If patients with diabetes are not moved to take action after being taught how to care for themselves they will not thrive. Educators have developed a number of theories about how adults learn and we will look at these in this section.
Motivation to Change
Essential to effective teaching is an understanding of why and how people learn. The field of psychology helps us understand what drives human behavior. Russian physiologist Ivan Pavlov demonstrated that behavior may be based on a conditioned response of reward or punishment. If a dog is always rewarded with a bone after a bell rings, the dog will begin to salivate upon hearing the bell. For a person with diabetes, being rewarded with a good blood glucose level after daily exercise can be encouraging and can help encourage repetition of the desired behavior. Unfortunately, however, the reward of comfort food may overpower the “punishment” of a rising blood glucose level.
If a patient is reprimanded by a healthcare professional for being overweight or having chronic hyperglycemia, the patient may stop returning to the doctor’s office. Our behavior is determined by the promise/threat of reward or punishment. A teenage girl with type 1 diabetes may fear weight gain caused by insulin more than developing diabetic ketoacidosis and choose to go without her needed insulin after a meal. Identifying the predominant drive can help us understand the choices people make.
Cognitive learning theory states that people can learn logically and by social example; however, in eating we humans tend to be more emotional than rational. For example, a person may know (cognitive) that pasta elevates blood glucose more rapidly than a lean protein meal but still consume large amounts of pasta because it tastes so good (emotional). Abraham Maslow who developed humanistic learning theory, believes that what drives people to action, including learning and behavior change, is based on trying to fill the most urgent need at the time. His classic pyramid model demonstrates that the most primary human needs are survival, and only after having food, shelter, air, elimination of pain and waste, can we then focus on higher-level needs such as safety and security, social belonging, love and affection, and ultimately self-actualization.
Maslow’s Hierarchy of Needs
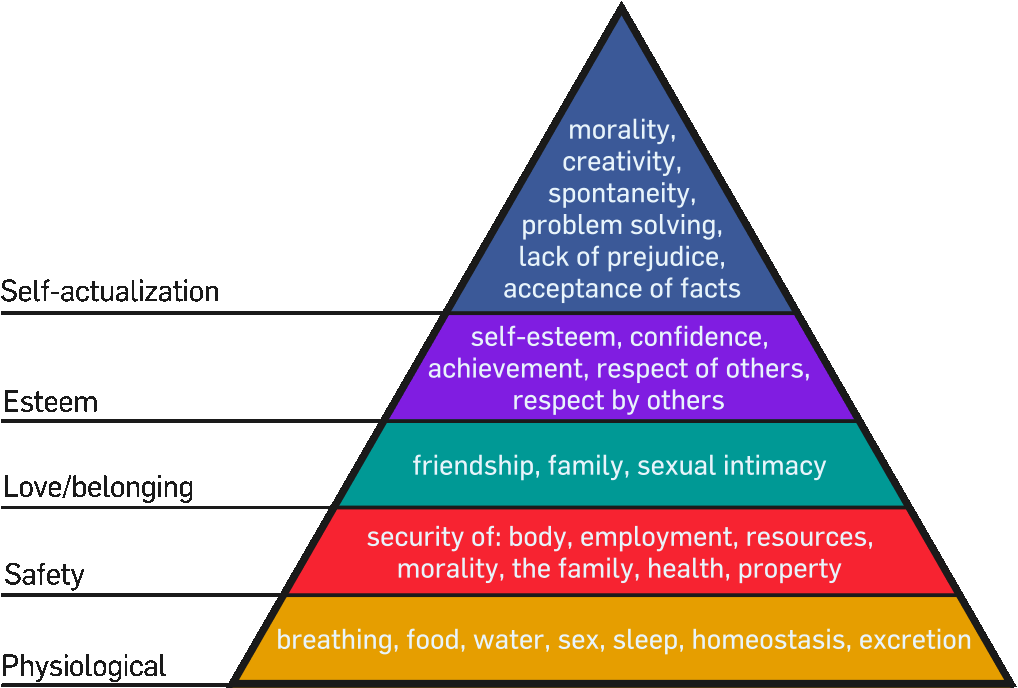
Source: Maslow, 1943; image from Wikipedia Commons.
The person with diabetes who is suffering from painful neuropathy, erratic blood sugars, and retinopathy may not be interested in sitting in a class. He may be more focused on learning about behaviors that promise elimination of pain. Sometimes simply asking “What is the most important thing to you about learning to control your diabetes right now?” can help clarify the present drive to learn.
Adult learning theory identifies how adults learn and helps anyone who teaches adults to understand what motivates them. The following list identifies basic preferences of adult learners.
- Information is related to an immediate need.
- Learning is voluntary.
- Adults are problem- centered.
- Adults are self-controlled and self-directed.
- Learning is active.
- Threat to self is minimized.
- Learning is in a group.
- Adults prefer a variety of learning activities.
- Prompt feedback is given.
