Obviously, there is a bit of an anti-science trend in the United States, a pushing back on authority telling you what to do. Sometimes, in a good vein, that could be the independent spirit of the American people. That is part of our character. But on the other hand, it can work against you. And when you push back on someone telling you what to do, and you mix that with a trend of anti-authority, anti-science, then you get into trouble. Then you get into the situation we find ourselves now, where people are not acting in a way that is safeguarding their health.
Dr. Anthony S. Fauci, M.D. Wired, July 29, 2020 Anthony Fauci Explains Why the US Still Hasn't Beaten COVID
This is a big fucking deal. If I would not be excommunicated from the world of science, I would call this an evil virus, but I can’t do that because I can’t impugn motives to it. But if I could, I would call it that. It’s certainly pernicious. This is the worst pandemic in our lifetime. And it is the first time we have had a pandemic in the United States in which we have had such a total, abysmal failure of our federal government.
Dr. Larry Brilliant Wired, July 9, 2020 On How Well We Are Fighting Covid-19
When I ask [Larry David] if he is hoarding anything, he is outraged. “Not a hoarder,” he said. “In fact, in a few months, if I walk into someone’s house and stumble onto 50 rolls of toilet paper in a closet somewhere, I will end the friendship."
Maureen Dowd, New York Times, April 4, 2020 Interview with Larry David, Master of His Quarantine
An outbreak of a novel and sometimes deadly respiratory disease in China grew rapidly in the first months of 2020. The illness has since spread around the world with sustained person-to-person transmission on six continents. As of September 14, 2020, there are more than 29,000,000 confirmed cases and nearly 926,000 deaths worldwide in this swiftly expanding pandemic. The United States continues to lead the world with ~22% of global infections and more than 20% of global deaths.
In December of 2019, a cluster of viral pneumonia cases was reported in Wuhan City, Hubei Province, China. In January of 2020 a novel coronavirus, believed to have originated in a live animal market, was identified as the causative agent of the pneumonia. The virus, temporarily named 2019-nCoV but now called COVID-19 (which stands for coronavirus disease-2019), caused a widespread epidemic throughout China, with many exported cases that became the seeds for the global spread of the easily transmissible virus.
Chinese health officials reported tens of thousands of coronavirus cases in that country and took the unprecedented measure of quarantining nearly 60 million people. Despite the massive quarantines, the virus still spread beyond China’s borders and was soon spreading person-to-person in many parts of China and other parts of the world (NIH, 2020a).
The United States reported its first confirmed instance of person-to-person spread on January 30, 2020. On the same day, the World Health Organization (WHO) declared the novel coronavirus outbreak a public health emergency of international concern. “The main reason for this declaration is not because of what is happening in China but because of what is happening in other countries. Our greatest concern is the potential for the virus to spread to countries with weaker health systems, which are ill-prepared to deal with it,” WHO Director-General Tedros Adhanom Ghebreyesus said (CNN, 2020a).
“A public health emergency of international concern” is an event that poses a global health risk that may require a coordinated international response as happened with Ebola, Zika, and H1N1 (CNN, 2020a).
On January 31, the United States declared a public health emergency to aid the nation’s healthcare community in responding to COVID-19 and the President of the United States signed a presidential “Proclamation on Suspension of Entry as Immigrants and Nonimmigrants of Persons who Pose a Risk of Transmitting 2019 Novel Coronavirus” (CDC, 2020b). On March 13, 2020, a national health emergency was declared in the United States.
“The goal of the measures we have taken is to slow the introduction and the impact of the disease in the United States,” said Nancy Messonnier, director of the National Center for Immunization and Respiratory Diseases (CDC, 2020c).
Despite measures taken to slow the entry and spread of COVID-19 in the United States and other countries, as of February 26, 2020 there were more confirmed COVID-19 cases outside of China than inside China (CNN, 2020a). On March 11, 2020, the World Health Organization (WHO), declared the novel coronavirus a global pandemic.
On March 26, 2020, the United States surpassed China to become the country with the most confirmed cases of COVID-19. “Scientists warned that the United States someday would become the country hardest hit by the coronavirus pandemic. That moment arrived Thursday” (NY Times, March 27, 2020).
Global Epidemiology
The number of confirmed COVID-19 cases as of September 14, 2020 include:
- Globally, there are 29,145,068 confirmed cases
- Total deaths: 925,947
Source: Center for Systems Science and Engineering, Johns Hopkins University, September 14, 2020.
