The ugly reality is that dementia often manifests as a relentless and cruel assault on personhood, comfort, and dignity. It siphons away control over thoughts and actions, control that we take for granted every waking second of every day.
Michael J. Passmore, Geriatric Psychiatrist
University of British Columbia
Dementia is the collective name for progressive, global deterioration of the brain’s executive functions. It develops primarily in later adulthood and is a major cause of disability in older adults. Almost everyone with dementia is elderly but nevertheless dementia is not considered a normal part of aging.
Very early identification of dementia—before obvious symptoms appear—is an intense focus of research. Staging (used primarily in the research setting) and correctly diagnosing dementia is becoming increasingly important in the clinical setting. Understanding the difference between Alzheimer’s disease and other types of dementia and differentiating dementia from delirium and depression is of critical importance.
Once a person has been diagnosed with any form of dementia, management becomes a priority. Because dementia is progressive, patients and caregivers are faced with the challenge of managing an array of behavioral issues associated with dementia while providing more care as the disease progresses. Dementia is not an easy disease, either for the person experiencing the progressive loss of independence and control or for caregivers and family members. Education, collaboration, communication, and support are critical.
Did you know . . .
Worldwide more than 35 million people live with dementia and this number is expected to double by 2030 and triple by 2050 (Alzheimer’s Disease International).
Although dementia is widespread in humans and occurs throughout the world, its exact cause is still unknown. In Alzheimer’s disease, and likely in other forms of dementia, damage within the brain is associated with the formation of unwanted structures called beta-amyloid plaques andneurofibrillary tangles. It is also related to the degeneration and loss of nerve cells within the brain.
Degeneration of Cerebral Neurons
Left: A healthy nerve cell. Right: A dying nerve cell. Source: ADEAR, 2014, Public domain.
We are learning that the changes associated with dementia occur over years, or even decades, before emotional, physical, or cognitive symptoms emerge. Eventually symptoms become obvious, and they lead to gradual and progressive decline (DeFina et al., 2013).
Alzheimer’s Dementia

Different levels of contrast, with less contrast below (50%, 75%). Source: Wikimedia Commons.
You likely already know that Alzheimer’s disease (AD) is the most frequent and most studied cause of dementia in older adults. Its onset is gradual and progressive, meaning it gets worse over time. Memory problems are the most common early symptom of AD although language difficulties, apathy, depression, and vision and spatial difficulties can also be early symptoms. The latter two symptoms are less studied than memory changes but can be just as debilitating. Difficulties with vision and spatial awareness affect reading and comprehension of form and color, and can affect the ability to see contrast. This can make it difficult to detect motion and process visual information accurately (Quental et al., 2013).
The progressive brain damage associated with Alzheimer’s dementia is illustrated in the drawings below, which show the formation and spread of plaques and tangles in the brain. In the earliest stage, before symptoms appear, plaques and tangles form in an area of the brain called the hippocampus, where new memories are formed (A). As the disease progresses, plaques and tangles spread to the front part of the brain; symptoms begin to be obvious at this stage (B). In the severe stage (C), plaques and tangles are found throughout the brain. Damage eventually affects memory, emotions, communication, safety awareness, logical thinking, recognition of loved ones, and the ability to care for oneself.
The Progression of Alzheimer’s Disease
A
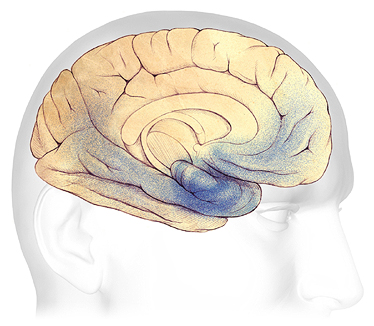
B
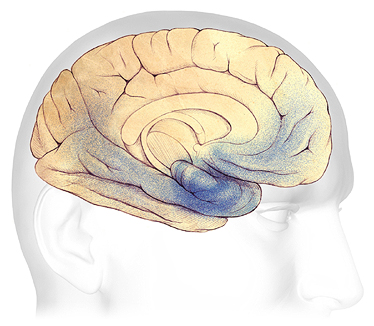
C
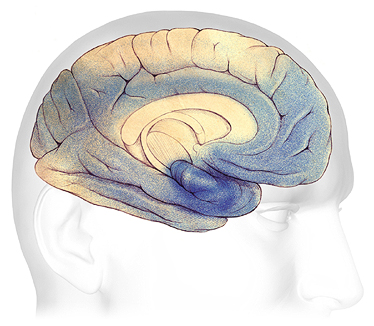
A: Plaques and tangles (shaded in blue) are beginning to form within the hippocampus. B: As the disease progresses, they spread toward the front and rear of the brain. C: In severe Alzheimer’s, plaques and tangles cause widespread damage throughout the brain. Source: Courtesy of The Alzheimer’s Association. Used with permission.
Changes within the brain affect every aspect of a person’s life. Memory is at the very core of who we are as a person. Difficulties with vision and spatial awareness affect our ability to move about safely in the environment. Because of these changes, walking on a busy street can be dangerous, driving is no longer safe, and avoiding obstacles is a challenge.
It turns out that memory loss isn’t the only thing that happens in early Alzheimer’s disease. In fact the hippocampus is just one part of a larger brain structure called the limbic system. This area of the brain is not only responsible for the formation of new memories; it is also involved with emotions.
