Human coronaviruses have been regarded historically as relatively benign causes of the common cold. Three times in the twenty-first century, however, coronavirus outbreaks have emerged from animal reservoirs to cause severe disease and global transmission concerns; severe acute respiratory syndrome (SARS), which emerged in late 2002 and disappeared by 2004; Middle East respiratory syndrome (MERS), which was first identified in 2012 and consistently jumps from dromedary camels to people; and the 2019 novel coronavirus (COVID-19), that emerged in December 2019 from China (NIH, 2020).
SARS Virus
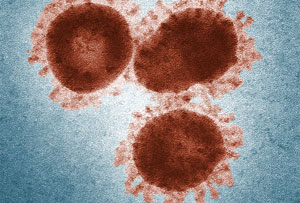
Source: CDC.
SARS was an atypical pneumonia first detected in eastern China during the winter of 2002–2003. The organism was found to be a new, highly pathogenic, coronavirus. The outbreak brought back memories of the influenza pandemic of 1918–1919 in which as many as 50 million people died worldwide. The World Health Organization (WHO) called for immediate action against SARS and directed its Global Outbreak and Response Network in Geneva, Switzerland to coordinate efforts to monitor the spread of SARS throughout the world. (WHO, GOARN, 2005).
The index case for the ensuing epidemic was a middle-aged businessman named Johnny Cheng who had traveled extensively in Southeast Asia and China before becoming ill. Unknowingly infected with the new virus, Cheng travelled to Hong Kong and checked into room 911 of the Metropole Hotel. He was admitted to a hospital on February 26, 2003 with a high fever, dry cough, myalgia, and mild sore throat. Over the following 4 days he developed symptoms of acute respiratory distress syndrome (ARDS) requiring ventilatory support, and severe thrombocytopenia. Despite intensive therapy he died on March 13, 2003 after being transferred to an isolation facility in Hong Kong.
During his short stay at the Metropole, Cheng infected more than a dozen other guests on the ninth floor of the hotel, who then took SARS with them back to Toronto, Singapore, and Hanoi. Over the next eight months, the disease killed 775 people in 29 countries and cost the global economy billions of dollars (NPR, 2020).
Before discovering the cause of SARS, WHO received hundreds of reports about people who were sick with a pneumonia possibly related to “bird flu.” The first reports came from Canada, China, Hong Kong, Indonesia, Philippines, Singapore, Thailand, and Vietnam. SARS was quickly categorized as an atypical pneumonia of unknown etiology (WHO, 2003).
Early manifestations included influenza-like symptoms such as fever, myalgias, headache, sore throat, dry cough, shortness of breath, and difficulty breathing. In some cases, these symptoms were followed by hypoxia, pneumonia—and occasionally acute respiratory distress (requiring mechanical ventilation) and death.
Laboratory findings included thrombocytopenia and leukopenia. Some close contacts, including healthcare workers, developed similar illnesses. Centers for Disease Control and Prevention (CDC) initiated surveillance for cases of SARS among travelers and their close contacts (CDC, 2005).
WHO and the CDC launched a massive research, surveillance, and containment program to try to prevent the spread of SARS. In response to requests for assistance, WHO Global Outbreak Alert and Response Network (GOARN) field teams were deployed to help local health authorities investigate and control the outbreaks. (WHO, GOARN, 2005).
Through effective public health efforts and international cooperation among leaders, scientists, and healthcare workers, a global pandemic was avoided. Classic public health measures of isolation and containment are likely what brought the outbreak to an end. No human cases of SARS have been reported anywhere in the world since 2004 (NIH, 2020).
Identifying a Coronavirus
There are hundreds of coronaviruses, most of which circulate among animals including pigs, camels, bats, and cats. Sometimes these viruses jump to humans—a spillover event—and can cause disease, as happened with SARS, Middle East Respiratory Syndrome (MERS), and now with COVID-19 (NIH, 2020a).
Coronaviruses are named for the crown-like spikes on their surface. There are four main sub-groupings of coronaviruses, known as alpha, beta, gamma, and delta. Only seven of these viruses are known to cause human disease—four of which cause mild to moderate upper-respiratory tract illnesses, like the common cold. However, as noted earlier, three times in the twenty-first century coronavirus outbreaks have emerged from animal reservoirs to cause severe disease and global transmission concerns; SARS, which emerged in late 2002 and disappeared by 2004; MERS, which was first identified in 2012 and consistently jumps from dromedary camels to people; and the 2019 novel coronavirus, that emerged in December 2019 from China (NIH, 2020a).
While most coronaviruses only infect animals, MERS and SARS are notable for their ability to infect a variety of species, including humans. Recent research at the National Institute of Allergy and Infectious Diseases (NIAID) shows how the MERS virus can adapt to infect cells of a new species, which suggests that other coronaviruses might be able to do the same (NIH, 2018). It appears that the most recent human coronavirus, COVID-19, has done just that. A global effort was needed to contain its spread.
