An indicator is an alert or warning that you need to give more attention to a situation. Indicators of abuse can be obvious: for example, a child with the mark of a belt showing on his or her back or burns in the shape of an iron or cigarette tip gives clear support for reasonable cause to suspect child abuse. Often your suspicion will rest on less obvious physical or behavioral indicators.
Indicators must always be considered within the context of how a child behaves, how he or she looks, what you know about the child, and the child’s family situation and history. Children do not react the same way to similar circumstances and many abused children may not show any of the indications discussed below. Nevertheless, learning to recognize high-risk situations and the signs and symptoms of abuse is an important skill for a mandated reporter. Indicators can alert you to physical, sexual, and mental abuse or neglect.
11.1 Indicators of Bodily Injury (23 Pa.C.S. § 6303)
General rule—the following words and phrases, when used in the PA CPSL, shall have the meanings given to them in this section unless the context clearly indicates otherwise:
Bodily injury is the impairment of physical condition or substantial pain.
- Impairment: if, due to the injury, the child’s ability to function is reduced temporarily or permanently in any way.
- Substantial pain: if the child experiences what a reasonable person believes to be substantial pain.
Indicators of physical abuse do not, in and of themselves, prove that a child has been abused. Keep in mind that injuries occur accidentally when children play. Physical abuse should be considered when the explanation does not fit the pattern or frequency of injury. When physical abuse has occurred, indicators can be behavioral as well as physical.
Indicators of bodily injury include unexplained injuries, unbelievable or inconsistent explanations of injuries or injuries that are inconsistent with a child’s age/developmental level. Other indicators:
- Fear of going home
- Fear of parent or caregiver
- Extreme apprehensiveness/vigilance
- Pronounced aggression or passivity
- Flinches easily or avoids being touched
- Play includes abusive talk or behavior
- Unexplained injuries
- Unbelievable or inconsistent explanations of injuries
- Injuries inconsistent with a child’s age/developmental level
- Unable to recall how injuries occurred, or account of injuries is inconsistent with the nature of the injuries
- Multiple bruises in various stages of healing
- Bruises located on face, ears, neck, buttocks, back, chest, thighs, back of legs, and genitalia
- Bruises that resemble objects such as a hand, fist, belt buckle, or rope
- Burns
11.2 Indicators of Sexual Abuse or Exploitation
Despite common beliefs that sexual abusers are strangers, in more than 80% of cases the abuser is likely to know the child they are sexually abusing. Victims may be threatened with negative consequences to keep them silent. Certain factors contribute to silence, including secrecy, helplessness, entrapment, accommodation, and the fear of not being taken seriously when revealing abuse.
Physical indicators of sexual abuse or exploitation can include positive testing for sexually transmitted disease or HIV, pain or irritation in the genital or anal areas, and difficulty walking, sitting, or urinating. Other physical indicators include:
- Sleep disturbances
- Bedwetting
- Pregnancy
- Excessive or injurious masturbation
Behavioral indicators of sexual abuse or exploitation include cruelty to animals, anxiety, withdrawal, and cruelty to other children or adults. Additional behavioral indicators can include:
- Sexually promiscuity
- Developmental, age-inappropriate sexual play and/or drawings
- Fire setting
11.3 Indicators of Serious Mental Injury
Mental and emotional injury may be the most prevalent type of child abuse; however, it is among the most hidden, underreported, and least studied. However, a large body of evidence has demonstrated that exposure to childhood maltreatment at any stage of development can have long-lasting consequences.
Physical indicators of serious mental injury include:
- Frequent psychosomatic complaints (nausea, stomachache, headache, etc.)
- Bed-wetting
- Self-harm
- Speech disorders
Behavioral indicators of serious mental injury may include evidence of an eating disorder, poor relations with other children or peers, or expressing feelings of inadequacy. Other indicators can include:
- Fear of trying new things
- Overly compliant behaviors
- Excessive dependence on adults
- Habits such as sucking or rocking
11.4 Indicators of Serious Physical Neglect
Physical neglect is an act of abuse. It accounts for over three-quarters of confirmed cases of child maltreatment in the United States—far more than physical or sexual abuse—but it continues to receive less attention from practitioners, researchers, and the media.