Non-Alzheimer’s Dementia
Although Alzheimer’s disease is the most common and well-known form of dementia, there are other causes and types of dementia that you are likely to encounter in your work. Some other common types of dementia include:
- Vascular dementia and vascular cognitive impairment
- Frontotemporal dementia
- Dementia with Lewy bodies
- Dementia associated with Parkinson’s disease
In all, nearly twenty different types of non-Alzheimer’s dementia have been identified. Determining if someone has Alzheimer’s disease or another type of dementia is important because some types of dementia are treatable and reversible if the underlying cause is identified and treated (Sönke, 2013).
Vascular Dementia and Vascular Cognitive Impairment
Vascular dementia and vascular cognitive impairment are umbrella terms that refer to damage caused by injuries to the vessels supplying blood to the brain. Damage can be due to multiple small strokes or to any injury to the small vessels within the brain. Generally, the first symptoms of vascular dementia are difficulty making decisions and impaired judgment. The risk of developing dementia from vascular damage can be significant even when individuals have suffered only small strokes or minor damage to the blood vessels (NINDS, 2021).
Vascular dementia is the second most common form of dementia after Alzheimer’s disease, affecting approximately 20% of the dementia cases worldwide (Neto et al., 2015). Risk factors for developing vascular dementia and vascular cognitive impairment include heart rhythm irregularities, high blood pressure, diabetes, high cholesterol, smoking, and obesity. Vascular dementia also has been associated with a condition called amyloid angiopathy, in which amyloid plaques accumulate in the blood vessel walls, causing them to break down and rupture (NINDS, 2021).
Symptoms of vascular dementia and vascular cognitive impairment often begin suddenly and usually proceed in a step-wise progression. This means the symptoms stay the same for a period of time, and then suddenly get worse, usually as a result of additional small strokes or other vascular damage.
In vascular dementia, memory is less affected than in Alzheimer’s but mood changes are more common. Cognitive impairment often seems “patchy” because of the many areas of the brain that are affected. Vascular dementia can be largely prevented if the underlying causes are identified and addressed.
Frontal-Temporal Dementia
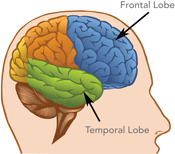
Damage to the brain’s frontal and temporal lobes causes forms of dementia called frontotemporal disorders. Source: National Institute on Aging.
Frontal-Temporal (frontotemporal) dementia begins in the frontal and temporal lobes of the brain. This contrasts with Alzheimer’s dementia, in which damage begins in the hippocampus and then spreads to the front part of the brain. Frontotemporal dementia typically starts at an earlier age than Alzheimer’s disease; it is a relatively common type of dementia in those under the age of 60.
In the early stages of frontotemporal dementia, judgment is more affected than memory, although memory is eventually affected as well. There is a gradual and progressive change in behavior (mood changes, apathy, and disinhibition*), gradual difficulties with language, and gradual weakness or slowing of movement. Behavior is often referred to as “odd,” “socially inappropriate,” and “schizoid.”
*Disinhibition: a loss of inhibition, a lack of restraint, disregard for social convention, impulsiveness, poor safety awareness, an inability to stop strong responses, desires, or emotions.
Because frontotemporal dementia can also affect the hippocampus and because of the many variations found in the disease, it is often difficult to tell the difference between frontotemporal dementia and Alzheimer’s disease. It can also be confused with other psychiatric conditions such as late-onset schizophrenia.
Dementia with Lewy Bodies
Dementia with Lewy bodies is one of the most common types of progressive dementia. It is caused by the buildup of abnormal proteins called Lewy bodies inside nerve cells in areas of the brain responsible for certain aspects of memory and motor control. It is not known exactly why Lewy bodies form or how Lewy bodies cause the symptoms of dementia (NINDS, 2015).
The central features of dementia with Lewy bodies are progressive cognitive decline, “fluctuations” in alertness and attention, visual hallucinations, and parkinsonian motor symptoms, such as slowness of movement, difficulty walking, or rigidity (stiffness). People may also suffer from depression (NINDS, 2015).
Difficulty sleeping, loss of smell, and visual hallucinations can precede movement and other problems by as much as 10 years. Because of this, dementia with Lewy bodies can go unrecognized or be misdiagnosed as a psychiatric disorder until its later stages (NINDS, 2021).
The similarity of symptoms between dementia with Lewy bodies, Parkinson’s disease, and Alzheimer’s disease can make diagnosis difficult. It is possible that either dementia with Lewy bodies is related to these other causes of dementia or that an individual can have more than one type of dementia at the same time. Dementia with Lewy bodies usually occurs in people with no known family history of the disease. However, familial cases have occasionally been reported (NINDS, 2015).
Parkinson’s Disease Dementia
Mild cognitive impairment is common in the early stages of Parkinson’s disease and a majority of people with Parkinson’s disease will eventually develop dementia. The time from the onset of movement symptoms to the onset of dementia symptoms varies greatly from person to person.
Cognitive problems such as impaired memory, lack of social judgment, language difficulties, and deficits in reasoning can develop over time. Autopsy studies show that people with Parkinson’s disease dementia often have amyloid plaques and tau tangles similar to those found in people with Alzheimer’s disease, though it is not understood what these similarities mean.
Risk factors for developing Parkinson’s disease dementia include the onset of Parkinson’s-related movement symptoms followed by mild cognitive impairment and sleep disorders, which involves frequent vivid nightmares and visual hallucinations (NINDS, 2021).
Dementia with Lewy bodies and Parkinson’s disease dementia are now recognized in the Diagnostic and Statistical Manual of Mental Disorders (DSM-5), where they are respectively coded as “Major and Mild Neurocognitive Disorder with Lewy Bodies” and as “Major and Mild Neurocognitive Disorder due to Parkinson’s Disease” (Donaghy & McKeith, 2014).
Back Next