Difficulties related to communication are among the earliest symptoms of dementia and tend to worsen as the disease progresses. Difficulty with word finding, replacing a word with an unrelated word, or not finding a word at all often occurs in the early stage. As the disease progresses, forgetting names of family members and friends, confusion about family relationships, and loss of the ability to recognize family members is not uncommon.
Losing the ability to communicate is both social and relational. Needs go unmet and social interactions gradually become more stressful and tiring. This can cause frustration, conflict, and depression and may lead to earlier placement in a care facility. Dementia reduces a person’s ability to communicate effectively, which make is more difficult for caregivers to identify the needs of the person they are assisting (Pham et al., 2015).
Location of the hippocampus. Source: Image courtesy of the National Institute on Aging/National Institutes of Health. Public domain.
Communication changes are related to the area of the brain affected by the disease. In Alzheimer’s, damage begins in a part of the brain that is responsible for the formation of new, short-term memories, called the hippocampus. This means a person does not remember the “what, where, and when” of recent events—what they ate yesterday, where they went 2 days ago, and the date of their next doctor’s appointment. Located next to the hippocampus is a part of the brain called the amygdala, which is involved with emotional control. As short-term memory declines, emotional control also weakens, further affecting a person’s ability to communicate effectively.
In frontal-temporal dementia, damage begins in the front part of the brain. Because of the location, memory is (initially) less affected than in Alzheimer’s disease. This is because the front part of the brain is responsible for traits that allow us to function in society: judgment, planning, moral reasoning, logical thinking, and social behavior. Although these functions are affected by a person’s memories, the brain changes caused by frontotemporal dementia affect judgment, moral reasoning, and social control. As a result, a person may become more impulsive, make sexual comments or socially inappropriate remarks, and gradually lose the ability to make decisions.
In general, communication can be fraught with misunderstanding, frustration, and surprise—even for people without cognitive decline. A person experiencing cognitive decline due to frontal-temporal dementia gradually losses decision-making abilities, has difficulties with sequencing a task, is unable to explain or understand complex ideas, and loses the ability to communicate through written and spoken words. Because there is a loss of judgment and social control, caregivers and family members may be faced with embarrassing moments in public that can include inappropriate comments and behaviors.
So instead of losing short-term memory like people with Alzheimer’s disease, a person with frontal-temporal dementia might start behaving in a way that is confusing to their friends and family. They might steal, even though they have never stolen in the past. They might make inappropriate sexual remarks or engage in inappropriate sexual behaviors, even though they have never done these things in the past.
In vascular dementia, damage is caused by impaired blood flow to the brain. Cognitive changes can be widespread and not necessarily associated with a specific part of the brain. As a result, communication problems are usually less specific than in other types of dementia. There may be a slowness of thought, problems with attention and concentration, and difficulties with language. Complex, fast-paced conversations or quick changes in topic may be difficult to follow.
Vascular dementia can cause mood changes that are stronger than the mood changes you might see in someone with Alzheimer’s. It can also affect judgment—but not as strongly as in someone with frontal-temporal dementia. It can be difficult to differentiate vascular dementia and Alzheimer’s dementia because they can occur together. Cognitive changes can be gradual or occur in noticeable steps downward from a person’s previous level of function.
In Lewy body dementia, abnormal clumps of alpha-synuclein (Lewy bodies) form throughout the cortex, brainstem, and midbrain. The location of these clumps influences the symptoms, which vary from person to person. A person with Lewy Body dementia can experience paranoia, delusions, and hallucinations (usually visual), which are very real for the person experiencing them. Arguing, explaining, agreeing, or validating the paranoia or delusion is usually ineffective. Emotional support, quiet touch, and redirection are more effective than verbal communication.
Areas of Brain Associated with Communication
Certain parts of the brain are responsible for speech and language. These areas are mainly located in the left side of the brain. These brain regions and their connections form a network that provides the hardware for language in the brain. Without this network, we would not be able to talk to or understand others (Brauer, 2014).
The loss or decline of language and communication skills is called aphasia. This is an acquired language disorder that affects a person’s ability to comprehend and produce language. People with aphasia have trouble expressing themselves, finding the right words, understanding the words they are hearing—and also, have difficulty with reading and writing. Aphasia is a common symptom in a person with a stroke that affects the left side of the brain.
