4.1 Trauma
Trauma is the result of experiencing a frightening, dangerous, or violent event that poses a threat to an adult or child’s life, safety, or bodily integrity. Witnessing a traumatic event that threatens the life or physical security of a loved one can also be traumatic. This is particularly important for young children as their sense of safety depends on the perceived safety of their parents of caregivers.
Traumatic experiences often initiate strong emotions and physical reactions that can persist long after the event. Children may feel helplessness, fear, and physiological reactions such as heart pounding, vomiting, or loss of bowel or bladder control. Children who feel unable to protect themselves or who lack protection from others to avoid the consequences of the traumatic experience may also feel overwhelmed by the intensity of physical and emotional responses (NCTSN, nd).
4.1.1 Complex Trauma
Complex trauma describes both a child’s exposure to multiple traumatic events—often of an invasive, interpersonal nature—and the wide-ranging, long-term effects of this exposure. Abuse or profound neglect are severe and pervasive especially when they occur early in life. They can disrupt many aspects of the child’s development and the formation of a sense of self. Since these events often occur with a caregiver, they interfere with the child’s ability to form a secure attachment. Many aspects of a child’s healthy physical and mental development rely on this primary source of safety and stability (NCTSN, nd).
4.1.2 Early Childhood Trauma
Early childhood trauma generally refers to the traumatic experiences that occur to children aged 0-6. Because an infant’s or young child’s reactions may be different from those of older children, and because they may not be able to verbalize their reactions to threatening or dangerous events, many people assume that young age protects children from the impact of traumatic experiences (NCTSN, nd).
A growing body of research has documented that young children can be affected by events that threaten their safety or the safety of their parents or caregivers. These traumas can be the result of intentional violence—such as physical or sexual abuse, domestic violence, or the result of natural disasters, accidents, or war. Young children may also experience traumatic stress in response to painful medical procedures or the sudden loss of a parent or caregiver (NCTSN, nd).
4.1.3 Historical Trauma
Trauma due to systemic racism and discrimination, the impact of multigenerational poverty, and limited educational and economic opportunities intersect and exacerbate adverse childhood experiences. Historical power imbalances have had a profound effect on certain racial and ethnic groups: early deaths, unnecessary disabilities, and enduring injustices and inequalities (Global Health 50/50, 2020).
Structural racism is rooted in a hierarchy that privileges one race over another, influencing institutions that govern daily life, from housing policies to police profiling to incarceration (Muramatsu and Chin, 2022). Over centuries, structural racism has become entrenched, influencing the way medicine is taught and practiced as well as the functioning of healthcare organizations (Geneviève et al., 2020).
The unequal burden of COVID-19 on underserved populations has forced the medical community to reckon with uncomfortable truths about its role in perpetuating structural racism in modern society. A race-conscious conversation in medicine is evolving that acknowledges race as a social construct that creates and upholds barriers underlying health disparities (Santos, Dee, and Deville, 2021).
4.2 Adverse Childhood Experiences (ACEs)
Adverse childhood experiences, or ACEs, are preventable, potentially traumatic events that occur in childhood. These experiences can be caused by neglect, experiencing, or witnessing violence, or having a family member attempt suicide or die by suicide. Abuse and neglect, substance use, family members with mental health problems, parental separation or incarceration, and household violence can also undermine a child’s sense of safety, stability, and bonding (NCTSN, nd).
These experiences, and their negative impact on health over time—including the intersection of ACEs, suicide, and overdose—are interrelated and preventable. Living in under-resourced or racially segregated neighborhoods, frequently moving, being subjected to homelessness, or experiencing food insecurity can be traumatic and exacerbate the effects of other ACEs (NCTSN, nd).
Adverse childhood experiences are common across all socioeconomic groups. Children who have been subjected to a higher number of adverse events, particularly in the absence of protective factors, are more likely to experience ongoing trauma, negative health outcomes, and increases in chronic health conditions such as obesity, diabetes, and heart disease.
