THIS COURSE IS RETIRED. Do not try to take this course. We plan to update the course soon.
If you reside in Washington State, please click on the course link to access WA HIV/AIDS, 7 units or WA HIV/AIDS, 4 units.
Authors:
Tracey Long, PhD, RN, APRN
Lauren Robertson, BA, MPT
JoAnn O’Toole, RN, BSN
Susan Walters Schmid, PhD
Contact hours: 7
AOTA CEUs: 0.7
Expiration date: November 23, 2023
Course price: $49
Course Summary
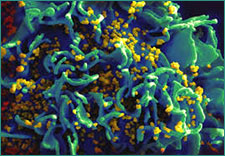
This course on HIV covers HIV origin and epidemiology, transmission precautions and infection control, testing and counseling, clinical manifestations and treatment, legal and ethical issues, and psychosocial issues.
Target Audience
Nurses, nurse practitioners, advanced practice nurses, physical therapists, physical therapy assistants, occupational therapists and occupational therapy assistants*.
*If you are an OT or OTA, you may need the following information for relicensure:
![]() ATrain Education is an AOTA Approved Provider of professional development. Approved provider #6558. This distance learning-independent is offered at 0.7 CEUs, introductory, Foundational Knowledge. The assignment of AOTA CEUs does not imply endorsement of specific course content, products, or clinical procedures by AOTA.
ATrain Education is an AOTA Approved Provider of professional development. Approved provider #6558. This distance learning-independent is offered at 0.7 CEUs, introductory, Foundational Knowledge. The assignment of AOTA CEUs does not imply endorsement of specific course content, products, or clinical procedures by AOTA.
Criteria for Successful Completion
Study the course material, achieve a score of 80% or higher on the post test (the post test can be repeated if a learner scores less than 80%), complete the course evaluation, and pay where required. No partial credit will be awarded.
Accreditation
To find specific accreditations or approvals, click here.
Conflict of Interest/Commercial Support Disclosure
The planners and authors of this learning activity have declared no conflicts of interest, vested interest, or financial relationship that may influence the content of this activity. All information is provided fairly and without bias.
ATrain Education, Inc. received no outside financial or commercial support in the preparation, presentation or implementation of this learning activity and has no affiliation with any company whose products or services are mentioned in this activity.
Course Objectives
When you finish this course you will be able to*:
- Discuss the origin and epidemiology of HIV in the United States.
- Describe transmission, infection control, and prevention of HIV.
- Outline the common testing and counseling requirements for HIV-infected individuals.
- Characterize the clinical manifestations, opportunistic infections and treatment options of HIV/AIDS.
- Identify the legal and ethical issues associated with HIV.
- Discuss the main psychosocial issues facing HIV-infected people and their caregivers.
- Identify global and national resources for healthcare professionals and clients with HIV.
*Please note: attainment of course objectives will be assessed in the course evaluation.