United States Epidemiology
The number of confirmed COVID-19 cases as of September 14, 2020 include:
- Total confirmed cases: 6,550,629
- Total test results in the United States: 88,831,535
- Total deaths: 194,411
Source: Center for Systems Science and Engineering at Johns Hopkins University, September 14, 2020.
Graphs of Confirmed COVID-19 Cases and Deaths in the United States
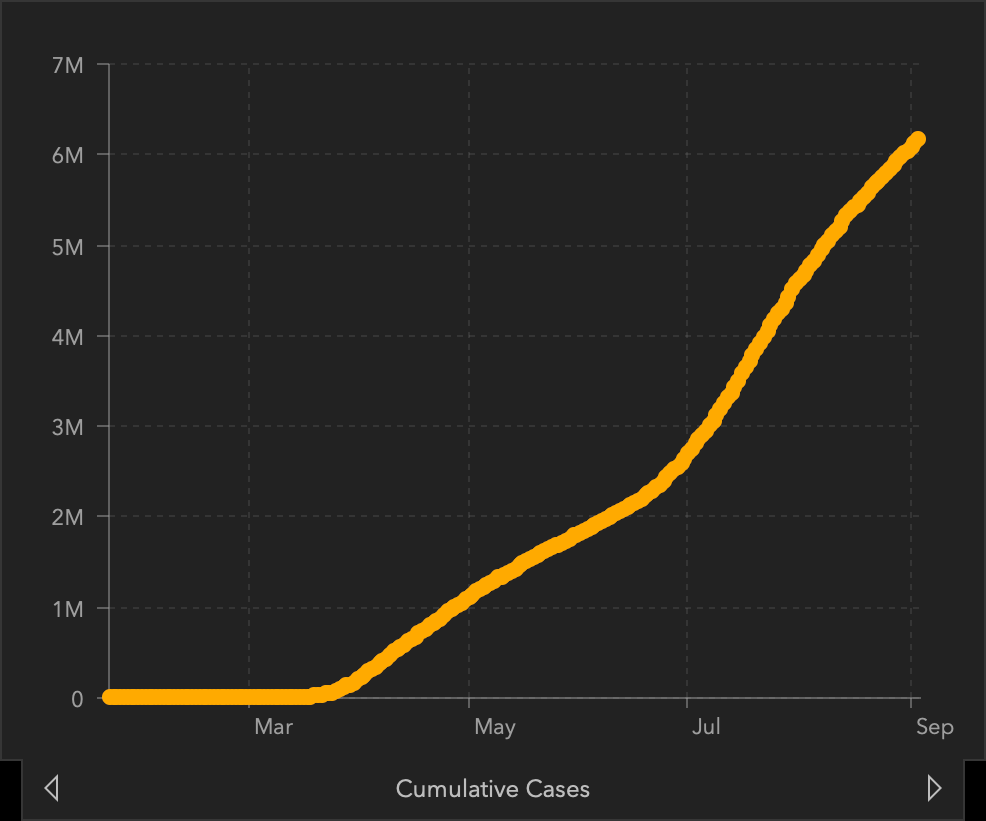
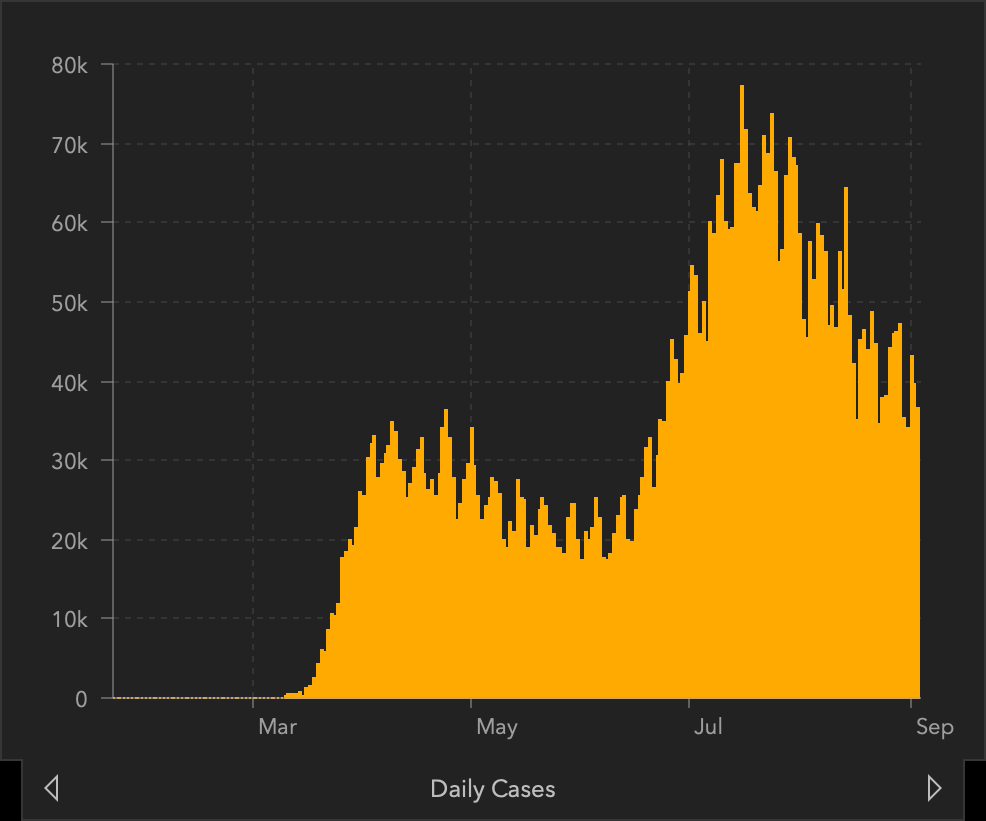
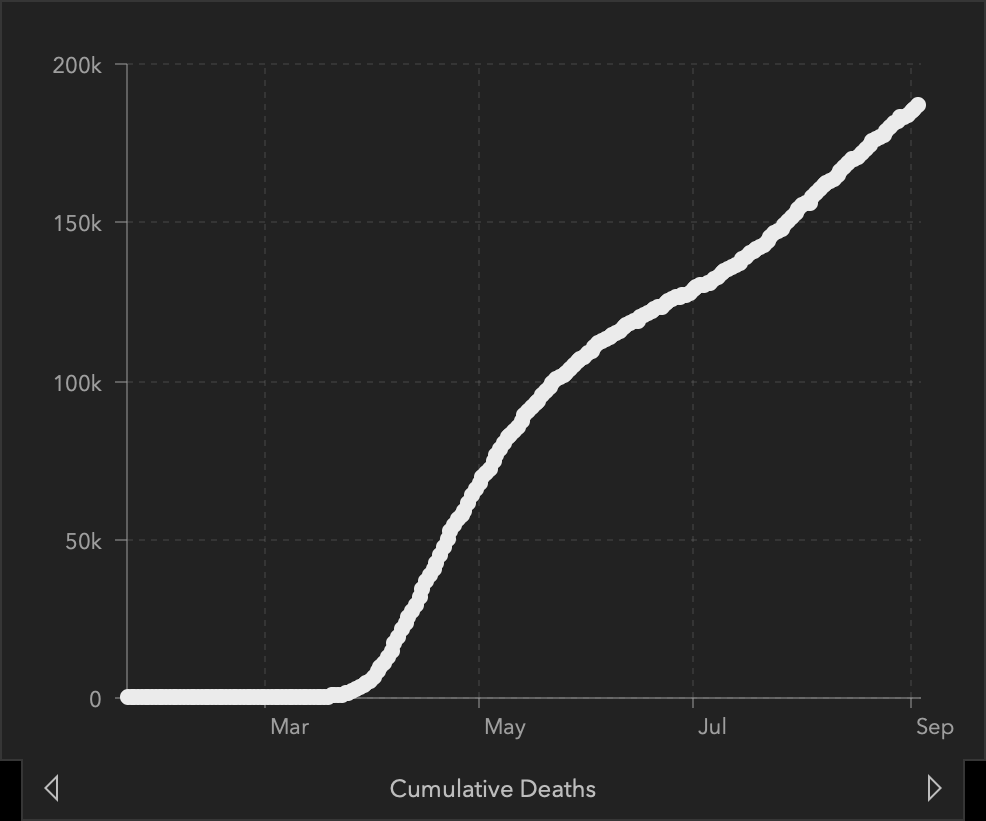
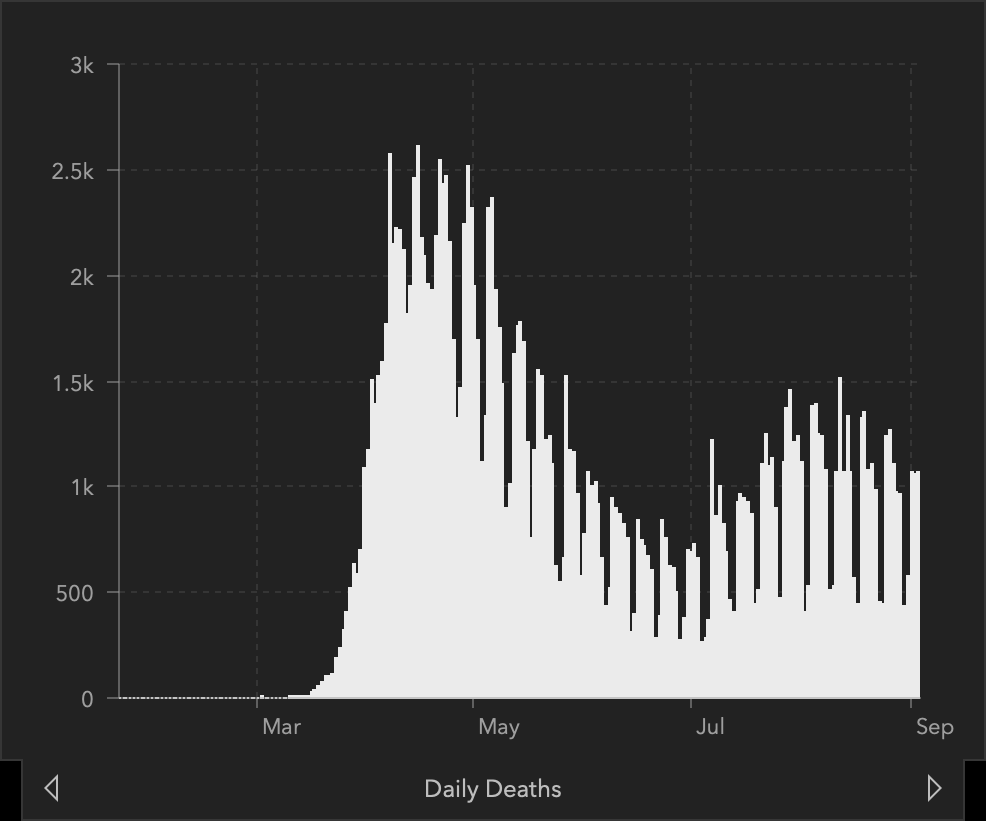
Top left: total confirmed cases in the US. Top right: daily case count. Bottom left: total COVID-19 deaths in the US. Bottom right: daily count of COVID-19 deaths.
Source: Center for Systems Science and Engineering at Johns Hopkins University, September 4, 2020.
