The brain is a communications center consisting of billions of neurons, or nerve cells. It is the most complex organ in the body. This three-pound mass of gray and white matter is at the center of all human activity—you need it to drive a car, to enjoy a meal, to breathe, to create an artistic masterpiece, and to enjoy everyday activities. The brain regulates your body’s basic functions; it enables you to interpret and respond to everything you experience and shapes your thoughts, emotions, and behavior (NIDA, 2018).
Networks of neurons pass messages back and forth among different structures within the brain, the spinal cord, and the nerves in the rest of the body (the peripheral nervous system). These nerve networks coordinate and regulate everything we feel, think, and do (NIDA, 2018). Dementia interrupts the efficient function of these networks, affecting every aspect of a person’s life.
Alzheimer’s disease and other types of dementia damage the brain. The most significant and obvious damage occurs in the critically important part of the brain called the cerebrum. The cerebrum fills up most of our skull and is divided into four lobes:
- Frontal lobes: reasoning, judgement, motor control, planning, decision-making
- Temporal lobes: memory and emotion, hearing, language
- Parietal lobes: sensation, touch, temperature, pressure, pain
- Occipital lobes: visual processing, depth, distance, location of objects
The Human Brain
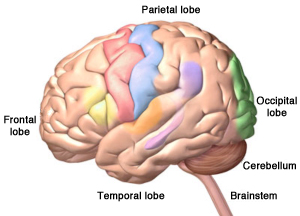
The four lobes of the cerebrum, plus the cerebellum and the brainstem. Alzheimer’s disease starts in the hippocampus, located in the temporal lobe. ©Zygote Media Group, Inc. Used with permission.
The cerebrum allows us to think, form memories, communicate, make decisions, plan for the future, and act morally and ethically. It also controls our emotions, helps us make decisions, and helps us tell right from wrong. The cerebrum also controls our movements, vision, and hearing.
When dementia strikes, brain cells in the cerebrum begin to shrink and die. As the damage progresses, brain cells are no longer able to communicate with one another as well as they did in the past. Not surprisingly, as more and more brain cells are damaged, connections are lost, pathways are disrupted, and eventually people with dementia lose many brain functions.
Because the right and left sides of each lobe differ in function, the location of the deterioration is important to understand. For example, damage in the left frontal and temporal lobes can affect the so-called language centers, causing difficulties with speech and language comprehension, while damage to the right hemisphere can cause problems with spatial perception and identifying objects by touch.
The parietal lobes provide another example of the differences between the right and left sides of this part of the brain. Several portions of the parietal lobe are important to language and visuospatial processing; the left parietal lobe is involved in symbolic functions in language and mathematics, while the right parietal lobe is specialized to process images and interpretation of maps (i.e., spatial relationships) (Lumen Learning, n.d.).
it is easy to exaggerate the differences between the functions of the left and right hemispheres; both hemispheres are involved with most processes. Additionally, neuroplasticity (the ability of a brain to adapt to experience) enables the brain to compensate for damage to one hemisphere by taking on extra functions in the other half, especially in young brains (Lumen Learning, n.d.).
Hemispheres of the Brain
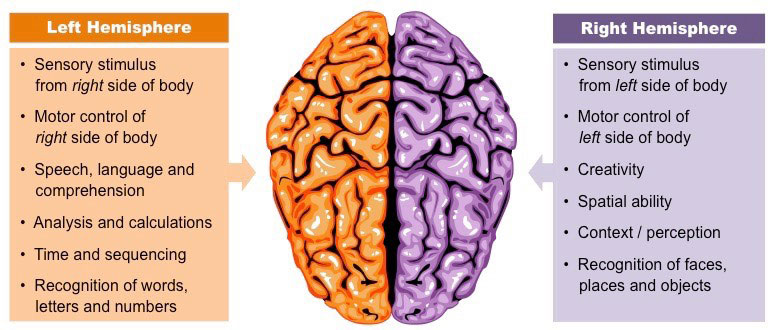
Source: Cornell, B. 2016. BioNinja. Reprinted by permission.