Wernicke’s aphasia is caused by damage to the left temporal lobe. It is sometimes referred to as fluent aphasia because a person can speak but the words carry no meaning.
Broca’s aphasia is caused by damage to the left frontal lobe. It is sometimes referred to as non-fluent aphasia because a person’s speech is short and choppy. Global aphasia is a combination of Wernicke’s and Broca’s aphasia in which a person is unable to understand the spoken word or communicate with speech.
Speech and Language Areas of the Brain
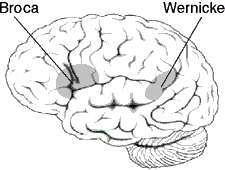
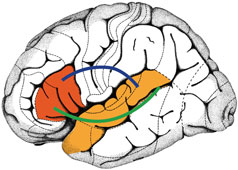
Left: Areas of the left side of the brain associated with processing speech and language. Source: Wikimedia Commons. Used with permission. Right: Broca’s and Wernicke’s brain regions are highlighted in red and orange. The blue and green lines illustrate connections that link the two regions with one another and form a network of language areas. Frontiers for Young Minds. Reprinted with permission.
Communication is also related to our emotions. An area of the brain located close to the hippocampus called the amygdala is involved with emotions, particularly emotional behavior, learning, and motivation. Damage to this part of the brain can affect a person’s ability to read facial emotions as well as their ability to control their own emotions. Damage to the amygdala can affect a person’s ability to understand when another person is frustrated, angry, or even happy. This likely affects a person’s ability to follow non-verbal facial cues.
How Dementia Affects Communication
Dementia affects our ability to communicate, as well as our ability to comprehend what others are trying to communicate. As dementia progresses, there is:
- A loss of ability to find the right word
- A tendency to describe objects rather than naming them
- An inability to finish sentences or express cohesive thoughts
- The loss of train of thought
- A tendency to revert to language of origin
- The need for longer periods of time to respond (Zeman, 2015)
A person with dementia:
- Has difficulty finding a word
- Creates new words for ones that are forgotten
- Repeats a word or phrase (perseveration)
- Has difficulty organizing words into logical sentences
- Curses or uses other offensive language
- Reverts to their original language
- Talks less than usual (Alzheimer’s Society of Canada, 2019)
Managing Communication Challenges
Caregivers may fail to understand that good communication is a learned skill. Poor communication increases confusion and stress for the person with dementia and can also cause confusion and stress for the caregiver. The ability to communicate with people whose speech or hearing is impaired by cognitive decline is a skill that can be developed with practice. Several therapeutic interventions have been developed to work directly with people with dementia on an individual or group basis, and also indirectly with family and professional caregivers, to improve communication and quality of life for people with dementia (Pham et al., 2015).
Direct, simple phrases are recommended. Appropriate touch can signal the start of a conversation or a change in topic. Nonverbal cues such as simple hand signals can be helpful. Well-designed, meaningful individual or group activities can improve communication skills. The focus of group activities is on improving or maintaining functional skills, including communication.
A Physical Therapist Uses Sign Language
When I was younger, I took several classes in American Sign Language at the local community college. After graduating from PT school, I started working in stroke rehab and noticed that the signs I learned were helpful when communicating with people who were experiencing language deficits following a stroke. It didn’t take me long to realize that simple signs also worked well for people in various stages of cognitive decline. Using simple, nonverbal cues was relaxing for me—it was quiet, direct, and successful!
Bella, PT, Miami
How you talk to a person influences how they respond. Techniques that improve communication and reduce agitation, confusion, fear, or anxiety include:
- Approaching from the front or side and sitting or kneeling at eye level
- Assessing a person’s body language
- Monitoring your body language, facial expression, and tone of voice
- Introducing yourself each time and explaining what you are doing and why
- Making sure the person with dementia can clearly see you
- Reducing distractions
- Speaking slowly and clearly using short sentences
- Allowing extra time for a response (Zeman, 2015)
Communication habits of the caregiver affect the success or failure of interactions with a person experiencing cognitive changes. Poor communication can be a major driver of behavioral symptoms and increase agitation, confusion, fear, and anxiety. Communication habits to be avoided include:
- Speaking “down” to a person
- Using infantilizing words: “she’s just like a baby”
- Using complex or lengthy explanations
- Speaking too quickly
- Speaking in an impatient voice
- Failing to allow time for the person to process what you are trying to communicate
- Rushing through any activity (Gitlin & Vause Earland, 2010)
Hallie Is Scared
Introduction: As many as two-thirds of stroke patients experience cognitive impairment or cognitive decline following a stroke; approximately one-third go on to develop dementia. This may be inadvertently overlooked because, following a stroke, the emphasis is often on recovery of functional abilities such as walking and activities of daily living.