Transmission of SARS
[Material from this section is from WHO, GOARN, 2005.]
SARS spread rapidly within China during 2003, while subsiding in other countries. On April 28, 2003, Viet Nam was removed from the list of affected countries, making it the first country to successfully contain its SARS outbreak. The change in Viet Nam’s status followed 20 consecutive days (the duration of two incubation periods) since the last new case was detected. Key actions undertaken by that country included early recognition of the outbreak, the consolidation of SARS patients in a single hospital, strict infection control, diligent contact tracing, and thorough investigation of all rumored cases.
Although Viet Nam was removed from WHO’s list of affected countries, it was advised to maintain a high level of alert since even a single new case of SARS could have sparked another outbreak. Because of continued infections in China, the Vietnamese health ministry heightened its border surveillance with that country.
One day later, a WHO travel advisory recommending postponement of all but essential travel to Toronto, Canada was lifted. Toronto had not had a new case of SARS outside of a medical facility for 20 days but remained on alert. Canada agreed to increase airport screening, including use of thermal imaging machines to check passengers for fever. WHO cautioned that Toronto still had an outbreak of SARS and the travel advisory situation could change if any new cases were discovered.
WHO established logistic bases and sent supplies of protective and clinical equipment to all affected countries. On March 15, 2003, WHO published a travel advisory notice advising all individuals traveling to affected areas to watch for the development of symptoms for a period of 10 days after returning home. On May 10, 2003, WHO updated the advisory, recommending that people planning to travel to Mainland China, Taiwan and Hong Kong consider postponing all but essential travel. Travel alerts were reassessed regularly.
The overall death (mortality) rate from SARS was about 10% and it increased substantially with age:
- Patients under 24 years of age had a mortality rate of about 1%
- Patients aged 25 to 44 had a mortality rate of 6%
- Patients aged 45 to 65 had a mortality rate of 15%
- Those over 65 years of age had a 50% or higher mortality rate (CNBC, 2020)
Symptoms of SARS
SARS was a new coronavirus that jumped from animals to humans and the first that caused severe disease. Prior to SARS, there were only four known human coronaviruses and they caused mild to moderate respiratory symptoms. The criteria to identify suspected SARS patients was the onset of symptoms following February 1, 2003, and:
- Measured temperature >100.4°F (>38°C) and
- One or more clinical findings of respiratory illness (e.g. cough, shortness of breath, difficulty breathing, hypoxia) and
- Travel within 10 days of onset of symptoms to an area with suspected or documented community transmission of SARS (excludes areas with secondary cases limited to healthcare workers or direct household contacts). Travel included transit in an airport in an area with documented or suspected community transmission of SARS.
or
- Close contact* within 10 days of onset of symptoms with a person known to be a suspected SARS case.
*Close contact was defined as having cared for, lived with, or having had direct contact with respiratory secretions and/or body fluids of a patient suspected of having SARS.
Areas that had documented or suspected community transmission of SARS were:
- Peoples’ Republic of China (i.e., Mainland China and Hong Kong Special Administrative Region)
- Hanoi, Vietnam
- Singapore
- Toronto, Canada
In the United States, by the time the epidemic was over, only 8 people had laboratory evidence of SARS infection. All of those people had traveled to other parts of the world where SARS was spreading. SARS did not spread more widely in the community in the United States.
Probable cases showed:
- Radiographic evidence of pneumonia or respiratory distress syndrome
- Autopsy findings consistent with respiratory distress syndrome without an identifiable cause
Clinical History of SARS
[Unless otherwise cited, material from this section is from WHO, 2020.]
SARS was a viral respiratory illness caused by a coronavirus, called SARS-associated coronavirus (SARS-CoV). The illness was first reported in Asia in February 2003. Over the next few months, it spread to more than two dozen countries in North America, South America, Europe, and Asia before the SARS global outbreak of 2003 was contained (CDC, 2017).
Based on data from the Hanoi and Hong Kong SAR, the incubation period was estimated to be 2 to 7 days, but usually 3 to 5 days. Attack rates of >56% among healthcare workers caring for patients with SARS was consistent in both the Hong Kong and Hanoi areas.
