Lethal means are items or actions that might be used in a suicide attempt that are likely to result in death. Lethal means can be divided into two main categories: violent and nonviolent methods. Violent methods can include firearms, cutting or piercing with a sharp object, hanging, jumping from high places, or stepping in front of a train or other vehicle. Nonviolent methods include ingestion of pesticides, poison by gases, suffocation, and overdose. Access, availability, and social acceptability of certain suicide methods and some location-specific factors such as access to firearms or tall buildings can factor into the choice of a lethal means (Sun & Jia, 2014).
Objects Used in Suicide Attempts
Household gun ownership rates are a significant positive predictor of both homicide and suicide. A substantial proportion of Americans—over 50% in some states—live in households with guns and may not need to purchase a new firearm to carry out a violent act (Swanson et al., 2015). More than half of male suicides are firearm-related (NCHS, 2016).
Although individuals who own firearms are not more likely than others to have a mental disorder or to have attempted suicide, the risk of a death is higher among this population because individuals who attempt suicide using a firearm are more likely to die in their attempts than those who use less lethal methods.
The use of firearms is particularly prevalent among veterans, with approximately 41% of female and 68% of male suicide deaths resulting from a firearm. Poison is the second-most common means of suicide among female veterans while suffocation is the second-most common cause of death among male veterans (USDVA, 2016a).
Substances Used in Suicide Attempts
Among middle-aged adults (aged 35 to 64) poisoning (predominantly drug overdose) is the leading cause of suicide death among females and the third leading cause for males. Suicide attempts (and suicide deaths) among middle-aged adults have increased in recent years, which underscores the importance of understanding risk factors for suicide in this age group (Tesfazion, 2014).
Nearly all drug-related emergency department visits involving suicide attempts among middle-aged adults involve prescription drugs and over-the-counter medications. About half of visits involve anti-anxiety and insomnia medications, a third involve pain relievers, and 22% involve antidepressants. Among middle-aged adults, more than a third of all drug-related ED visits involving a suicide attempt also involved alcohol, and 11% involved illicit drugs (Tesfazion, 2014).
Inert gas asphyxiations using helium have been on the increase in the United States. The increasing familiarity with this gas is partly the reason for the rise in suicide by helium. Helium suicides have also been publicized on internet websites as simple and painless. More formal recommendations regarding suicides with inert gas asphyxiations need to be developed as well as restricting access to helium (Hassamal et al., 2015).
The most frequent “other” suicide methods for females are falls and drowning. For males, the most frequent “other” methods are falls and cutting or piercing (NCHS, 2016). Although falling from buildings or bridges is a relatively small percentage of suicide attempts, it is very often lethal (Hemmer et al., 2017)
For both females and males, about a quarter of suicides in 2014 were attributable to suffocation (includes hanging, strangulation, and suffocation), an increase over previous years (NCHS, 2016). The high prevalence of asphyxiations can be attributed to the widespread availability of means for hanging. Currently, there are no formal proposals on how to reduce asphyxiation suicides. Research indicates that those who attempted suicide by hanging viewed it as a quick, simple, and painless death. One way to reduce hanging suicides would be to challenge perceptions of hanging as a quick, simple, and painless suicide method (Hassamal et al., 2015).
