Infection prevention means breaking the chain of infection or interrupting the infectious disease process. Infections are prevented by:
- Controlling the routes of transmission
- Supporting and protecting the host
- Training and educating healthcare workers in appropriate preventive procedures
To protect themselves and patients from the transmission of bloodborne pathogens, healthcare workers should consider all patients to be potentially infected and act accordingly. This means following Standard and Universal Precautions with all patients.
Preventing the spread of infectious organisms other than bloodborne pathogens includes:
- Early identification of the infectious organism
- Prompt isolation of the patient
- Initiation of appropriate treatment
Routine use of Standard Precautions for all patients suspected of being infectious will reduce the risk of transmission even before a definitive diagnosis can be made and specific precautions based on that diagnosis can be implemented. Patients suspected of having a condition requiring Airborne, Droplet, or Contact Precautions require the use of enhanced precautions while the diagnostic process continues.
When an emergency nurse in Leesburg, Virginia encountered an elderly Chinese patient with atypical pneumonia who had just returned from a trip to China, she immediately placed her in a negative air-flow room and had the staff initiate isolation procedures. She then notified the county health department, who in turn alerted the CDC. Only later did the nurse learn that her quick thinking may have saved many lives.
SARS Coronavirus
The SARS coronavirus mutated to produce the novel COVID-19, which was first discovered in China in 2019. Source: Shutterstock.com.
The elderly Chinese woman was the first U.S. case of severe acute respiratory syndrome (SARS)—documented more than a month before the World Health Organization declared SARS a “worldwide health threat” (Fenwick, 2003).
Certain syndromes and conditions such as SARS carry a sufficiently high risk to warrant Airborne, Droplet, or Contact precautions. For a listing of some of those conditions and the recommendations beyond Standard Precautions, see “Type and Duration of Precautions Needed for Selected Infections and Conditions.”
Specific information about the SARS virus is available here.
Controlling the routes of transmission includes:
- Hand hygiene
- Use of appropriate barriers
- Sterilization or disinfection of patient care equipment
- Isolation or cohorting individuals with communicable diseases and conditions
- Environmental control measures
- Engineering control measures
- Work practice controls
Social Distancing
Social distancing is a preventive measure recommended by public health experts to slow the spread of COVID-19. It is advised that people stay at home as much as possible, going out only for critical needs like groceries and medicines, or to exercise and enjoy the outdoors. Other recommendations include avoiding gatherings of more than 10 people, no handshakes, regular handwashing, and, when encountering someone outside of your immediate household, remaining at least 6 feet apart (i.e., social distancing) (NIH Director’s Blog, March 19, 2020).
Social distancing remains one of our best weapons to slow the silent spread of coronavirus and flatten the curve of the COVID-19 pandemic. This gives our healthcare professionals, hospitals, and other institutions valuable time to prepare, protect themselves, and aid the many people whose lives may be on the line from the 2020 coronavirus pandemic (NIH Director’s Blog, March 19, 2020).
Hand Hygiene
Hand hygiene includes handwashing, antiseptic handwash, antiseptic hand rub, or surgical hand antisepsis. Appropriate hand hygiene is essential to preventing transmission of infection. According to the CDC, handwashing is the single most important measure to reduce the risks of transmitting organisms from one person to another or from site to another on the same patient.
Washing hands as promptly and thoroughly as possible between patient contacts and after contact with body substances, and equipment or articles contaminated by them is a key component of infection control and isolation precautions. Thorough drying of hands is also important as more organisms are transferred by wet hands than from hands that are thoroughly dried.
A wide selection of hand hygiene agents is available to promote safe patient care, including antimicrobial soaps/detergents, rubs, scrubs, and waterless antiseptic agents. According to the CDC (2007, 2019), alcohol-based products are more effective for standard handwashing or hand antisepsis than plain soap or antimicrobial soaps. Recent studies have shown that alcohol-based rinses or gels containing emollients cause substantially less skin irritation and dryness than soaps or antimicrobial detergents.
Factors that influence handwashing efficacy include not only the product used but the frequency and length of time hands are washed. CDC recommends a minimum of 15 seconds and longer if possible; however, research studies show that most healthcare workers wash for less than 10 seconds. Easy access to hand-hygiene supplies, whether sink, soap, medicated detergent, or alcohol-based hand-rub solution, is essential to appropriate hand hygiene.
Hand hygiene also includes attention to fingernails, which can harbor pathogens. Nails should be unpolished and less than ¼ inch long. Chipped nail polish, long nails, artificial fingernails or nail extenders may tear gloves and can harbor pathogens, even after careful handwashing or the use of surgical scrubs.
Barriers
Use of appropriate barriers or personal protective equipment (PPE), such as gloves, gowns, face shields, head covers, masks, also reduces transmission of pathogens. Gloves are the first line of PPE, and can prevent transmission of pathogens and heavy contamination of hands during patient care. However, wearing gloves cannot completely guard against acquiring viral infections, particularly HBV and herpes simplex virus.
Wearing gloves does not replace the need for handwashing because gloves may have small, unnoticeable defects or may tear during use, and hands can become contaminated during glove removal. Hands should always be washed after glove removal particularly if hands are visibly soiled or if the glove has torn. In the absence of visible hand contamination, hand hygiene with alcohol hand rubs is appropriate after glove removal (APIC, 2016).
