We in the public health sector must be crystal clear in articulating exactly what we know and what we still need to know about the threat, and in helping people understand how this new risk compares to risks they willingly assume every day. With that perspective, people will be better able to understand what rational steps they can take to protect themselves.
Communicating About COVID-19, Anthony Fauci, March 25, 2020
Contact tracing and follow-up control measures such as quarantine and isolation were crucially important during the SARS outbreak in 2003, the Ebola outbreak in Africa in 2014, as well as in the eradication of smallpox. Until a vaccine is developed, the role of contact tracing and follow-up control measures in the initial stage of this pandemic is especially important. For some novel pathogens, cutting-edge technology may shorten the time needed for vaccine development after initial isolation, bridging the gap between epidemic emergence and vaccine availability (NIH, 2019).
According to the World Health Organization (WHO, 2017), contact tracing consists of three basic steps: identification, listing, and follow-up. All infected people must be identified and isolated. A public health official then calls a confirmed or “clinically compatible case in regions of widespread ongoing transmission” and compiles a list of the patient’s recent contacts including family members, co-workers, healthcare providers or friends.
Regular follow-up must be conducted with all contacts to monitor symptoms of people on the contact list until diagnostic results show that a person is not infected or beyond the incubation period of the virus (WHO, 2017). Contact tracing is a specialized skill. To be done effectively, it requires people with the training, supervision, and access to social and medical support for patients and contacts.
Priority settings include:
- Healthcare facilities including long-term care facilities
- Group home/board
- Homeless shelters
- Federal, state and local correctional facilities
- Crowded, multigenerational housing
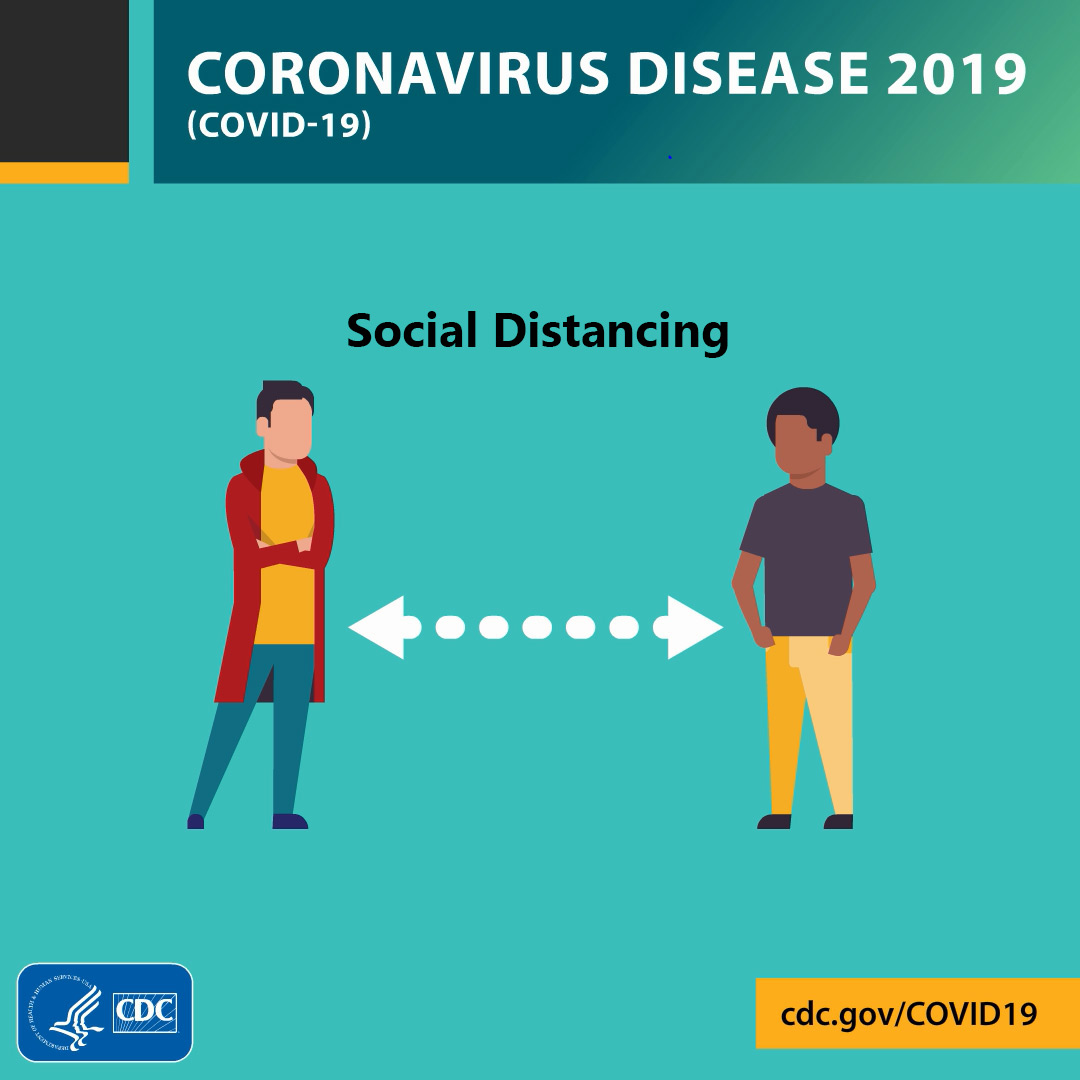
Social distancing is one of the most important mitigation measures recommended by public health experts to slow the spread of COVID-19. Most states have implemented stay-at-home orders, allowing people to go out only for critical needs such as groceries and medicines, or to exercise. Other recommendations include avoiding gatherings, no handshakes, regular handwashing, and, when encountering someone outside of your immediate household, remaining at least 6 feet apart. Masks are required in most states when leaving the home and when in situations in which social distancing is not possible.