Reported Cases of SARS (November 1, 2002 to May 10, 2003) | ||
|---|---|---|
Country | Cumulative number of case(s) | Number of deaths |
Australia | 4 | 0 |
Brazil | 2 | 0 |
Bulgaria | 1 | 0 |
Canada | 145 | 22 |
China | 4882 | 235 |
China, Hong Kong | 1674 | 212 |
China, Taiwan | 172 | 18 |
France | 7 | 0 |
Germany | 9 | 0 |
Italy | 9 | 0 |
Malaysia | 7 | 2 |
Mongolia | 9 | 0 |
Philippines | 10 | 2 |
Singapore | 205 | 27 |
Thailand | 7 | 2 |
United Kingdom | 6 | 0 |
United States | 64 | 1 |
Viet Nam | 63 | 5 |
Total | 7296 | 526 |
By March 21, 2003, the majority of patients identified as having SARS were adults aged 25 to 70 years who were previously healthy. Few suspected cases of SARS were reported among children aged <15 years. Though the incubation period for SARS was typically 2 to 7 days, isolated reports suggested an incubation period as long as 10 days.
The illness began with a prodrome of fever (>100.4°F [>38.0°C]) that was often high and sometimes associated with chills, rigors, headache, malaise, and myalgia. At the onset of illness, some people had mild respiratory symptoms. Typically, rash or neurologic or gastrointestinal findings were absent; however, some patients reported diarrhea during the febrile prodrome.*
*Prodrome is an early symptom indicating the onset of a disease or illness.
After 3 to 7 days, a lower respiratory phase began with the onset of a dry, nonproductive cough or dyspnea, which might have been accompanied by or progressed to hypoxemia. In 10% to 20% of cases, the respiratory illness was severe enough to require intubation and mechanical ventilation. The case–fatality rate among persons with illness meeting the WHO case definition of SARS ended up at 9.6%.
Chest x-rays were sometimes normal during the febrile prodrome and throughout the course of illness. However, in a substantial proportion of patients, the respiratory phase was characterized by early focal interstitial infiltrates that progressed to more generalized, patchy, interstitial infiltrates. Some chest x-rays from patients in the late stages of SARS also showed areas of consolidation.
Early in the course of disease, the lymphocyte count was often decreased. At the peak of the respiratory illness, approximately 50% of patients had leukopenia and thrombocytopenia or low-normal platelet counts of 50,000 to 150,000/µL. Early in the respiratory phase, elevated creatine phosphokinase levels (as high as 3,000 IU/L) and hepatic transaminases (2 to 6 times the upper limits of normal) were noted. In the majority of patients, renal function remained normal.
The severity of illness was highly variable, ranging from mild illness to death. Although a few close contacts of patients with SARS developed a similar illness, the majority remained well. Some close contacts reported a mild, febrile illness without respiratory signs or symptoms, suggesting the illness might not always progress to the respiratory phase.
Before the cause of the illness was discovered, treatment regimens included several antibiotics to treat presumptively known bacterial agents of atypical pneumonia. In several locations, therapy also included antiviral agents such as oseltamivir or ribavirin. Steroids were also administered orally or intravenously to patients in combination with ribavirin and other antimicrobials. None of these treatments were effective against SARS.
In the United States, clinicians who suspected cases of SARS were requested to report such cases to their state health departments. CDC requested that reports of suspected cases from state health departments, international airlines, cruise ships, or cargo carriers be directed to the SARS Investigative Team at the CDC Emergency Operations Center. Outside the United States, clinicians who suspect cases of SARS were requested to report such cases to their local public health authorities.
Epidemic SARS
SARS was a diagnosis of exclusion. Initial diagnostic testing included chest radiograph, pulse oximetry, blood cultures, sputum Gram stain and culture, and testing for viral respiratory pathogens, notably influenza A and B and respiratory syncytial virus. A specimen for legionella and pneumococcal urinary antigen testing was also considered. Clinicians saved any available clinical specimens (respiratory, blood, and serum) for additional testing until a specific diagnosis was made. Acute and convalescent (greater than 21 days after onset of symptoms) serum samples were collected from each patient who met the SARS case definition. Paired sera and other clinical specimens were forwarded through State and local health departments for testing at CDC.
Laboratory Worker Testing for SARS

Source: CDC.
In California there were more patients who met the criteria for suspect and probable SARS than any other state and hundreds of patients were evaluated in local hospitals and clinics. Patients were tested for known respiratory illnesses in order to rule out other illnesses. Many emergency rooms, hospitals, and public health offices were overwhelmed. Hundreds of persons were evaluated by local counties before being reported to the health department, where they were then classified as having suspect or probable SARS.
In California, determining a commonly recognized cause for an influenza-like illness allowed cases to be removed from the suspect or probable SARS categories. The resultant removal of a SARS designation alleviated the required epidemiologic investigation, hospitalization or isolation, strict infection control precautions, and additional specimen collection and contact tracing required for SARS patients (Emerging Infectious Diseases, 2004).
Clinicians who evaluated suspected SARS patients used standard precautions (e.g., hand hygiene) together with airborne (e.g., N-95 respirator) and contact (e.g., gowns and gloves) precautions. Eye protection was also recommended for all patient contact.