Suicide Deaths, by Method and Sex: United States, 1999 and 2014
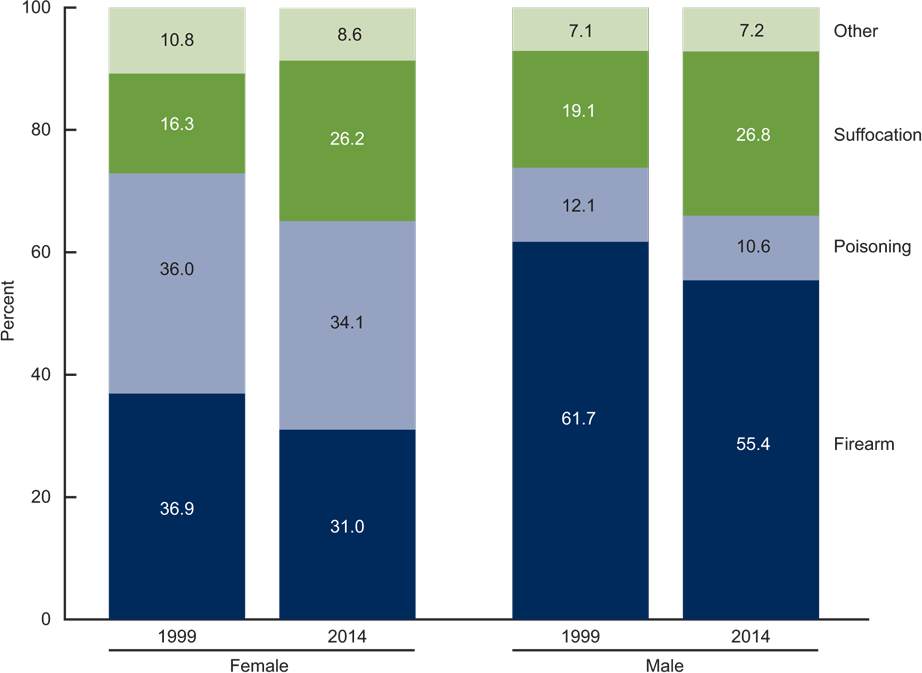
Source: NCHS, National Vital Statistics System, Mortality.
Talking About Lethal Means
Individuals experiencing significant distress or who have a recent history of suicidal behavior should not have easy access to means that may be used in a suicide attempt. This includes access to firearms, weapons, medications, illicit drugs, chemicals used in the household, other poisons, or materials used for hanging or suffocation.
Healthcare providers are in a unique position to ask about lethal means. Providers have the opportunity to educate patients and families about safe firearm storage and access, as well as the appropriate storage of alcoholic beverages, prescription drugs, over-the-counter medications, and poisons. Many healthcare providers avoid these discussions or ask about lethal means only when a patient is identified as being at a very high risk for suicide.
About Lethal Means—A Nurse Practitioner’s Guidance
Once you have identified that your patient is at risk for self-harm, try to identify any lethal means that your patient might be able to access once he or she leaves your office. Ask direct questions: “While you’re in this dangerous period, may I call your partner or family member and ask them to remove the guns or poisons from the house?”
Ask permission and show concern in a non-judgmental manner—this is more likely to elicit information from your patient. You can continue by saying “I want to let you know that I appreciate and am honored that you’ve shared your thoughts with me. I’m just concerned that you may go again to a place of despair when you leave and I’m thinking of your safety.”
Try to establish and maintain trust with your patient—if you think the person is at risk, there is no reason to cover your concern or to lie.
Restricting Access to Lethal Means
Means restriction involves techniques, policies, and procedures designed to reduce access or availability to means and methods of deliberate self-harm. Among suicide prevention interventions, reducing access to highly lethal means of suicide has a strong evidence base and is now considered a key strategy to reduce suicide death rates (Betz et al., 2016).
Lethal means restriction can include:
- Complete removal of a lethal method
- Reducing the toxicity of a lethal method, for example, reducing carbon monoxide content emissions from vehicles
- Interfering with physical access, for example, using gun locks or placing barriers on bridges
- Enhancing safety, for example, encouraging at-risk families to remove lethal suicide means from the home
- Reducing the appeal of a more lethal method, for example, changing the perception of hanging as a quick and painless death.(Hassamal et al., 2015)
The majority of suicide attempts are transient and the time between contemplating suicide and the attempt is less than 5 minutes for many attempters. Success or failure depends on what method is readily available (Hassamal et al., 2015).
Restricting access to firearms is of particular importance because a suicide attempt using a firearm is fatal about 90% of the time. Patients with access to firearms at home might be considered at particularly high risk for discharge to home, given that firearm access is a risk factor for suicide (Betz et al., 2016).