What We Learned from SARS
The SARS outbreak was contained in human populations in 2003 largely by aggressive use of traditional public health interventions. The same public health interventions must be used today to stop the spread of COVID-19. The public health measures used during the SARS outbreak were:
- Finding and isolating patients
- Quarantining contacts
- Measures to “increase social distance,” such as canceling mass gatherings and closing schools
- Recommending that the public augment personal hygiene and wear masks
- Limiting the spread of infection by domestic and international travelers, by issuing travel advisories and screening travelers at borders
- Enhanced infection control measures in settings where care was provided to persons with SARS, especially in healthcare facilities and homes (Bell, 2004)
These measures also contained a smaller SARS outbreak in 2004 that originated from a laboratory-acquired infection. Measures to decrease the interval between onset of symptoms and isolation were effective in containing community transmission.
Some measures were implemented because of recommendations by WHO, while others were implemented by governments on their own initiative. A novel technology, infrared scanning, was used extensively in some countries to try to identify persons with fever at international borders and in public places (Bell, 2004).
Identifying and isolating patients, combined with rapid identification and management of contacts, were highly effective in interrupting transmission in several countries. For example, a study in Singapore demonstrated a correlation between rapidly isolating patients after onset of symptoms and a decreased number of secondary cases among their contacts (Bell, 2004).
Contacts in these countries were placed in various forms of quarantine or, less commonly, monitored for symptoms without confinement but isolated if and when symptoms emerged. The location of quarantine was usually at home but was sometimes at a designated residential facility (e.g., for travelers, persons who did not wish to remain at home for fear of exposing their families, homeless persons, and noncompliant persons). In some cases, quarantined persons were allowed to leave the quarantine site with the permission of local health authorities if they wore masks and did not use public transportation or visit crowded public places. In at least one area, these restrictions were applied to essential workers and termed work quarantine (Bell, 2004).