Identifying serious physical neglect in children may seem more difficult than identifying other forms of abuse because neglect usually involves the absence of a certain behavior, rather than the presence. A thorough investigation of the child’s safety and risk followed by a comprehensive family assessment can help determine what kinds of services and supports the family may need.
Physical indicators of serious physical neglect may include the presence of persistent, untreated conditions such as head lice or diaper rash, lack of medical and dental care, developmental delays, or dirty or inappropriate clothing for the weather or clothing too large or too small. Other indicators of physical neglect can include:
- Hunger
- Lack of shelter
- Weight is significantly lower than normal for their age and gender
- Exposure to hazards such as illegal drugs, rodent or insect infestation, or mold
Behavioral indicators of serious physical neglect can include poor impulse control, unusual fatigue, or a child not registered in school. Other indicators of physical neglect can include:
- Inadequate or inappropriate supervision
- Parentified behaviors (when children are forced to take on the role and responsibilities of a parent)
Healthcare providers must differentiate between neglectful situations and poverty. For example, if a family living in poverty was not providing adequate food for their children, it would be considered neglect only if the parents were aware of but chose not to use food assistance programs. Taking poverty into consideration can prevent unnecessary removals and place the focus on providing concrete services for families to protect and provide for their children.
11.5 Risk Factors for Child Abuse and Neglect
[Unless otherwise noted, the following section is from CDC, 2024, February 22).
Risk factors are characteristics associated with child abuse and neglect—they may or may not be direct causes. A combination of individual, relational, community, and societal factors contribute to the risk of child maltreatment. Although children are not responsible for the harm inflicted upon them, certain characteristics have been found to increase their risk of being maltreated.
Individual Risk Factors for Victims
- Children younger than 4 years of age
- Special needs that may increase caregiver burden (e.g., disabilities, mental retardation, mental health issues, and chronic physical illnesses)
Individual Risk Factors for Perpetration
- Parents’ lack of understanding of children’s needs, child development and parenting skills
- Parents’ history of child maltreatment in family of origin
- Substance abuse and/or mental health issues including depression in the family
- Parental characteristics such as young age, low education, single parenthood, large number of dependent children, and low income
- Non-biological, transient caregivers in the home (e.g., mother’s male partner)
- Parental thoughts and emotions that tend to support or justify maltreatment behaviors
Family Risk Factors
- Social isolation
- Family disorganization, dissolution, and violence, including intimate partner violence
- Parenting stress, poor parent-child relationships, and negative interactions
Community Risk Factors
- Community violence
- Concentrated neighborhood disadvantage (e.g., high poverty and residential instability, high unemployment rates, and high density of alcohol outlets), and poor social connections
11.6 Shaken Baby Syndrome
Shaken baby syndrome/abusive head trauma (SBS/AHT) is a special type of physical abuse. It is a term used to describe the constellation of signs and symptoms resulting from violent shaking or shaking and impacting of the head of an infant or small child.
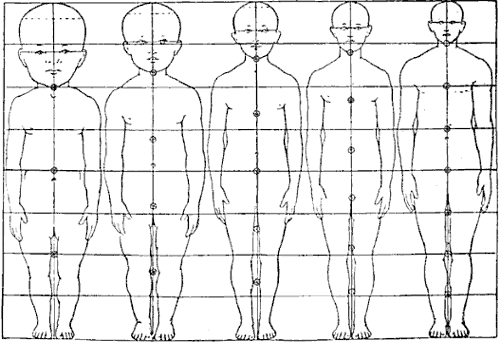
Infants 2 to 4 months of age are at the greatest risk of injury from shaking, because their brains are softer, and their skulls are thinner than those of adults. An infant’s head is also larger in proportion to its body than an adult’s head and its neck muscles, tendons, and ligaments are weaker than those of an adult.
Source: Wellcome Images. Licensed under the Creative Commons Attribution 4.0 International license.
Shaking a baby may cause bruising, swelling, and bleeding (intracerebral hemorrhage) of the brain which may lead to permanent, severe brain damage or even death. It usually occurs in children younger than 2 years old but may be seen in children up to the age of 5.
There are various signs of SBS/AHT and in less severe cases the child may not be seen by a medical professional and properly diagnosed. In most severe cases a child quickly becomes unconscious with “rapidly escalating central nervous system dysfunction.” Injuries from SBS/AHT can result in severe disability or death and if you suspect a child has been shaken you should seek immediate medical attention.