While access to firearms and other lethal means does not mandate psychiatric admission, restricting access to firearms is a key component of home safety planning that should be addressed with all patients being discharged. Safe storage of firearms and other lethal means has been associated with less risk for suicide among adults and youth, and lethal means counseling in EDs might affect storage behavior (Betz et al., 2016).
Reducing access to potentially toxic medications is also important but can be a challenge, given that many of the medications used to treat mental illness can be toxic in an overdose. In one sample, 60% of patients reported currently taking at least one medication for an emotional or psychological problem, and medication overdose was the suicide method most commonly reported as having been considered (Betz et al., 2016).
Access to other lethal means of suicide—such as sharp objects or supplies for hanging—is also difficult to control given their widespread availability for other purposes. Installing bridge barriers or otherwise restricting access to popular jump sites may prevent deaths, depending on specific local conditions.
In times of crisis or during stressful transitions, research indicates that:
- The interval between deciding to act and attempting suicide can be as short as 5 or 10 minutes.
- People tend not to substitute a different method when a highly lethal method is unavailable or difficult to access.
- Increasing the time interval between deciding to act and the suicide attempt by making it more difficult to access lethal means, can be lifesaving. (Stone et al., 2017)
If a lethal method is not immediately available, the crisis will often pass, and the person may never attempt suicide. It is important to understand that most people who attempt suicide once and survive, never attempt again. Putting time, distance, and other barriers between a person at risk and the most lethal means can make the difference between life and death (WSDOH, 2016).
For patients at highest risk, make sure firearms are inaccessible. For patients at intermediate to high acute risk, discuss the possibility of safe storage of firearms with the patient and family. When possible, limit access to medications that carry risk for suicide, at least during the periods when patient is at acute risk. This may include prescribing limited quantities, supplying the medication in blister packaging, providing printed warnings about the dangers of overdose, or ensuring that currently prescribed medications are controlled by a responsible party. Also provide information on how to secure chemical poisons, especially agricultural and household chemicals, to prevent accidental or intentional ingestions. Many of these chemicals are highly toxic.
Restricting Access to Suicide Hotspots
Suicide hotspots, or places where suicides may take place relatively easily, include tall structures such as bridges, cliffs, balconies, and rooftops; railway tracks; and isolated locations such as parks. Efforts to prevent suicide at these locations include erecting barriers or limiting access to prevent jumping, and installing signs and telephones to encourage individuals who are considering suicide to seek help (Stone et al., 2017).
A meta-analysis examining the impact of suicide hotspot interventions implemented in combination or in isolation, both in the United States and abroad, found reduced rates of suicide. For example, after erecting a barrier on the Jacques-Cartier Bridge in Canada, the suicide rate for jumping from the bridge decreased from about 10 suicide deaths per year to about 3 deaths per year. Moreover, the reduction in suicides by jumping was sustained even when all bridges and nearby jumping sites were considered, suggesting little to no displacement of suicides to other jumping sites. Further evidence for the effectiveness of bridge barriers was demonstrated by a study examining the impact of the removal of safety barriers from the Grafton Bridge in Auckland, New Zealand (see box) (Stone et al., 2017).
Unintended Consequences—The Grafton Bridge
In 1996, after having been in place for 60 years, safety barriers to prevent suicide by jumping were removed from Grafton Bridge in Auckland, New Zealand. The barriers were reinstalled in 2003.
Removal of barriers was followed by a fivefold increase in the number and rate of suicides from the bridge. Since the reinstallation of barriers, there have been no suicides from the bridge. This natural experiment shows that safety barriers are effective in preventing suicide: their removal increases suicides; their reinstatement prevents suicides.
Source: Harvard School of Public Health, 2017.
Public jump sites are well-suited for suicide prevention, given that a great number of suicides are often limited to a few structures. At these hotspots, substantial suicide preventive effects can be achieved by a few prevention efforts. Most interventions for suicide prevention on bridges are of a structural nature (Hemmer et al., 2017).