Sixteen Weeks into the COVID-19 Pandemic
On January 23, 2020, when the death count from the novel coronavirus reached 15, a quarantine was declared in Wuhan, China. Air travel was cancelled and trains and buses were stopped. Schools were closed and workers were given additional time off to try to prevent people from congregating and spreading the virus. People were encouraged to stay at home and to use a mask if they had to leave their homes (The Atlantic, 2020).
Travel was banned in the Chinese cities of Huanggang and Ezhou as infections were confirmed there. By January 24, an area with a population of 35 million people was quarantined. In the following days, up to 50 million people in China were quarantined, though that may have been too late to stop the spread of the virus (The Atlantic, 2020).
Wuhan is a city of 11 million people that is a major travel hub. Around 3,500 people daily take direct flights from Wuhan to cities outside of China. The virus began spreading during Lunar New Year celebrations when people travel to be with their families all over China and in other Asian countries. Although the Chinese government shut down travel to and from Wuhan, it is estimated that around 5 million people had already traveled from the city after the outbreak began and before travel restrictions were put into place by the Chinese government (NY Times, 2020b).
On January 30, WHO declared a global health emergency, and January 31 most airlines suspended flights to and from China.
Also, on January 31, the CDC issued mandatory 14-day quarantine orders for 195 U.S. citizens evacuated on a flight from Wuhan, China to a military base in Riverside, California. “CDC, under statutory authority of the HHS secretary, has issued federal quarantine orders for all 195 passengers,” according to CDC’s Messonnier. “While we recognize this is an unprecedented action, we are facing an unprecedented public health threat,” she said (NY Times, 2020c).
The Secretary of Health and Human Services (HHS), Alex M. Azar II, announced that further U.S. citizens returning from Hubei Province would also be quarantined for up to 2 weeks and foreign nationals who had been to China during the last 14 days would not be allowed to enter the United States (NY Times, 2020c).
CDC recommends that you avoid all nonessential international travel because of the COVID-19 pandemic. Some healthcare systems are overwhelmed and there may be limited access to adequate medical care in affected areas. Many countries are implementing travel restrictions and mandatory quarantines, closing borders, and prohibiting non-citizens from entry with little advance notice. Airlines have cancelled many international flights and in-country travel may be unpredictable. If you choose to travel internationally, your travel plans may be disrupted, and you may have to remain outside the United States for an indefinite length of time. CDC also recommends all travelers defer all cruise ship travel worldwide (CDC, May 28, 2020).
Traveler’s Card in English from Earlier in 2020

Source: CDC, 2020.
Testing for COVID-19
CDC Test Kit for COVID-19

Source: CDC, 2020.
At the start of the COVID-19 outbreak in the United States, CDC’s policy was to test only people with a history of exposure who were showing symptoms. Testing people too early, they said, could potentially miss infections because the virus had not established itself sufficiently in the system to be detected, the test may give a false negative result, and people may later become sick (CDC, 2020c).
According to a CDC press briefing on February 14, 2020:
CDC tested all of the initial 195 people who returned from Wuhan on January 29. But since that time we have learned more about how the virus behaves in people and when is the optimal time to test them [so as] to best inform our public health response. CDC may do testing of all people again if the risk warrants it, but right now, CDC staff (at each base where people are quarantined) are checking temperatures twice daily and monitoring people for any new symptoms. If someone has symptoms compatible with this new virus they’re medically evaluated and they’re tested (CDC, 2020c).
CDC later expanded its testing policy for COVID-19 because of a new case in Solano County, California. A woman who was transferred from a local hospital to UC Davis Medical Center in Sacramento was believed to be the first case of community spread of the disease in the United States. Even though the patient was showing symptoms of COVID-19, she did not meet the criteria of recent travel to China or contact with an infected person and therefore was not tested for several days.
“As soon as that case was recognized, we . . . revised our definition,” said CDC director Robert Redfield on February 27 at a congressional hearing. “If a public official suspects coronavirus, then we should get a test for coronavirus. That updated guidance went out today.”