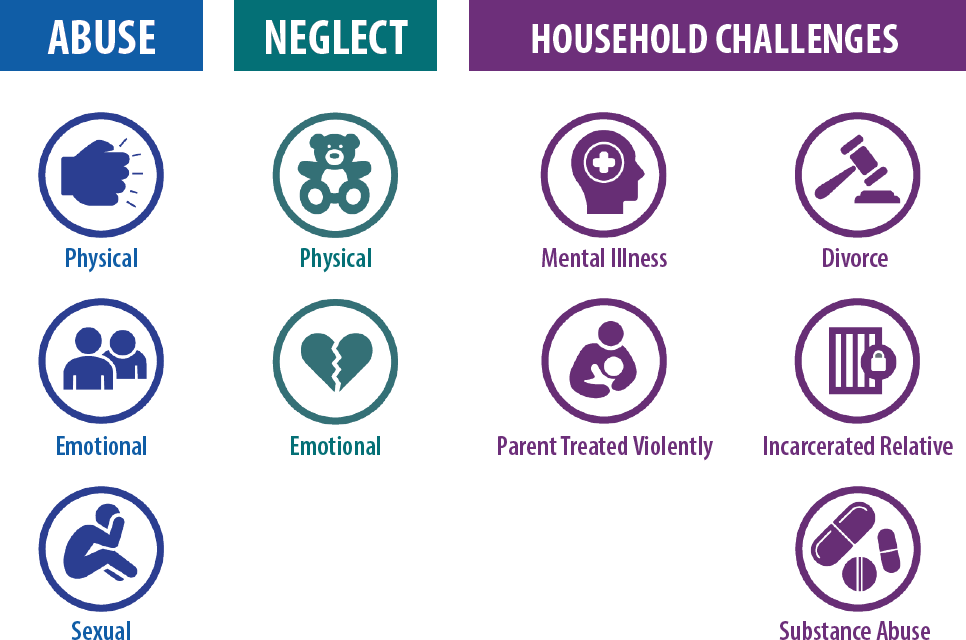
Source: CDC, Public Domain.
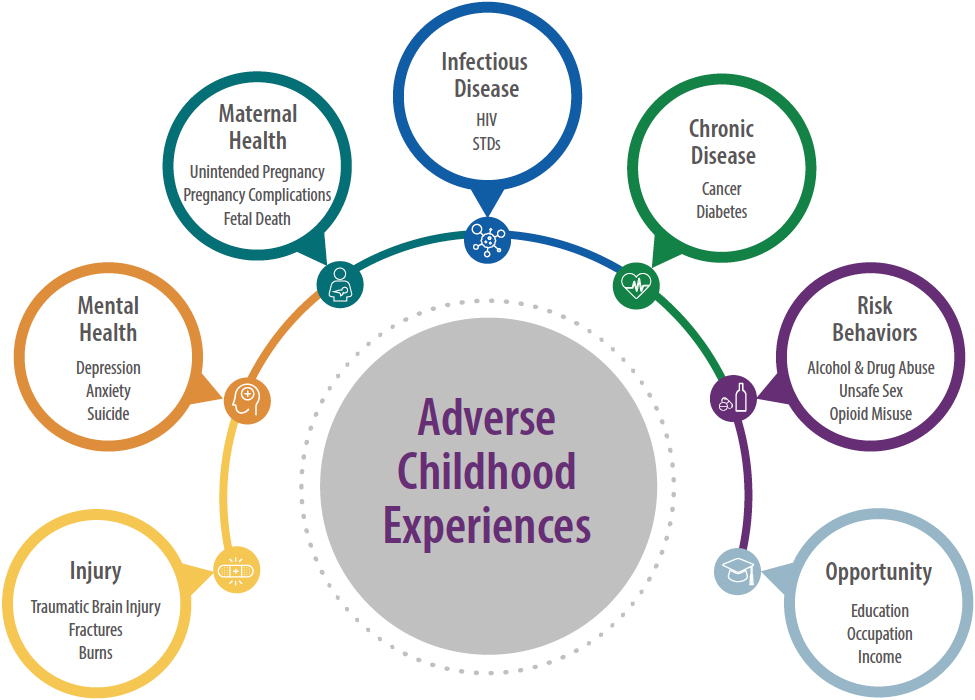
Source: CDC, Public Domain.
4.3 Trauma Informed Practice
Trying to implement trauma-specific clinical practices without first implementing trauma-informed organizational culture change is like throwing seeds on dry land.
Sarah Bloom, MD
Advancing Trauma-Informed Care
Trauma-informed practice is a model for engaging with individuals and families that recognizes the impact and influence that trauma may have on the individuals and families you serve. An important part of a trauma-informed practice is to avoid the inadvertent re-traumatization of individuals through your own interactions with them and to understand that trauma may have an impact on a person’s behavior.
4.3.1 Key Elements of Trauma-Informed Practice
Including the patient in all treatment decisions is a key element of trauma-informed care. Additional key elements include:
- Screening for trauma
- Training staff in trauma-specific care
- Creating a safe environment
Trauma-informed practice assists you in identifying when your own past experiences or trauma may impact the way you evaluate an incident you encounter in your professional role.
4.3.2 Protective Factors
In the past, child maltreatment prevention and intervention strategies have focused on eliminating risk factors—conditions, events, or circumstances that increase a family’s chances for poor outcomes. This emphasis on family risks, such as maternal depression, family violence, or history of maltreatment often left families feeling stigmatized or unfairly judged (CWIG, 2020).
A “protective factors approach” to the prevention of child maltreatment focuses on positive ways to engage families by emphasizing their strengths. It focuses on what parents and caregivers are doing well by identifying areas where families have room to grow with support (CWIG, 2020).
A protective factors approach includes strategies to mitigate the long-term consequences of adverse experiences by:
- Strengthening economic supports for families.