Client Information: Hallie is 90-years old woman who moved from Phoenix to live with her daughter in Santa Rosa, California following a brainstem stroke. She is struggling with mobility and also having difficulty expressing her needs. She refuses to participate in any activities.
Prior to suffering the stroke, she lived independently in Mesa, Arizona with her alcoholic son. In the hospital she was given a feeding tube due to swallowing problems. When she arrived in California, she was able to walk a few steps with a walker and needed a great deal of assistance with transfers, toileting, and bathing. For more than a year after moving she was unable to name the town or even what state she was living in. She was, however, able to read and write and her vision was good enough to read the captions on the TV.
Now, almost 2 years after her stroke, Hallie is off her feeding tube, eating independently and enthusiastically, coloring intricate patterns in a coloring book. She is transferring and bathing with much less assistance. She is still unable to walk and has difficulty with memory and recall.
Timeline: Because of her improvement, Hallie’s daughter feels her mother might enjoy the local adult day care program. The first time they attend, Hallie is withdrawn and refuses to participate in any activities—even drawing. The activities director, Celana, tries to engage Hallie in a conversation but she just smiles and asks where her mother is. Celana asks Hallie to tell her about her mother but she doesn’t (or can’t) answer. When Hallie’s daughter comes to pick up her mom the day care center administrator reports that Hallie didn’t participate in any activities and wouldn’t budge from her recliner—even to use the bathroom. Celena feels that, with some gentle encouragement, Hallie will begin to participate in activities. She reports her observations and concerns to the facility administrator.
Intervention: The staff discuss Hallie’s situation after the center closes that evening. The administrator asks Jenitra, a registered nurse, to assess Hallie in the morning—to spend some time with her and try to draw her out. Hallie’s daughter is a nurse and the administrator rightly thinks that Hallie may be comfortable talking to a nurse. When Hallie arrives the next day, Jenitra, using her dementia-specific training, approaches Hallie from the front, introduces herself, sits beside her, and offers her hand, which Hallie takes. She asks about Hallie’s daughter and says that she too is a nurse. She tries to engage Hallie in a general conversation without success.
Hallie is very quiet and seems confused. She asks Jenitra where she is and again asks for her mother. Jenitra makes sure Hallie is comfortable, quietly assesses her hearing and vision, and makes sure Hallie is able to understand English. Finally, after some quiet back and forth, Hallie admits that she’s scared. Jenitra asks her why and she says she is scared because she can’t remember things. This provides staff members with the information they need to design activities that will help Hallie feel more comfortable at day care.
Discussion: It is normal for a person to feel uncomfortable in a new social situation. This is especially true for a person with memory problems. Hallie is new to adult day care, in a new living situation, and new to California. The transition has been difficult for her. The staff acknowledge Hallie’s fears and make sure to support and educate Hallie’s family caregivers.
Hallie has many positive things going for her, considering the severity of her stroke. Her vision is good, she has a good sense of humor, she enjoys drawing, and she eats just about anything you put in front of her. Staff members learn that Hallie isn’t fond of physical activity but is able to concentrate on her intricate drawings for long periods of time. She also likes TV. They design a program of activities that focuses on art, drawing, and painting. They encourage her to participate in the exercise class, which she does reluctantly. Eventually, the activities director realizes that Hallie does better with one-on-one exercise.
Client Perspective: Hallie tells her daughter that she doesn’t want to go to “that place” although she isn’t able to articulate what she means. Her daughter is able to encourage Hallie to go again, telling her that they are having hamburgers for lunch. Hallie says she is OK with that and agrees to attend adult day care again.