Even though the United States revised the criteria for testing, there were still not enough kits available for those who needed them. By the end of March, 2020, the U.S. still did not have enough tests to determine the extent of infections in the country. “The government’s incapacity to conduct widespread testing slowed diagnoses, creating chains of infection. It also deprived epidemiologists of a map that could have told them how far and how fast the virus was traveling and where they should concentrate efforts to slow it down” (Politico, (2020).
The genome for the novel coronavirus was shared with the world by Chinese scientists on January 11, 2020 and “within a week virologists in Berlin had produced the first diagnostic test for the disease.” Soon, other countries had developed their own tests and by the end of February, WHO shipped tests to almost 60 countries, but not to the United States. It is not known why the United States did not receive the tests or why it has taken so long to develop our own (Politico, (2020). See Politico's How testing failures allowed coronavirus to sweep the U.S. (Retrieved March 30, 2020).
The CDC clinical criteria for considering testing for COVID-19 have been developed based on what is known about COVID-19 and are subject to change as additional information becomes available. Two kinds of tests are available for COVID-19: viral tests and antibody tests. A viral test tells you if you have a current infection. An antibody test tells you if you had a previous infection (CDC, 2020).
Viral tests check samples from your respiratory system (such as swabs of the inside of the nose) to tell you if you currently have an infection with SARS-CoV-2, the virus that causes COVID-19. Some tests are point-of-care tests, meaning results may be available at the testing site in less than an hour. Other tests must be sent to a laboratory to analyze, a process that takes 1-2 days once received by the lab (CDC, 2020).

Source: CDC, 2020.
Real time reverse transcription polymerase chain reaction (rRT-PCR) is an example of a viral test used to detect the coronavirus. The test uses respiratory samples from a nasopharyngeal swab or sputum sample. Results can be available within a few hours to 2 days (CDC, 2020).
Antibody tests, a type of serological test, detect antibodies present in the blood when the body is responding to or has responded to a specific infection, such as COVID-19. Antibody tests detect the body’s immune response to the infection caused by the virus rather than detecting the virus itself. This is why they should not be used to diagnose current SARS-CoV-2 infection (FDA, May 4, 2020).
Antibody tests can be used to determine if individual patients may have been exposed to and infected with a virus, and also can be used to understand to understand how many people in a population have antibodies (known as “surveillance tests,” or sero-surveys) (FDA, May 4, 2020).
Source: NIH Director's Blog, 2020
In general, a positive antibody test is presumed to mean a person has been infected with SARS-CoV-2, the virus that causes COVID-19, at some point in the past. It does not mean they are currently infected. Antibodies start developing within 1 to 3 weeks after infection. We currently don’t have enough information yet to say whether someone will definitely be immune and protected from reinfection if they have antibodies to the virus (CDC, 2020).
Public Health Measures Recommended by CDC
Public health measures are used to slow down the spread and limit the size of an epidemic. These measures save lives and also buy time for treatments and vaccines to be developed.
CDC has established the following exposure risk categories to help guide optimal public health management of people following potential COVID-19 exposure (CDC, 2020i).
Risk Categories for Exposures Associated with International Travel or Identified during Contact Investigations of Laboratory-confirmed Cases | ||
|---|---|---|
Risk Level | Geographic (Travel-associated) Exposures* | Exposures Identified through Contact Investigation |
High | Travel from Hubei Province, China | Living in the same household as, being an intimate partner of, or providing care in a nonhealthcare setting (such as a home) for a person with symptomatic laboratory-confirmed COVID-19 infection without using recommended precautions for home care and home isolation |
Medium (assumes no exposures in the high-risk category) |
|
|
Low (assumes no exposures in the high-risk category) | Travel from any other country | Being in the same indoor environment (e.g., a classroom, a hospital waiting room) as a person with symptomatic laboratory-confirmed COVID-19 for a prolonged period of time but not meeting the definition of close contact |
No identifiable risk | Not applicable | Interactions with a person with symptomatic laboratory-confirmed COVID-19 infection that do not meet any of the high-, medium- or low-risk conditions above, such as walking by the person or being briefly in the same room. |
* * *
CDC recommends the following guidelines after determining risk categories for people exposed to the coronavirus (CDC, 2020h).