For global and regional coronavirus cases in real time check out the Johns Hopkins University Center for Systems Science and Engineering.
For cases by state and county in the U.S. check out https://covid19.topos.com/.
What Is a Coronavirus?
There are hundreds of coronaviruses, most of which circulate among animals including pigs, camels, bats, and cats. Sometimes these viruses jump to humans—a spillover event—and can cause disease, as happened with Severe Acute Respiratory Syndrome (SARS), Middle East Respiratory Syndrome (MERS), and now COVID-19 (NIH, 2020b).
Source: CDC, 2020.
Coronaviruses are named for the crown-like spikes on their surface. There are four main sub-groupings of coronaviruses, known as alpha, beta, gamma, and delta. Only seven of these viruses are known to cause human disease—four of which cause mild to moderate upper-respiratory tract illnesses, like the common cold. However, three times in the twenty-first century, coronavirus outbreaks have emerged from animal reservoirs to cause severe disease and global transmission concerns: SARS, which emerged in late 2002 and disappeared by 2004; MERS, which was first identified in 2012 and consistently jumps from dromedary camels to people; and the 2019 novel coronavirus, that emerged in December 2019 from China (NIH, 2020b).
While most coronaviruses only infect animals, MERS and SARS are notable for their ability to infect a variety of species, including humans. Recent research at the National Institute of Allergy and Infectious Diseases (NIAID) shows how the MERS virus can adapt to infect cells of a new species, which suggests that other coronaviruses might be able to do the same (NIH, 2018). It appears that COVID-19 has done just that. A global effort is under way to contain its spread (NIH, 2018).