In addition to the cerebrum, the human brain has two other important parts: the cerebellum and the brainstem. Touch the back part of your head just below the occipital lobes. The cerebellum is right there. It is involved with coordination and balance.
Three Main Sections of the Human Brain
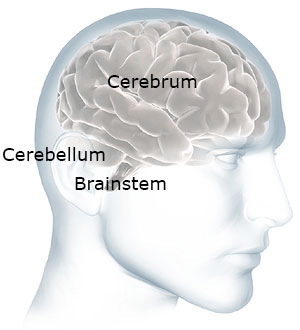
The cerebellum and brainstem are at the back of your head below the cerebrum. Source: NIH. Used with permission.
Now move your hand a little down and stop before your get to your spine. The brainstem is right there—at the back of the head, above your spine. It connects the brain to the spinal cord. The brainstem oversees automatic functions such as breathing, digestion, heart rate, and blood pressure. Although it is possible for the brainstem and cerebellum to be damaged by stroke or traumatic injury, they are generally not affected by dementia.
Defining Dementia
Dementia is a collective name for the progressive, global deterioration of the brain’s executive functions. Dementia occurs primarily in later adulthood and is a major cause of disability in older adults. Although almost everyone with dementia is elderly, dementia is not considered a normal part of aging.
Alzheimer’s disease is the most common type of dementia and is responsible for 60% to 80% of all cases. AD typically starts in an area of the brain called the hippocampus—the part of the brain responsible for new, short-term memories. The hippocampus is part of the brain’s limbic system and is responsible for the formation of new memories, spatial memories and navigation, and is also involved with emotions.
Damage to the hippocampus can cause a person with dementia, particularly someone with Alzheimer’s disease, to forget something that happened just a moment ago. Although most types of dementia start in one part of the brain, eventually the entire brain will be affected.
Alzheimer’s disease isn’t the only cause of dementia and, unfortunately, there is no way to know for sure what type of dementia a person has. Early diagnosis remains a key focus and goal of research.
Diagnosis of AD is most often based on a combination of medical history and detailed physical, neurologic, and neuropsychological exams. Brain imaging can be used but early preclinical dementia is difficult to diagnose accurately using these methods. In recent years, a number of soluble components in cerebrospinal fluid (CSF) and blood have been identified as potential, useful biomarkers* for AD (DeMarshall et al., 2019).
*Biomarkers: A measurable substance that may indicate the presence of a particular biologic state, a clinical disease, an environmental exposure, or disease susceptibility.
Measuring biomarkers for brain diseases in blood is the focus of intense research although there are a number of challenges. Because of the blood-brain barrier, biomarkers are generally present at relatively low concentrations in blood taken from the brain. In addition, some biomarkers related to AD pathology are expressed in non-cerebral tissues, which may confound their measurement in the blood. Blood may also contain antibodies, which can give falsely high or low results. This is less of a problem in CSF because antibody levels in CSF are much lower. Finally, the biomarker of interest may be degraded by various substances in blood plasma (Zetterberg & Burnham, 2019).
Recently, a blood test has been developed that measures a specific variant of tau protein in an ordinary blood plasma sample. The test measures the presence of the P-tau181 variant, using a method called Single Molecule Array (Simoa). P-tau181 has long been measured in CSF and is seen in advanced positron emission tomography (PET) scans. But both of these methods are expensive and not universally available and therefore not practical in primary care settings (Gustafsson Kubista, 2020).
There is potential to use this blood test to identify Alzheimer’s in its early stage when cognitive impairment is mild. This may provide primary care practitioners the ability to evaluate and treat people early in the disease rather than when symptoms are so obvious that they show up during cognitive testing.
Symptoms differ little among the types of dementia. It is good to know the difference to help you understand why someone is acting the way they are. Characteristics of Alzheimer’s dementia will be described in module 2.