- Promoting social norms that protect against violence and adversity.
- Ensuring a strong start for children.
- Enhancing skills to help parents and youths handle stress, manage emotions, and tackle everyday challenges.
- Connecting youths to caring adults and activities.
- Intervening to lessen immediate and long-term harms.
Using this approach, agencies can build capacity and partnerships with other service providers—such as early-childhood and youth-service systems—that are likely to enhance support for children and families and promote their well-being. Children, youth, and families can build resilience and develop skills, characteristics, knowledge, and relationships that offset risk exposure and contribute to both short- and long-term positive outcomes (CWIG, 2020).
Families, communities, practitioners, and advocates can help foster social and emotional competencies at the individual, family, and community levels. These strategies help children who experience adversity develop resilience and skills. Adverse childhood experiences can be mitigated by positive childhood experiences, and more children can have healthy environments in which to play, learn, and grow into mentally, emotionally, and physically healthy adults (CWIG, 2020).
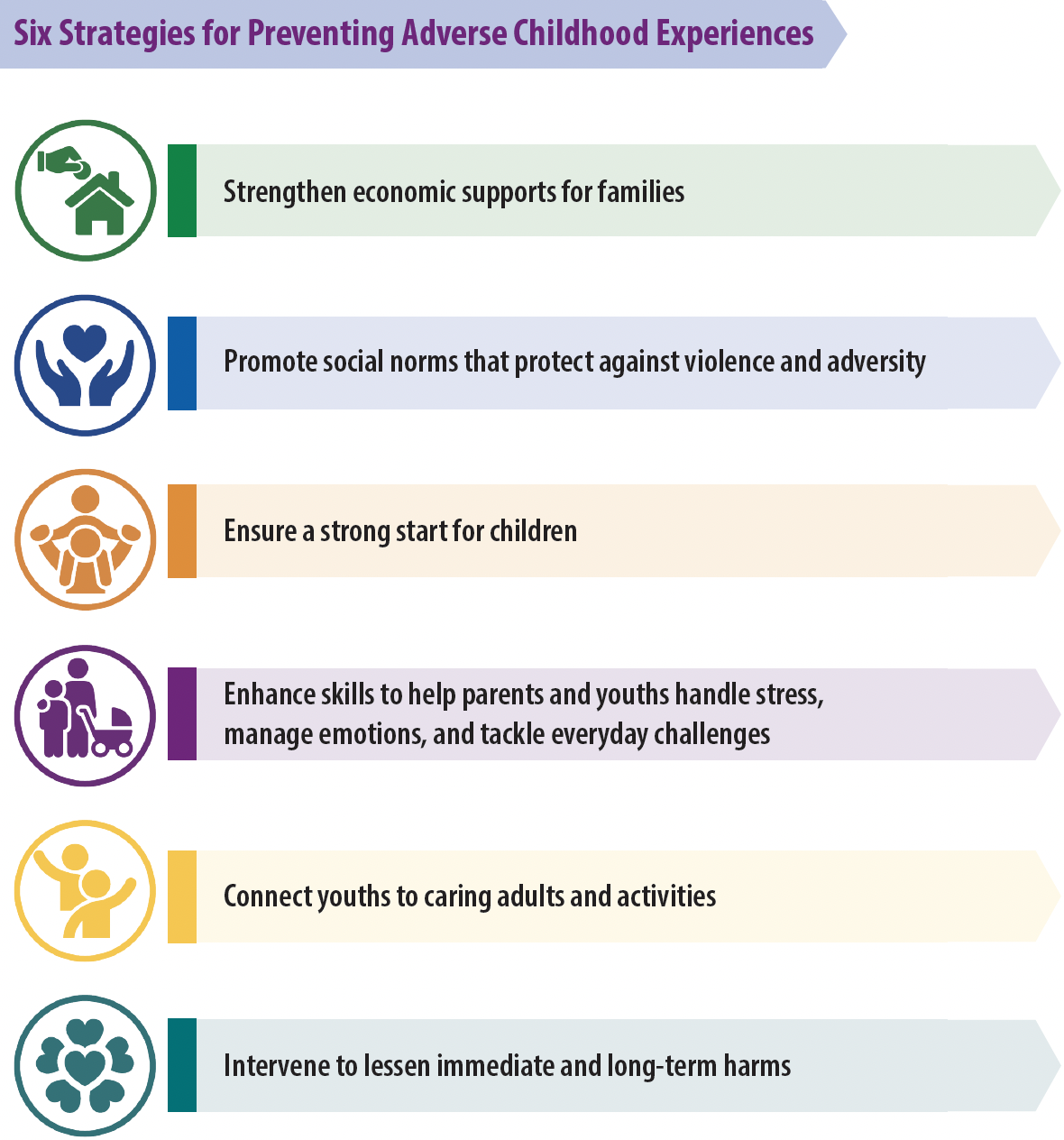
Source: CDC, Public Domain.