How Coronaviruses Adapt to Infect Other Species
To cause infection, a virus must first attach to a receptor molecule on cells of the host species. This interaction is highly dependent on the shape of the receptors, which the host genes control (NIH, 2018b).
To evaluate how MERS evolves to infect host cells, scientists from NIAID tested 16 bat species and found that the virus could not efficiently enter cells with receptors from the common vampire bat, Desmodus rotundus. They then grew virus on cells that had vampire bat receptors and observed the virus evolving to better infect the cells. After a few generations, the virus had completely adapted to the vampire’s receptors (NIH, 2018).
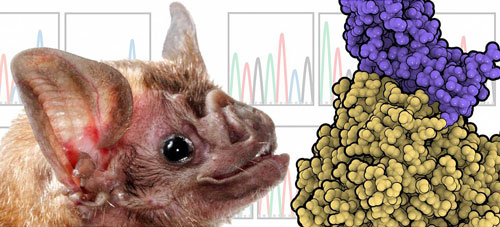
This illustration shows the bat species used in the study, Desmodus rotundus, or vampire bat, and representations of MERS-CoV (purple) interacting with host receptor DPP4 (gold).
Source: NIAID, 2020.
By studying how the shape of the MERS virus changed over time in order to attach to the new host receptor, the scientists found similarities with prior studies of the SARS virus. Thus, while these two viruses are different, they use the same general approach to enter the cells of new species (NIH, 2018).
Human Coronaviruses
The new cluster of viral pneumonia cases originating in Wuhan, China, marks the third time in 20 years that a member of the large family of coronaviruses has jumped from animals to humans and sparked an outbreak.
Anthony S. Fauci, Director
National Institute of Allergy and Infectious Diseases (NIAID)
(NIH, 2020c)
There are seven different coronaviruses that can infect people and cause illness. Common human coronaviruses are:
- 229E (alpha coronavirus)
- NL63 (alpha coronavirus)
- OC43 (beta coronavirus)
- HKU1 (beta coronavirus) (CDC, 2020e)
These viruses have been circulating among humans for many years and usually cause mild to moderate upper-respiratory tract illnesses, like the common cold. Most people become infected with these viruses at some point in their lives and their illnesses are usually of short duration. Symptoms may include
- Runny nose
- Headache
- Cough
- Sore throat
- Fever
- General feeling of being unwell (CDC, 2020e)
These human coronaviruses can also cause lower-respiratory tract illnesses, such as pneumonia or bronchitis; complications more commonly seen in people with cardiopulmonary disease and/or weakened immune systems, infants, and older adults (CDC, 2020e).
Other, newer and more virulent, human coronaviruses are:
- MERS-a beta coronavirus
- SARS-a beta coronavirus
- COVID-19- a beta coronavirus (CDC, 2020e)
Evidence suggests that both SARS and MERS viruses originated in bats before transmitting to civets and camels, respectively.
Source: NIH, 2018.
SARS
Human coronaviruses historically have been regarded as relatively benign causes of the common cold. In 2002, however, a novel, highly pathogenic beta coronavirus emerged in China that caused 8,098 recorded cases of SARS, including 774 deaths, and cost the global economy billions of dollars. Symptoms often included fever, chills, and body aches which usually progressed to pneumonia. Classic public health measures of isolation and containment are likely what brought the outbreak to an end. No human cases of SARS have been reported anywhere in the world since 2004 (NIH, 2020c).
MERS
MERS, another beta coronavirus, jumped from animals to humans in 2012. It causes severe respiratory illness with symptoms of fever, cough, and shortness of breath. About 3 or 4 out of every 10 patients infected with MERS have died. The virus spreads from ill people to others through close contact, such as caring for or living with an infected person. These patients have ranged in age from younger than 1 to 99 years old(NIAID, 2020).
Unlike SARS, which was eliminated within several months of the initial outbreak, MERS continues to smolder due to sporadic transmission from camels—the virus’s intermediate host—to people, and limited chains of person-to-person transmission with a roughly 35 percent fatality rate (NIH, 2020c).
The first known cases of MERS occurred in Jordan in April 2012 and so far all cases of MERS have been linked through travel to, or residence in, countries in and near the Arabian Peninsula. The largest known outbreak of MERS outside the Arabian Peninsula occurred in the Republic of Korea in 2015. That outbreak was associated with a traveler returning from the Arabian Peninsula (CDC, 2019a).