Frontal-Temporal Dementia
Look at the picture of the brain below. Put your hand on your forehead. The part of your brain just behind your forehead is called the frontal lobe. Now slide your fingers from the front to the side of your head (your temple). This part of the brain is called the temporal lobe.
Lobes of the Brain
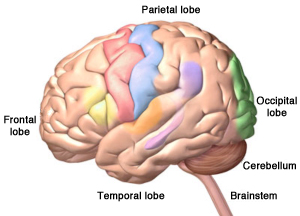
Damage to the brain’s frontal and temporal lobes causes forms of dementia called frontotemporal disorders. ©Zygote Media Group, Inc. Used with permission.
There is a type of dementia that affects this part of the brain. It is called frontal-temporal dementia. It is thought to be the most common type of dementia in people under the age of 60 and is responsible for 5% to 10% of all cases of dementia. It’s not nearly as common as Alzheimer’s and usually starts at a much younger age.
We use the front part of our brain to make decisions, to tell right from wrong, to control our emotions, and to plan for the future. Someone with dementia in this part of the brain will have poor judgment and lose the ability to tell right from wrong. They also have less control over their behavior.
So instead of losing short-term memory like people with Alzheimer’s disease, a person with frontal-temporal dementia might start doing things that are confusing to their friends and family. They might steal, even though they have never stolen in the past. They might make inappropriate sexual remarks or engage in inappropriate sexual behaviors, even though they have never done these things in the past.
Frontal-temporal dementia is usually categorized under three subtypes:
- Behavior variant frontotemporal dementia (bvFTD)—changes in personality and behavior that can affect people in their early 50s and 60s. Affects judgement, empathy, foresight, and planning.
- Primary progressive aphasia (PPA)—usually begins before the age of 65. Affects language skills, reading, writing, and comprehension.
- Disturbances of motor function, muscle weakness or wasting, without behavioral or language problems. (Alzheimer’s Association, 2020c)
Vascular Dementia
Vascular dementia is a general term used to describe changes in cognition resulting from impaired blood flow to the brain. It can be caused by a stroke or a series of small strokes or any condition that causes brain damage or reduces blood flow to the brain. Factors that increase the risk of heart disease such as diabetes, high blood pressure, high cholesterol, and smoking also increase the risk of developing vascular dementia. You might have cared for more than one client with vascular dementia because many older adults have high blood pressure that isn’t under good control.
Vascular dementia is responsible for 20-30% of all cases of dementia. Generally, vascular dementia doesn’t affect memory as much (or in the same way) as Alzheimer’s, at least in its early stage. Symptoms are related to the part of the brain experiencing reduced blood flow.
Vascular dementia can cause mood changes that are stronger than the mood changes you might see in someone with Alzheimer’s. It can also affect judgment—but not as strongly as in someone with frontal-temporal dementia. It can be difficult to differentiate vascular dementia and Alzheimer’s dementia because they can occur together. Cognitive changes can be gradual or occur in noticeable steps downward from a person’s previous level of function.
Lewy Body Dementia (LBD)
Lewy body dementia is a spectrum of disorders rather than a single diagnosis. LBD is less common than Alzheimer’s dementia, but more common than frontal-temporal and vascular dementia.
Lewy Body
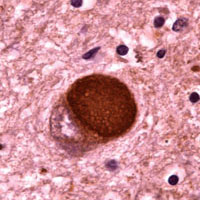
Microscopic image of a Lewy body. Courtesy of Carol F. Lippa, MD, Drexel University College of Medicine. Source: Alzheimer’s Disease Information and Referral Center.
