Mental health has traditionally been the purview of psychiatrists and mental health practitioners. Over the last two to three decades however, family practice physicians, nurse practitioners, allied health professionals, social workers, and other healthcare providers are increasingly responsible for screening, assessing, and managing chronic mental health problems. Because of this, all healthcare providers must be knowledgeable about suicide risk factors and warning signs; understand suicide assessment and screening tools; and know when, where, and how to treat or refer a client who is at risk for self-harm.
Defining Terms
- Suicide is defined as death caused by self-directed injurious behavior with intent to die as a result of the behavior.
- A suicide attempt is a non-fatal, self-directed, potentially injurious behavior with intent to die as a result of the behavior. A suicide attempt might not result in injury.
- Suicidal ideation refers to thinking about, considering, or planning suicide.
Source: NIMH, 2019.
Throughout the world, suicide is an increasingly serious public health concern. Every year over 800,000 people die by suicide, and between 10 and 20 million attempt suicide. Often suicidal thoughts precede a suicide attempt or completed suicide. Among those thinking about suicide, about one-third attempt suicide, and more than half of these attempts occur within the first year after the onset of suicidal thoughts (Brüdern et al., 2018).
U.S. Suicide Rates, 1999–2016
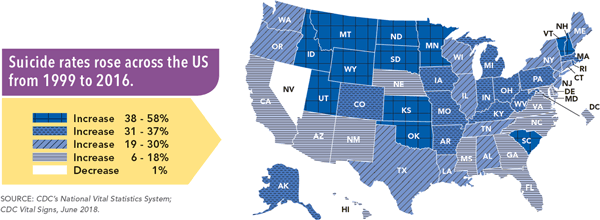
Suicide rates vary from state to state. Source: CDC, 2018a.
In the United States, approximately 47,000 people die from suicide each year, making it the country’s tenth leading cause of death (NIMH, 2019). Suicide is not limited to any one age, socioeconomic or ethnic group, or gender. Remarkably, in 2017 there were more than twice as many suicides in the United States as homicides (NIMH, 2019).
For youth and young adults (ages 10–24) suicide is the second leading cause of death (19.2% of deaths). It is also the second leading cause of death for adults aged 25 to 44 (10.9%). For middle-aged adults (age 45–64) suicide rates subside somewhat but still represent the eighth leading cause of death (3.1% of deaths). For the populations aged 65 and over, suicide is not among the 10 leading causes of death (Heron, 2019).
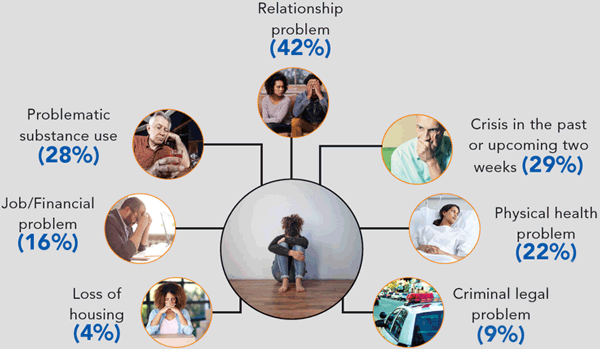
Many factors contribute to suicide among those with and without known mental health conditions.
Source: CDC’s National Violent Death Reporting System, data from 27 states participating in 2015.
Key Points About Suicide
- Suicide is not a personal weakness or family failure.
- Suicide prevention is everyone’s responsibility.
- Silence and stigma harm individuals, families, and communities.
- Suicide does not affect all communities equally or in the same way.
- People experiencing suicidal thoughts retain the right to make decisions about their care.
Biological, psychological, social, environmental, and situational factors influence suicidal behaviors. Childhood trauma, substance abuse, poverty, untreated mental health problems, loss of housing, financial difficulties, health problems, legal issues, and relationship problems are some of the factors that may contribute to suicidal ideation and behaviors. Unfortunately, many people do not or cannot get the help they need because of provider shortages, stigma, and the cost of care.