Teaching people of different ages requires different approaches. Adults generally prefer information that will help solve an immediate problem or need. Adults seek prompt feedback when learning a new skill and prefer a relationship where they are not threatened. Research shows that the patient-provider relationship is crucial to adherence to a prescribed medical regimen (Ciechanowski et al., 2001).
Adults who feel safe, valued, and free of judgment may be more compliant to a prescribed management plan than those adults who feel they are “just a number” or are being talked down to. Creating a collaborative relationship that includes the patient in diagnostic results and creating the health plan is beneficial in creating positive outcomes. The approach of teaching patients self- management that empowers them to take control of their own life produces powerful improvements in health outcomes (ADA, 2015.)
Diabetes self-management support (DSMS) is defined by the ADA as “support and education for the person with diabetes that facilitates the knowledge, skill, and ability necessary for diabetes self-care.” The goal of any patient education needs to be to improve the health of the individual and reduce diabetes-associated complications. Historically, diabetes education and support has occurred primarily in hospitals and physicians’ offices, however alternative settings such as clinics, community centers, homes, pharmacies, and home-based technology are now available and accessible.
Clinical Scenario
You are teaching a man who has type 2 diabetes about his blood glucose meter and his wife continually interrupts to ask questions about food and meals.
Q: What is the best course of action for you as the diabetes educator?
A: According to adult learning theory, you need to address her pressing need for information. Allow her to ask the questions and answer them. Continue with your demonstration when she feels her questions have been answered. It is still polite to remind her your time is limited and the goal of this session is to teach them how to use the meter. Using the meter can help them both identify the effects of the meals on blood sugar.
Helpful Educational Models
Sometimes we look at educational models and assume they are meant for academics but are not relevant to our daily teaching. Consider the models that follow and what they may contribute as you teach your patients about diabetes self-care.
Health Belief Model
In addition to the learning theories, the Health Belief Model is a psychological model that can help you understand and predict health behaviors (J Pharm Prac, 2015). It can also help you to understand resistance to changing positive self-care behaviors. The model identifies factors that can either help or prevent someone from likely engaging in health-promoting behavior. If patients don’t view their health condition as serious or see that they are truly susceptible, they generally won’t take any action.
The way patients perceive self-care actions as benefits or barriers determines what they do. Even if patients acknowledge the seriousness of their condition and the benefits to behavior change, when there are barriers to the action or they don’t believe they are capable of doing the behaviors, the actions won’t occur.
The Health Belief Model is based on the patient’s perception and not necessarily on reality. Many patients continue in denial and thus don’t take action toward positive behaviors that will support their health. By addressing patients’ perceptions of their diagnosis, potential or real consequences from the medical condition, and barriers to performing self-care behaviors, you will have greater success in teaching.
The Health Belief Model
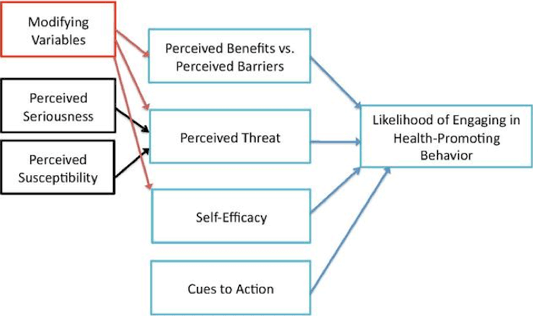
Source: Ontario Health Promotion System, 2015.
The gap between theory and practice closes as you understand the theories that explain human behavior and begin to adjust the way you teach your patients about diabetes. Teaching someone about the dangers of chronic hyperglycemia without asking if they have a glucose monitor and know how to adjust their own behaviors creates a barrier they won’t be able to overcome—and will not produce favorable glycosylated hemoglobin test results.
Teaching someone about the action of metformin and the need to take it twice daily won’t be successful if the person can’t afford the medication or doesn’t believe in the benefits of Western medicine. The theories and models can help you as you try to identify why a patient doesn’t follow prescribed medication use or behaviors. Rather than labeling a patient as “noncompliant,” try to identify the barriers to that desired behavior with the patient and create solutions together.
Clinical Scenario
Thalia Smith, a 21-year-old female with type 1 diabetes, continues to have repeated admissions to the emergency department in DKA due to inconsistency with her insulin injections.
Q: What are questions you could ask to identify the cause of her behavior?
A: What does she understand about diabetes and insulin? What are her barriers to taking insulin? Is there a cost barrier? Is she afraid of weight gain? Does she have insurance? Is she living on her own now that she is 21? Does she see a benefit to taking insulin? What is her understanding of complications from chronic hyperglycemia? Does she just have diabetes burnout?