There are two types of LBD: dementia with Lewy bodies and Parkinson’s disease dementia, which share a common etiology. Symptoms are caused by the buildup of Lewy bodies—accumulated bits of alpha-synuclein protein—inside the nuclei of neurons in areas of the brain that control certain aspects of memory and motor control. These unwanted molecules (Lewy bodies) can become scattered throughout the brain. Symptoms can include:
- Disturbances of movement (slowness of movement, rigidity, shuffling gait, tremors, difficulties with balance)
- Cognition decline (fluctuations in concentration, alertness, and attention)
- Behavioral changes (mood fluctuation, depression, anxiety, apathy, hallucinations, delusions)
- Sleep disturbances (daytime sleepiness, restless leg syndrome, difficulties awakening, acting out dreams, falling out of bed)
- Autonomic dysfunction (constipation, urinary incontinence, sexual dysfunction, difficulty regulating blood pressure and temperature, low blood pressure)
In Parkinson’s disease dementia, movement deficits are the first symptoms to appear. This can include festinating gait (shuffling), balance problems, muscle rigidity, resting tremors, bradykinesia (slow movement), and loss of facial expressiveness.
In general, memory is less affected than in Alzheimer’s disease, at least at first. But hallucinations, visuospatial changes, fluctuation in cognitive abilities, and sudden confusion can be present. These symptoms may come and go throughout the day.
Dementias and Their Characteristics | |
|---|---|
Type of dementia | Characteristics and symptoms |
Alzheimer’s disease (AD) 60%–80% of cases |
|
Frontal-temporal dementia 5%–10% of cases, prevalence thought to be underestimated |
|
Vascular dementia 20%–30% of cases |
|
Dementia with Lewy bodies ~5%–10% of cases |
|
How Dementia Affects the Brain
Dementia changes the entire brain. In Alzheimer’s disease, nerve cells in the brain die and are replaced by abnormal proteins called plaques and tangles. As the nerve cells die, the brain gets smaller. Over time, the brain shrinks, affecting nearly all its functions.
Normal Brain Contrasted with AD Brain
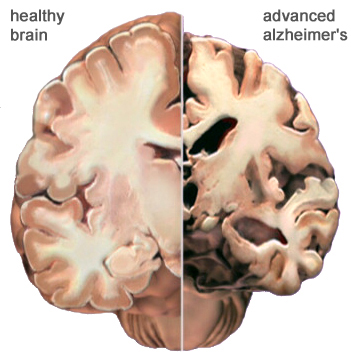
A view of how Alzheimer’s disease changes the whole brain. Left side: normal brain; right side, a brain damaged by advanced AD. Source: Courtesy of The Alzheimer’s Association. Used with permission.
Alzheimer’s disease usually affects memory and emotional control before other symptoms are obvious. Other types of dementia, because the damage is to another part of the brain, will have different symptoms. Although dementia can start in one part of the brain, eventually it will affect the entire brain.
Normal Age-Related Changes
We all experience physical and mental changes as we age. Some people become forgetful when they get older. They may forget where they left their keys. They may also take longer to do certain mental tasks. They may not think as quickly as they did when they were younger. These are called age-related changes. These changes are normal—they are not dementia.
Age-related changes don’t affect a person’s life very much. Someone with age-related changes can easily do everything in their daily lives—they can prepare their own meals, drive safely, go shopping, and use a computer. They understand when they are in danger and continue to have good judgment. They know how to take care of themselves. Even though they might not think or move as fast as when they were young, their thinking is normal—they do not have dementia.
The table below describes some of the differences between someone who is aging normally and someone who has dementia.
Differences between Normal Aging and Dementia | |
|---|---|
Normal aging | AD or other dementia |
Occasionally loses keys | Cannot remember what a key does |
May not remember names of people they meet | Cannot remember names of spouse and children—don’t remember meeting new people |
May get lost driving in a new city | Get lost in own home, forget where they live |
Can use logic (for example, if it is dark outside it is night time) | Is not logical (if it is dark outside it could be morning or evening) |
Dresses, bathes, feeds self | Cannot remember how to fasten a button, operate appliances, or cook meals |
Participates in community activities such as driving, shopping, exercising, and traveling | Cannot independently participate in community activities, shop, or drive |
In some older adults, memory problems are a little bit worse than normal age-related changes. When this happens, the person has mild cognitive impairment, also called MCI.
