)
When looking at the reasons why a significant percentage of healthcare providers in the United States say they do not intend to get a seasonal flu vaccine, the most commonly reported reason was that they do not think the flu vaccine works. Other reasons included thinking they do not need a flu vaccine, fear of getting sick, fear of side effects from vaccination, being allergic to the vaccine, and thinking that flu vaccination is not good for you.
Main Reason Reported for Not Getting the Flu Vaccine Among Healthcare Personnel Not Planning to Get One in 2016–2017 Internet Panel Survey, November 2016, USA
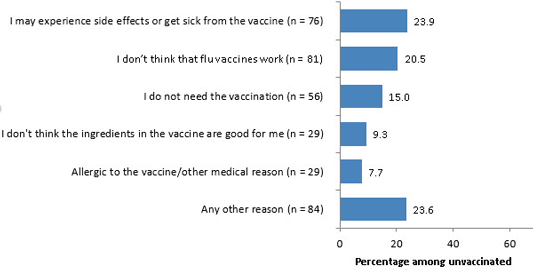
Source: CDC, 2016.
Recently, researchers from the European Centre for Disease Prevention and Control (ECDC) analyzed the results of a study conducted by vaccine producers, which looked at the costs and benefits of influenza vaccination. Cautioning that the data on vaccine coverage, disease burden, and health costs are imprecise, the analysts nevertheless agreed that it is important to understand the reasons for low vaccine coverage in the 27 European countries included in the study (Ciancio & Rezza, 2014). The reasons for low vaccine coverage echo many of the findings in earlier studies:
- Vaccine hesitancy in healthcare workers and in the population
- Lack of confidence in vaccine effectiveness and safety
- Complex vaccine recommendations
- Short vaccine delivery window
- Lack of resources
Reasons for Accepting the Flu Vaccine
When I first started work as a nurse, I never got a flu shot. If I got the flu, I went to work even though I was sick. One year I got the flu shot on a Friday morning and was sick as a dog by the evening. Now I know that I already had the flu when I got the shot—back then I blamed it on the vaccine and didn’t get a shot for several more years. One year I got the flu, missed several days of work, and coughed my lungs out for almost two weeks. After that I thought, this is ridiculous, the flu vaccine will stop all of this. It was a no-brainer. Now I get a shot every year.
ER Nurse, California, 2020
There are many good reasons for healthcare workers to get a flu vaccine, not least of which is they are less likely to become ill themselves and much less likely to pass the virus on to their patients and families. Among healthcare personnel who received the flu vaccine in 2016, protecting themselves from flu was the most common reason reported for receiving the flu vaccination. Employer requirement for flu vaccination was the second most commonly reported reason why vaccinated healthcare providers decided to get the flu vaccination (CDC, 2016).
Main Reason Reported for Getting the Flu Vaccine Among Healthcare Personnel (n=1,378) Internet Panel Survey, November 2016, USA
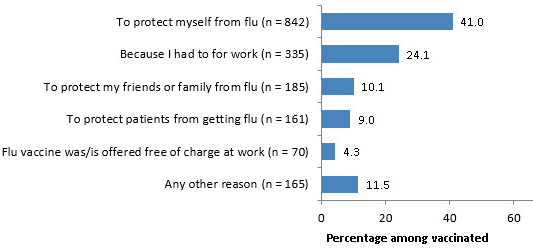
Source: CDC, 2016.
During the 2009–2010 H1N1 influenza pandemic in France, Germany, and Mexico, the most common reason given to be vaccinated for A/H1N1 pandemic influenza was a physician’s advice or recommendation. In the United States, media advertising was the most important motivating factor, although a physician’s advice was nearly as important (Blank et al., 2012).
Influenza Vaccination Programs
Influenza vaccination programs in healthcare facilities are most successful when they are multifaceted. Successful programs focus on the following:
- Full, visible leadership support with the expectation for vaccination fully and clearly communicated to all healthcare personnel
- Provision of adequate resources and support for the healthcare personnel vaccination program
- Inclusion of all practices necessary to reduce the spread of influenza in healthcare settings, including patient isolation, use of personal protective equipment, applying hand and respiratory hygiene and cough etiquette, and restriction of ill visitors and ill healthcare personnel (NVAC, 2013)
In one innovative program initiated by the University of Pittsburgh Medical Center, 14 long-term care facilities ceded control of vaccination-related policies and processes to a regional pharmacy. The facilities worked collaboratively with the pharmacy to implement and enforce standardized policies and processes to boost influenza vaccination rates among facility workers. This policy change significantly increased worker vaccination rates in participating facilities, enabling all facilities to reach the Healthy People 2010 goal of vaccinating 60% of workers in long-term care settings and several facilities to exceed the Healthy People 2020 goal of vaccinating 90% (AHRQ, 2014).
When receiving the influenza vaccine is a condition for employment, vaccination rates can approach 100%. During the 2010–2011 influenza season, CDC found that approximately 13% of healthcare personnel reported that their employers required influenza vaccination as a condition of employment. Among this group, vaccination coverage was 98.1%, compared with 58.3% among those without an employer requirement (NVAC, 2013).
A national survey of acute care hospitals found that 55.6% of the hospitals surveyed had implemented an institutional requirement, but that vaccination coverage rates increased most significantly in hospitals that also enforced consequences for vaccine refusal. Consequences ranged in severity from mandatory masking to employee termination for noncompliance (NVAC, 2013).
