Since the concept of implicit bias was first introduced in 1995, it has permeated almost all aspects of equity, diversity, and inclusion training programs (Sukhera, 2020). These programs often focus on individual healthcare providers, but because of long-standing systemic health inequities, bias training directed toward an individual is only one part of a program to address disparities. Addressing the challenges and complexities associated with a rapidly changing healthcare system is an important part of an overall strategy to reduce bias.
Improving Attitudes, Reducing Disparities
Training to reduce implicit bias should provide concrete strategies that focus on improving provider communication, particularly non-verbal skills (Dirks et., 2022). When people are exposed to or are invited to think about traits or behaviors that counter their stereotypes, they became less prejudicial toward that social group. Equality of status, social and institutional support, pleasant contact, and intergroup cooperation often produce positive results (Brusa et al., 2021).
A Multipronged Approach
Sustaining the effects of bias training requires changes in policy and visible support of organizational leaders. Rather than focusing exclusively on training others, leaders must consider their own approaches to equity and diversity. Leaders who model a more inclusive approach and integrate bias training with other initiatives to enhance inclusion and belonging within their organization are more successful than those who rely on training alone (Sukhera, 2020).
Bias training is most effective when the approach is multipronged, when people work and train together, and when it is designed with context and professional identity in mind. Training in teams helps individuals feel comfortable sharing their biases and accepting their vulnerabilities. Training that enhances collaboration and openness reinforces behavioral change (Sukhera, 2020).
Applying a Health Equity Lens
Despite efforts at the federal, regional, state, and local levels, health disparities persist. Researchers continue to examine how policies, both historic and contemporary, perpetuate these disparities (Douglas et al., 2019).
Applying a “health equity lens” means intentionally looking at the potential positive and negative impacts of training materials and policies. This means communication planning, development, and dissemination must be inclusive and avoid bias and stigmatization.
When applying a health equity lens:
- Identify the health equity issue and affected population.
- Analyze the policy impacts and opportunities for improvement.
- Develop research strategies in partnership with community stakeholders.
- Evaluate policy outcomes and their impact on heath disparities.
- Disseminate findings to stakeholders, including policy makers, communities, public health officials, and healthcare providers.
(Douglas et al., 2019)
Applying a health equity lens to media can influence attitudes towards members of different social groups. Media can reinforce prejudices and stereotypes but can also raise awareness and influence attitudes. A number of studies have shown that implicit racial stereotypes are decreased when people are exposed to news stories countering those stereotypes (Brusa et al., 2021).
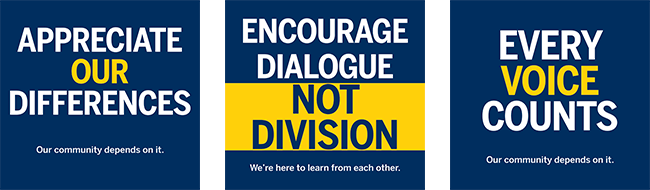
Source: University of Michigan, used with permission.
The Michigan Health Equity Project
In Michigan, the Centers for Medicare & Medicaid Services has provided funding for the Health Equity Project in five Michigan counties (Washtenaw, Genesee, Jackson, Kent, and Livingston). The Health Equity Project helps these counties reduce health disparities associated with social needs such as housing instability, food insecurity, transportation, health system complexity, and other socioeconomic factors (U of M, 2021).
The Health Equity Project:
- supports efforts to connect people from historically disadvantaged populations to needed social services,
- shares data between relevant health and social service providers to facilitate improved care,
- provides population-based data to analysts, stakeholders, and policymakers, and
- engages with, and reflects on, the views of community members with lived experience (U of M, 2021).
Michigan Social Health Interventions to Eliminate Disparities (MSHIELD)
In traditional health care systems, we go to the doctor when we’re sick; if we have a chronic condition, we get treatment for that. But, for me, when we talk about healthcare, we have to talk about education, employment, quality of housing, the food people have access to—all of those are health issues, too.
Kirk Smith, President, CEO of the Greater Flint Health Coalition
The MSHIELD program seeks to eliminate healthcare disparities by working with existing community programs in four Michigan geographic regions* to address the needs of high-risk medical and surgical patients. The program employs community health workers and care managers to help patients navigate complex healthcare and social services systems (MSHIELD, 2022).
*Kent County’s Health Net of West Michigan, Jackson Care Hub, Livingston and Washtenaw Counties’ Michigan Community Care, Genesee Community Health Access Program.
Evidence shows that interventions focusing on social determinants of health lead to better health outcomes and lower costs. This MSHIELD program tries to identify patients with unmet social needs who are at high risk for receiving costly, low-value care. Failure to address unmet social needs directly contributes to health inequities and low-value care (MSHIELD, 2022).
