The American Medical Association has urged healthcare providers to ask patients if they have served in the military and to include that experience in their records. At the request of the American Psychoanalytic Association, the AMA has changed the Current Procedural Terminology [CPT] Evaluation and Management Services Guidelines (Jordan, 2015).
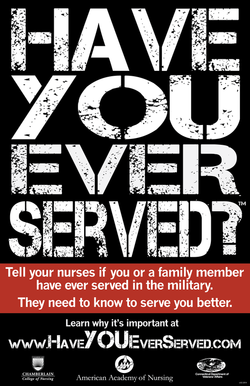
Source: AAN, 2017.
The American Academy of Nursing launched an awareness campaign in 2013 to encourage health professionals to ask patients if they are Veterans or family members of Veterans. This question is not routinely asked by healthcare providers. Only a small percentage of Veterans receive services through the Veterans Administration. Many more Veterans receive healthcare through community providers.
Called “Have You Ever Served in the Military?” and accessed at http://www.haveyoueverserved.com/, the AAN program provides screening and intake questions and information on general areas of concern for all Veterans, such as posttraumatic stress, military sexual trauma, and blast concussions/traumatic brain injury (TBI), as well as health concerns for Veterans of specific conflicts or deployment conditions. The initiative aims to ensure that individuals have appropriate access to services and to increase provider awareness of service-related healthcare issues.
Cheryl Sullivan, CEO of the AAN remarked to a conference of State Directors of Veterans Affairs:
Nurses are healthcare’s equivalent to boots on the ground and are uniquely positioned to facilitate the change and ensure vital information is obtained and recorded so as to improve the healthcare provided to our Veterans and their families (Sullivan, 2013).
Importance of Screening
Assessing Veteran status is not included in traditional behavioral health screenings and a patient might not volunteer this information. Patients may be unwilling to discuss their military status and experiences, particularly if doing so causes mental suffering. Asking patients if they have served in the military has important implications for the available benefits and care. Screening for Veteran status:
- Ensures that each Veteran has access to the network of healthcare and support services he or she is eligible for.
- Informs treatment planning.
- Increases awareness of the strengths that Veterans often possess and the challenges they may face. (Seehusen, 2010)
Finding out if patients have close family members who are Veterans can help providers understand the patient’s family context and determine if the family could benefit from connection to Veteran resources.
Determining Military History
The American Academy of Nursing suggests the following screening questions for determining military service of patients or family members of patients. The initiative to improve the health of Veterans, Have You Ever Served in the Military?, was implemented in all 50 states by April, 2015.
- Have you or has someone close to you ever served in the military?
- When did you serve?
- Which branch?
- What did you do while you were in the military?
- Were you assigned to a hostile or combative area?
- Did you experience enemy fire, see combat, or witness casualties?
- Were you wounded, injured, or hospitalized?
- Did you participate in any experimental projects or tests?
- Were you exposed to noise, chemicals, gases, demolition of munitions, pesticides, or other hazardous substances?
- Have you ever used the VA for healthcare?
- When was your last visit to the VA?
- Do you have a service-connected disability or condition?
- Do you have a VA primary care provider? (AAN, 2017)
Common Military Health Risks Nurses Should Know
- Radiation Exposure/Nuclear Weapons (WWII: Amchitka, Alaska, Hiroshima, Nagasaki, POW in Japan; Korea; sub-mariners exposed to nasopharyngeal radium treatment; Gulf Wars; Bosnia; Afghanistan): High risk for cancer.
- Agent Orange Exposure (Korea, Vietnam): High risk for cancers (including respiratory and prostate cancer), chloracne, type 2 diabetes, ischemic heart disease, soft tissue sarcoma, peripheral neuropathy, spina bifida in Veterans’ biological children.
- Camp Lejeune Water Contamination (January 1, 1957–December 31, 1987): Veterans and families stationed at Camp Lejeune exposed to chemical contaminants in the groundwater and wells are at risk for the following cancers (bladder, blood dyscrasia, breast, esophageal, kidney, leukemia, lung, multiple myeloma, myelodysplastic syndromes, non-Hodgkin’s lymphoma) and conditions (female infertility, hepatic steatosis, miscarriage, renal toxicity, scleroderma).
- Hepatitis C (Vietnam): Transfusions prior to 1992, battlefield exposures to blood and human fluids, group use of needles, razors, toothbrushes, and other personal items.
- Exposure to Open Air Burn Pits (Vietnam, Iraq, Afghanistan): High risk for respiratory illnesses and wide variety of cancers, including leukemia.
- Gulf War Syndrome (Gulf Wars): Characterized by fibromyalgia, chronic fatigue syndrome, headaches, gastrointestinal problems, cognitive impairment and pain, high rates of brain and testicular cancers, and neurodegenerative diseases (ALS, MS).
- Depleted Uranium (Gulf Wars, Bosnia, Afghanistan): Inhaled or ingested microfine particles (heavy metal toxicity). Risk for respiratory and kidney diseases.
- Infectious Diseases (Iraq & Afghanistan): Malaria, typhoid fever, viral hepatitis, leishmaniasis, TB, rabies resulting from animal bites. (AAN, 2017)
Good Clinical Practice in Caring for Veterans
Healthcare providers can recognize and successfully address the physical, mental, and emotional health of Veterans. Good clinical practices include the following:
- Thank the Veteran for his or her service.
- Ask about traumatic experiences (specifically ask about sexual trauma).
- Listen to the Veteran’s story.
- Validate the Veteran’s feelings about common trauma reactions.
- Screen for PTSD symptoms.
- Identify concern for the patient and emphasize the need for follow-up.
- Screen for suicidal ideation.
- Refer the Veteran to an appropriate healthcare professional for complete evaluation and treatment recommendations.
- Arrange for a follow-up assessment and health teaching (Rossignol, 2010).