Gloves should also be changed any time the healthcare worker switches from contaminated to clean tasks, even with the same patient. Disposable gloves should never be washed or decontaminated after use. Sterilization or disinfection of patient-care equipment is fundamental to preventing transmission of pathogens.
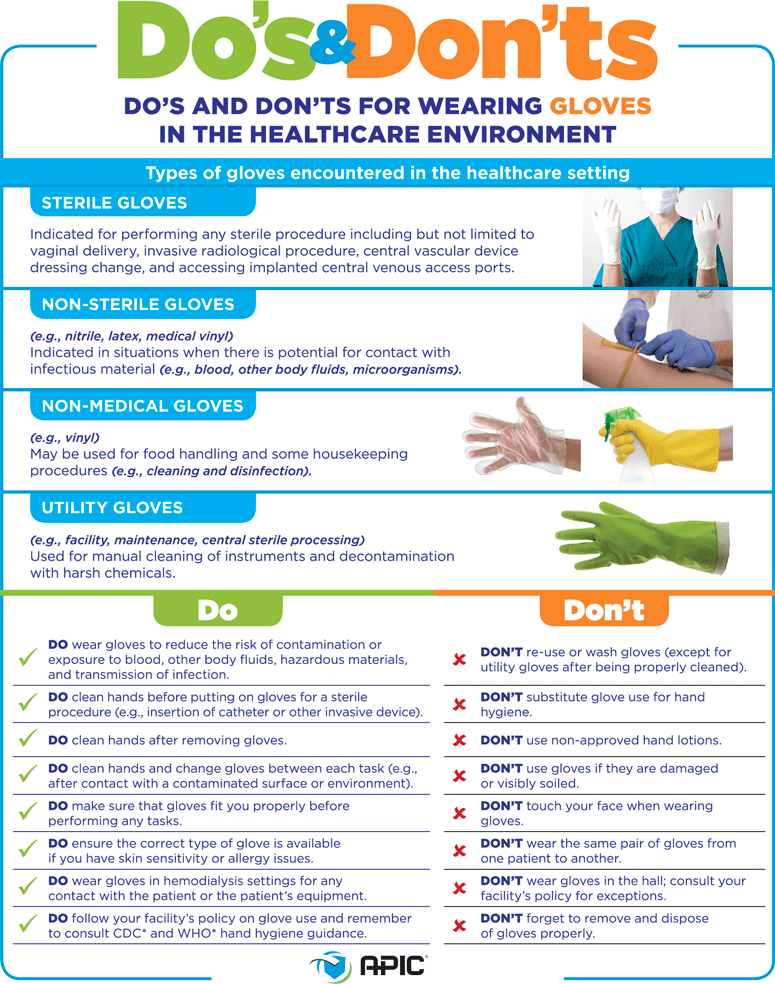
Source: Association for Professionals in Infection Control and Epidemiology. Used with permission.
Sterilization
Sterilization or disinfection of patient care equipment is fundamental to preventing transmission of pathogens. In general, reusable medical devices or patient-care equipment that enters normally sterile tissue or the vascular system or through which blood flows should be sterilized before each use. Sterilization means the use of a physical or chemical procedure to destroy all microbial life, including highly resistant bacterial endospores.
The major sterilizing agents used in hospitals are:
- Moist heat by steam autoclaving
- Ethylene oxide gas
- Dry heat
However, there are a variety of chemical germicides that have been used to reprocess reusable heat-sensitive medical devices and appear to be effective when used according to manufacturer’s instructions. These chemicals are rarely used for sterilization but appear to be effective for high-level disinfection of medical devices that come into contact with mucous membranes during use, such as flexible fiberoptic endoscopes (CDC, 2007, 2019).
Isolating and Cohorting
[Material in this section is taken from CDC, 2007, 2019, unless otherwise cited.]
Isolating or cohorting patients with communicable disease is essential to prevent outbreaks among patients and healthcare providers. Isolation means placing the infected patient in a private room to prevent direct or indirect contact transmission of microorganisms and taking other isolation precautions as appropriate.
Isolation precautions have disadvantages to the hospital, patients, personnel and visitors: specialized equipment and environmental controls increase the cost of care, are inconvenient to healthcare workers, and force solitude for patients. However, these disadvantages must be weighed against the hospital's mission to prevent the spread of serious infection in the hospital.
Isolation is particularly important when the patient has poor hygiene habits, contaminates the environment, or cannot assist in maintaining infection control procedures to limit transmission of microorganisms; this includes infants, children and patients with altered mental status. Whenever possible, the private room should have handwashing and toilet facilities.
If a private room is not available, an infected patient is cohorted, that is, placed with another patient infected by the same microorganism, provided that neither is infected with other potentially transmissible microorganisms. This can be helpful during outbreaks or when there is a shortage of private rooms.
When a private room is not available and cohorting is not achievable or recommended, the healthcare worker should consult an infection control professional before patient placement. If it is necessary for an infected patient to share a room with a non-infected patient, it is important that patients, personnel, and visitors take precautions to prevent the spread of infection and that roommates are selected carefully.
If a patient is suspected of infection with an airborne pathogen, such as the SARS virus, a private room with appropriate air handling and ventilation is critical to reducing the risk of transmission to susceptible patients and other others in the hospital. Some hospitals use an isolation room with an anteroom as an extra measure of precaution. Standard precautions should be followed with all patients, regardless of infection status.