Did You Know. . .
The Aurora Bridge in Seattle had the second highest suicide death toll in the United States (behind the Golden Gate Bridge). In 2006 emergency call boxes and signs with a suicide hotline number were installed on the bridge. Suicides continued to occur at an average of about five per year until a fence was installed in 2011. In the 18 months afterward, only one suicide occurred (Draper, 2017).
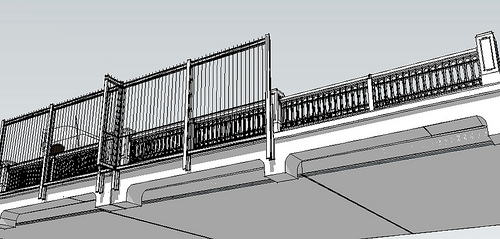
Designer view of the Aurora Bridge Fence suicide barrier in Seattle prior to its construction in 2010. Source: Washington State Department of Transportation.
Some interventions to prevent jumps from hotspots or other methods of suicide are not feasible for bridges. Although blocking access roads to hotspots have been shown to deter suicide jumps, this is not a viable measure for most bridges. There is evidence that the number of suicides by carbon monoxide poisoning in public parking lots has been reduced by installing aid signs. However, no studies exist that evaluate the effectiveness of aid signs as the sole intervention when used on bridges or other jumping sites, although they are widely installed (Hemmer et al., 2017).
Some research has shown that, if in addition to aid signs, emergency helpline phones are directly available on bridges, the phones are used on a regular basis. Another research project found that, in combination with increased police presence, emergency helplines led to a decrease in the number of suicides at the Sunshine Skyway Bridge in Florida (Hemmer et al., 2017).
Safe Storage Practices
Safe storage of medications, firearms, and other household products can reduce the risk for suicide by separating vulnerable individuals from easy access to lethal means. Such practices may include education and counseling around storing firearms locked in a secure place, unloaded and separate from the ammunition; and keeping medicines in a locked cabinet or other secure location away from people who may be at risk or who have made prior attempts (Stone et al., 2017).
In a case-control study of firearm-related events identified from 37 counties in Washington, Oregon, and Missouri, and from five trauma centers, researchers found that storing firearms unloaded, separate from ammunition, in a locked place or secured with a safety device was protective of suicide attempts among adolescents. Further, a systematic review of clinic and community-based education and counseling interventions suggested that the provision of safety devices significantly increased safe firearm storage practices compared to counseling alone or compared to the provision of economic incentives to acquire safety devices on one’s own (Stone et al., 2017).
Pharmacists and community healthcare and mental health providers play a critical role in encouraging safe storage of potentially lethal products. For pharmacists and mental health providers, medications are of particular concern because of the potential for abuse, accidental poisonings, and use in suicide attempts. Safer Homes Suicide Aware recommends:
- Lock up prescription medications.
- Limit the supply of in-home, over-the-counter medications.
- Return unused medications.
- Dispose of medications in cat litter or coffee grounds and place in the trash. (Safer Homes Suicide Aware, n.d.)
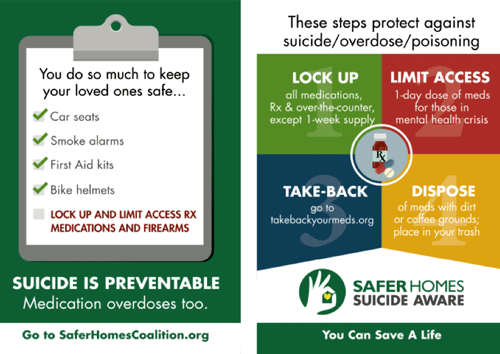
Source: Safer Homes Suicide Aware Training Materials. Used with permission.