The public health actions recommended in the table below apply to people who have been determined to have at least some risk for COVID-19. People who are being managed as asymptomatic in a particular risk level who develop signs or symptoms compatible with COVID-19 should be moved immediately into the symptomatic category in the same risk level and be managed accordingly. The risk level does not change if symptoms develop.
Summary of CDC Recommendations for Management of Exposed Persons with by Risk Level and Presence of Symptoms | ||
|---|---|---|
Risk Level | Management if Asymptomatic | Management if Symptomatic1 |
High Risk |
|
|
Medium Risk | Close contacts in this category:
|
|
Travelers from mainland China (outside Hubei Province) or Iran
| ||
Travelers from other country with widespread transmission
| ||
Travelers from other country with sustained community transmission
| ||
Low Risk |
|
|
No Identifiable Risk | None |
|
Note: The public health management recommendations made above are primarily intended for jurisdictions not experiencing sustained community transmission. In jurisdictions not experiencing sustained community transmission, CDC recommends that post-exposure public health management for asymptomatic exposed individuals continue until 14 days after the last potential exposure; however, these decisions should be made based on the local situation, available resources, and competing priorities. These factors should also guide decisions about managing symptomatic exposed individuals.
International travelers and other potentially exposed individuals in jurisdictions experiencing sustained community transmission should follow local guidance.
Prevention
There is currently no vaccine to prevent a COVID-19 infection. The best way to prevent infection is to avoid being exposed to the virus. Everyday actions to help prevent the spread of respiratory viruses include (CDC, 2020i):
- Wash your hands often with soap and water for at least 20 seconds, especially after going to the bathroom; before eating; and after blowing your nose, coughing, or sneezing.
- If soap and water are not readily available, use an alcohol-based hand sanitizer with at least 60% alcohol. Always wash hands with soap and water if hands are visibly dirty.
- Avoid touching your eyes, nose, and mouth with unwashed hands.
- Avoid close contact with people who are sick.
- Stay home when you are sick.
- Cover your cough or sneeze with a tissue, then throw the tissue in the trash.
- Clean and disinfect frequently touched objects and surfaces using a regular household cleaning spray or wipe. (CDC, 2020j)
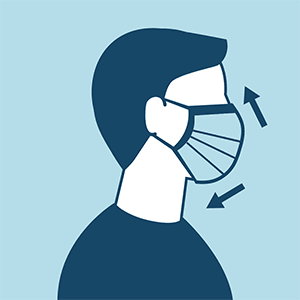
CDC on Homemade Cloth Face Coverings
CDC recommends wearing cloth face coverings in public settings where other social distancing measures are difficult to maintain (e.g., grocery stores and pharmacies), especially in areas of significant community-based transmission.
CDC also advises the use of simple cloth face coverings to slow the spread of the virus and help people who may have the virus and do not know it from transmitting it to others. Cloth face coverings fashioned from household items or made at home from common materials at low cost can be used as an additional, voluntary public health measure.
Cloth face coverings should not be placed on young children under age 2, anyone who has trouble breathing, or is unconscious, incapacitated or otherwise unable to remove the mask without assistance.
The cloth face coverings recommended are not surgical masks or N-95 respirators. Those are critical supplies that must continue to be reserved for healthcare workers and other medical first responders, as recommended by current CDC guidance.
How to Wear Face Covering
Face coverings should:
- Fit snugly but comfortably against the side of the face
- Be secured with ties or ear loops
- Include multiple layers of fabric
- Allow for breathing without restriction
- Be able to be laundered and machine dried without damage or change to shape