Mild cognitive impairment isn’t dementia. A large percentage of people with MCI experience personality changes. They also have a little more difficulty than is normal with thinking and memory. For some people, mild cognitive impairment gets worse and develops into dementia, but this doesn’t happen with everyone.
Dementia 101: Other Causes of Dementia; Teepa Snow [5:49]
http://teepasnow.com/resources/teepa-tips-videos/dementia-101/
Diagnostic Guidelines
Diagnosis of Alzheimer’s disease and other types of dementia is based on symptoms; no test or technique that can diagnose dementia. To guide clinicians, in 2011 the National Institute on Aging and the Alzheimer’s Association (NIA-AA) published updated diagnostic guidelines, which are intended to provide a deeper understanding Alzheimer’s disease than earlier guidelines. The 2011 guidelines:
- Recognize that Alzheimer’s disease progresses on a spectrum with three stages: (1) an early, preclinical stage with no symptoms; (2) a middle stage of mild cognitive impairment; and (3) a final stage marked by symptoms of dementia. Cognitive decline is gradual and progressive.
- Expand the criteria for Alzheimer’s dementia beyond memory loss as the first or only major symptom and recognize that other aspects of cognition, such as word-finding ability or judgment, may become impaired first. Other cognitive changes can include changes in:
- Episodic memory
- Executive functioning
- Visuospatial abilities
- Language functions
- Personality and/or behavior
- Reflect a better understanding of the distinctions and associations between Alzheimer’s and non-Alzheimer’s dementias, as well as between Alzheimer’s and disorders that may influence its development, such as vascular disease, delirium, or stroke.
- Recognize the potential use of biomarkers—indicators of underlying brain disease—to diagnose Alzheimer’s disease. However, the guidelines state that biomarkers are almost exclusively to be used in research rather than in a clinical setting. (National Institute on Aging, 2020)
Since the publication of the 2011 guidelines, researchers have increasingly come to
- Understand that cognitive decline in AD occurs continuously over a long period, and that
- Progression of biomarker measures* is also a continuous process that begins before
- Symptoms are evident. The disease is now regarded as a continuum rather than three distinct clinically defined stages. (Jack et al., 2018)
*β amyloid deposition, pathologic tau, and neurodegeneration neuronal injury.
A 2018 update of the 2011 NIA–AA diagnostic guidelines added a “numerical clinical staging scheme.” This staging scheme reflects the sequential evolution of AD from an initial stage characterized by the appearance of abnormal biomarkers in asymptomatic individuals. As biomarker abnormalities progress, the earliest subtle symptoms become detectable. Further progression of biomarker abnormalities is accompanied by progressive worsening of cognitive symptoms, culminating in dementia (Jack et al., 2018).
The numerical clinical staging scheme is as follows:
- Performance within expected range on objective cognitive tests
- Normal performance within expected range on objective cognitive tests. (Transitional cognitive decline: Decline in previous level of cognitive function, which may involve any cognitive domains
- Performance in the impaired/abnormal range on objective cognitive tests
- Mild dementia
- Moderate dementia
- Severe dementia (Jack et al., 2018)
In 2018 an Alzheimer’s Association workgroup lead by Alireza Atri published a report describing the need for clinical practice guidelines for use in primary and specialty care settings. The guidelines build on the NIA_AA guidelines but add a clinical component for the evaluation of cognitive impairment thought to be related to Alzheimer’s disease or a related type of dementia. Key components include:
- All middle-aged or older individuals who self-report or whose care partner or clinician report cognitive, behavioral or functional changes should undergo a timely evaluation.
- Concerns should not be dismissed as “normal aging” without a proper assessment.
- Evaluation should involve not only the patient and clinician but, almost always, also involve a care partner (e.g., family member or confidant). (Atri, 2018)