ED CALM
The Emergency Department Counseling on Access to Lethal Means (ED CALM) trained psychiatric emergency clinicians in a large children’s hospital to provide lethal means counseling and safe storage boxes to parents of patients under age 18 receiving care for suicidal behavior. In a pre-post quality improvement project, researchers found that at post-test 76% reported that all medications in the home were locked up as compared to fewer than 10% at the time of the initial emergency department visit. Among parents who indicated the presence of guns in the home at pre-test (67%), all (100%) reported guns were currently locked up at post-test.
Source: Stone et al., 2017.
Francoise Gets Help from Her Pharmacist
Francoise is a 45-year-old woman who was previously stable on medications (lithium) for bipolar disorder. She stopped filling her prescription for lithium about 3 months ago.
On the day the pharmacist is conducting screening, Francoise arrives at the Rite Aid Pharmacy with prescriptions for opioids and benzodiazepines from a different provider in a nearby town. She appears nervous and agitated with evidence of thought disorder. She also smells of alcohol, which the pharmacist knows further increases risk of death—intended or unintended—from the combination of disturbed thought process along with certain medications and alcohol.
Screening
The Rite Aid Pharmacy uses the Patient Health Questionnaire 2 to screen clients for suicidal ideation and behavior. The screening is activated when a client has a sudden change in medications, has a prescription from another pharmacy, is filling a prescription for high-risk medications, or when a client’s behavior causes staff concern. The pharmacist asks Francoise, “Over the last 2 weeks, how often have you been bothered by either of the following problems?
- Little interest or pleasure in doing things?
- Feeling down, depressed, or hopeless?
Although appearing quite nervous and agitated, Francoise answers in the negative to each question.
What Should You Do?
The pharmacist is concerned that Francoise is denying or minimizing her feelings. Because of the combination of medications and behaviors, she is worried that Francoise is in acute danger. She decides to ask some more direct followup questions. She uses another screening tool, the Emergency Medicine Network’s EDSAFE Patient Safety Screener that she’s familiar with from working in a hospital-based pharmacy. She asks Francoise:
- Over the last 2 weeks, have you had thoughts of killing yourself?
- In your lifetime, have you ever attempted to kill yourself? If so, when?
Francoise says she feels fine and hasn’t had any thoughts of harming herself. She says she did try to commit suicide in the past but refused to say when or how. She asks when she can get her prescriptions.
The pharmacist asks Francoise if she can contact a family member for additional information. She agrees. If Francoise had declined consent, HIPAA permits a clinician to make these contacts without the patient’s permission when the clinician believes the patient may be a danger to self or others.
Because the pharmacist has a “duty to protect” her client, she asks Francoise to wait with her in a private room and directs a cashier to call her family. Francoise’s husband arrives quickly and agrees to take his wife to the ED. The pharmacist follows up with local emergency and learns that Francoise has arrived at the hospital and is being evaluated.
Discussion
Relapsing bipolar disorder places a person at increased risk for suicide. Because Francoise stopped taking lithium and succeeded in getting prescriptions for a supply of medications from a different pharmacy, she now had the means (and perhaps the motive) to self-harm. The pharmacist and her staff were able to help Francoise through a combination of engagement, screening, concern, and a nonjudgmental attitude. They kept Francois in a safe environment under one-to-one observation until someone arrived to take her to the hospital. The system set up by the pharmacy to flag high-risk mediations along with a screening protocol provided help to a person in acute crisis.Policy-Based Strategies
Policy-based strategies that restrict access to lethal means have led to positive results. For example, limiting access to suicide methods such as carbon monoxide has resulted in decreases in suicide by carbon monoxide. Restriction of other suicide methods has also shown positive results. The implementation of enhanced restrictions to purchase firearms in the District of Columbia led to reductions in firearm-related suicides (Hassamal et al., 2015).
Although this goal focuses on reducing access to lethal means among individuals at risk, evidence for means restriction has come from situations in which a universal approach was applied to the entire population. For example, the detoxification of household gas in the United Kingdom and discontinuation of highly toxic pesticides in Sri Lanka were universal measures associated with 30% and 50% reductions in suicide, respectively.
