Proper and accurate documentation protects you in the event there may be skin breakdown or a caregiver challenges the accuracy or occurrence of education. Documentation protects your licensure and provides the caregiver with assurance that all appropriate steps have been taken to provide high-quality patient care, should it come in question.
Did You Know. . .
Partial thickness and full thickness are used to describe any wound that is not a pressure injury.
Such wounds can occur from a skin tear, trauma, surgery, or an unknown reason. Partial thickness wounds show tissue loss that extends below the epidermis and into but not through the dermis. They are shallow and usually heal by epithelialization. Partial thickness wounds are moist and painful because of the loss of the epidermal covering and the resultant exposure of nerve endings (Bryan & Nix, 2015). A full thickness wound exhibits tissue loss that extends below the dermis and into the subcutaneous tissue and fascia, possibly exposing the bone. These wounds usually heal by granulation, contraction, and re-epithelialization. Treatment of both wounds depends upon the depth of damage, drainage, risk of infection, and wound bed appearance.
Documenting Wound Etiology
If you are unsure of wound etiology, document it as partial or full thickness and treat according to tissue damage until identification of the wound cause is determined, which will assist in classification.
When documenting a wound, start with the location of the wound as defined by the anatomical man. If the wound is a pressure injury, describe the stage of the wound. Then describe the wound bed as to granulation tissue, slough, black eschar, epithelialization, and so on. The color of the tissue in the wound bed should be included: pink, red, yellow, or pale. The size of the wound, measured most often in centimeters, is then documented, with the length always going head to toe and the width always hip to hip. Do not measure the wounds at their greatest lengths and widths (as was done in the past). Measure perpendicularly (straight up and down and side to side) based off the patient’s head, feet, and hips.
Depth of wound is determined by inserting a moist swab into the wound at a 90-degree angle until the tip touches the base of the wound. Mark the point on the swab when it is level with the wound surface to determine depth. To measure undermining and tunneling, which can be seen in Stage 3 and Stage 4 wounds, the face of the clock is used to assist in description. For example, a wound can be described: wound bed 3 cm x 4 cm x 4 cm with undermining from 3 to 7 o’clock with greatest depth of 3 cm at 4 o’clock. Tunneling noted at 10 o’clock of 6 cm.
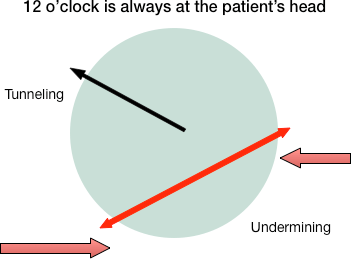
Wound description would say: Wound bed with undermining from 3 to 7 o’clock with greatest depth at 10 o’clock with depth of 6 cm.
The type and amount of exudate must be included in documentation (serous, serosanguinous, purulent) as well as any odor present.
Peri-wound assessment documentation consists of excoriation, tenderness, edematous, induration, erythema, rash, and maceration. Assessment of the periwound allows clinicians to decide if breakdown is likely to occur and to help prevent further complications. Wound edges can be documented as attached, detached, rolled, intact, thickened, or punched out. The appearance of the wound edges alerts you as to whether continuous pressure or trauma is being applied to the wound.
Describe any signs or symptoms of infection and notice if the area is painful to the touch or if there is generalized pain. Note and describe edema and, when the wound is on the lower extremity, assess bilateral pulses with palpation. The more thorough your documentation, the better you help other healthcare providers understand the cause and progression, or deterioration, of the wound.
It is important to update your education for the caregiver, observe how patient and caregiver interact during the visit, answer any questions asked, examine shoe and cushion selection, and note any new incidents that occurred since the last visit or assessment. Wound care is problem solving, and the more pieces of the puzzle you provide, the more complete picture you give as a basis for prevention and treatment.