Transtheoretical Model
Assuming the patient has been taught effectively, there are different levels of behavior change that need to be understood and acknowledged. Change is difficult, and most people are inherently resistant to change. According to the Transtheoretical Model of change, concepts from the other theories are applied to help us understand the various stages of modifying behavior (Prochaska & Prochaska, 2011). Studies show that when people try to change their behavior they move through a series of stages. The time within the stages is variable; however, progress to action and maintenance of a behavior change must follow stage by stage in a systematic manner. The process is also cyclical, in that people can slip back into earlier stages with relapse and hopeful renewal.
Think about your success regarding a New Year’s goal you set this year. Did you achieve it and stay in the ideal state of change or did your progress vary, relapse, and continue at various stages? Knowing about the various stages can help you assess and support the stage of change your patient may be in.
In the precontemplation stage a person hasn’t begun to take any thought or action toward a goal. Research states that it takes on average ten times for a healthcare professional to discuss a new behavior, such as smoking cessation, before the person begins to truly think about it. In precontemplation the action hasn’t even been seriously considered.
Transtheoretical Model
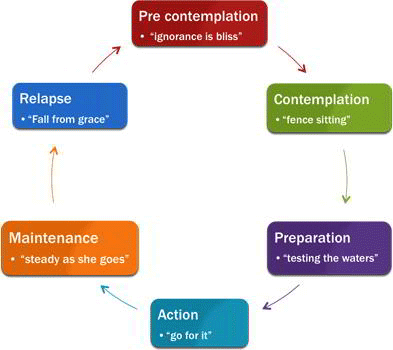
The next stage of contemplation is when the person begins to think seriously about changing a behavior. “Someday I’ll really stop smoking.” The third stage of preparation is when the person begins to think about all that is needed to make the change—for example, looking into available smoking cessation resources.
The next stage is action, when the person begins to make changes (throwing out cigarettes, joining a smoking cessation class, making an appointment to see his provider for a nicotine replacement product). According to research on behavior change, the action stage needs to occur more than 21 consecutive days to become habit. Once the new behavior has been continued for over a month, the new habit moves to the maintenance stage, which can take months or years. Relapse has been built into this model, as it recognizes human nature’s tendency to fall back into old habits. Acknowledging that change is hard and requires support, you can shore up continued efforts. Sometimes, the relapse may be so severe that the person has to begin the entire cycle anew, starting with precontemplation to decide if the effort was worth it.
Ruler Method of Change
A tool to help guide your patient change is called the ruler method. After patients identify a desired area of improvement, such as ideal weight, ask them:
- On a scale of 1 to 10, where do you think you are in this?
- How much do you want the new behavior or outcome?
Using the 1 to 10 scale, follow up with questions to help identify barriers and motivation:
- How ready are you to make that change?
- How confident are you to make that change?
- What would it take for you to move up 2 points from where you are now?
The ruler method can help identify patients’ level of change, barriers, and motivation. As the healthcare professional you don’t have to lecture or nag, but merely ask good questions to guide their own self-reflection and discovery. The burden is no longer on the diabetes educator but on the patient to explore their own readiness to change and improve health behaviors. The educator is there to answer any questions the patient may have and to guide the discussion.
The following table demonstrates what you can do to support your patients as they develop new healthy behaviors.
|
Stage of change |
Strategy |
|
Precontemplation (resistance/reluctance) |
Establish rapport, ask permission to help |
|
Contemplation (considering) |
Strengthen self-confidence |
|
Preparation |
Clarify short-term goals, resolve concerns |
|
Action |
Assist and support |
|
Maintenance |
Affirm, support, explore long-range goals |
Kübler-Ross Grieving Model
Another model pertinent to people with diabetes is the grieving model, as identified by Dr. Elizabeth Kübler-Ross (Pera et al., 2008). Each person diagnosed with diabetes experiences the loss of their former good health and goes through stages of grief similar to those of death and dying. Essentially, their old healthy self is now seen as lost. The stages vary in timing and duration and often follow the sequence of denial, anger, bargaining, depression, and acceptance.
Patients who are in the denial phase don’t make progress toward controlled blood sugar levels if they don’t believe they have diabetes and need the medication. Many people with prediabetes or metabolic syndrome deny they are at risk for diabetes and don’t make changes, which later may result in pancreatic fatigue, diabetes mellitus, and complications of chronic hyperglycemia. Patients may be in the anger or depression stage and not come to an acceptance of the reality of their disease, which delays improvement and glucose control. Recognizing the stages of valid grief can help you become a more compassionate diabetes educator. Remember, unless you have lived with diabetes yourself, you truly don’t know what it’s like, and compassion and support are some of the best medicines needed by your patients who have diabetes.
Clinical Scenario
Isaiah Brown, a 58-year-old African American man, is resistant to testing his blood sugar daily.
Q: What questions could you ask him to help him move to the next stage of action?
A: Tell me your concerns about testing your blood sugar. What gets in the way when you think of testing your blood sugar? What do you think may happen if you continue to have high blood sugar every day? What are some benefits of testing your blood sugar daily? How many times do you think you need to test your blood sugar? What would you do if you tested and had a high or low blood sugar?
