I attempted to take my life because of a breakup when I was 16. I woke up and I was fine, but I was really mad. I just didn’t want to live! I’d been trying to get a gun, and word got around. The school called my mom and a social worker came to talk to me. But what really changed my mind was my dad. I could feel his love, and it felt like he would lay down his life for me. Thinking about that would snap me out of it—suicide would hurt my family more than I’m hurting now.
In my worst moments the thought lingers, but now I know I could never go through with suicide. My faith gets me through those times—knowing that something bigger is out there and I shouldn’t rob myself of what is yet to come. My kids give me a sense of purpose. I’m able to say to myself, “No, that’s not an option, you can’t do that.” And I was really lucky to have that connection with my dad.
Annie Ost, Spokane
Source: WSDOH, 2016
A person’s support network can be a source of strength in times of crisis as well as during recovery. Strong social and familial ties decrease stress and increase a person’s ability to cope with a traumatic events or situations. Social support is a strong protective factor, which can diminish the risk of suicide:
- General support—such as positive contact, transportation and childcare, and messages of love and concern—is an important part of any social network.
- Crisis support—such as transport to a hospital or crisis center and assistance with children or pets—provides critical support during a new crisis.
Peer Support Programs
Peer norm programs seek to normalize protective factors for suicide by encouraging help-seeking, talking to trusted adults, and promoting peer connectedness. By leveraging the leadership qualities and social influence of peers, these approaches can be used to shift group-level beliefs and promote positive social and behavioral change. Peer norm programs typically target youth and are delivered in school settings but can also be implemented in community settings (Stone et al., 2017).
Programs such as Sources of Strength can improve school norms and beliefs about suicide that are created and disseminated by student peers. In a trial of Sources of Strength involving 18 high schools, researchers found that the program improved adaptive norms regarding suicide, connectedness to adults, and school engagement. Peer leaders were also more likely than controls to refer a suicidal friend to an adult. For students, the program resulted in increased perceptions of adult support for suicidal youths, particularly among those with a history of suicidal ideation, and the acceptability of help-seeking behaviors. Trained peer leaders also reported a greater decrease in maladaptive coping attitudes compared with untrained leaders (Stone et al., 2017).
Video: What Is Sources of Strength? [3:10]
https://www.youtube.com/watch?v=Rgi9GjhW3Ss
Gatekeeper Training
Gatekeeper suicide intervention training, which dates back to the late 1960s, teaches people to identify others at high risk for suicide and refer them to treatment. In essence, gatekeepers “open the gate” to get help for people at risk of suicide (Nasir et al., 2016).
Gatekeeper training (also referred to as “recognition and referral training”) teaches people with no formal psychosocial training to identify people who may be at risk of suicide. It provides information on how to respond, including encouraging the at-risk person to seek treatment and support services. Research shows that many at-risk people show warning signs that family, friends, or other gatekeepers may first notice.
Gatekeepers can be divided into two groups. Designated gatekeepers are professionals in healthcare, social work, nursing, and psychology. Emergent gatekeepers are community members who may not have been formally trained in suicide prevention, but who may have contact with people who have suicidal intent. Family, friends, and peer-helpers may be appropriate gatekeepers because of their close relationships with those at risk for suicide (Nasir et al., 2016).
One closely studied gatekeeper program, Applied Suicide Intervention Skills Training (ASIST), helps hotline counselors, emergency workers, and other gatekeepers identify and connect with suicidal individuals and direct them to available resources. Research has shown that callers who spoke with ASIST-trained counselors feel less depressed, less suicidal, less overwhelmed, and more hopeful by the end of their call, compared to callers who spoke to non-ASIST trained counselors. Counselors trained in ASIST were also more skilled at keeping callers on the phone longer and establishing a connection with them (Stone et al., 2017).
Gatekeeper training is a primary component of the Garret Lee Smith (GLS) Suicide Prevention Program, which has been implemented in 50 states and 50 tribes. A study assessing the impact of this training on suicide attempts and deaths compared the change in suicide rates and nonfatal suicidal behavior among young people (aged 10–24) in counties implementing GLS trainings, compared to similar counties that did not implement these trainings. Counties that implemented GLS trainings had significantly lower youth suicide rates one year following the training implementation. This equates to a decrease of 1 suicide death per 100,000 youth ages 10 to 24, or the prevention of approximately 237 deaths in the age group, between 2007 and 2010 (Stone et al., 2017).
Counties implementing GLS program activities also had significantly lower suicide attempt rates among youth (aged 16 to 23) in the year following implementation of the GLS program than did similar counties that did not implement GLS activities. More than 79,000 suicide attempts may have been prevented during the period examined (Stone et al., 2017).
Crisis Lines
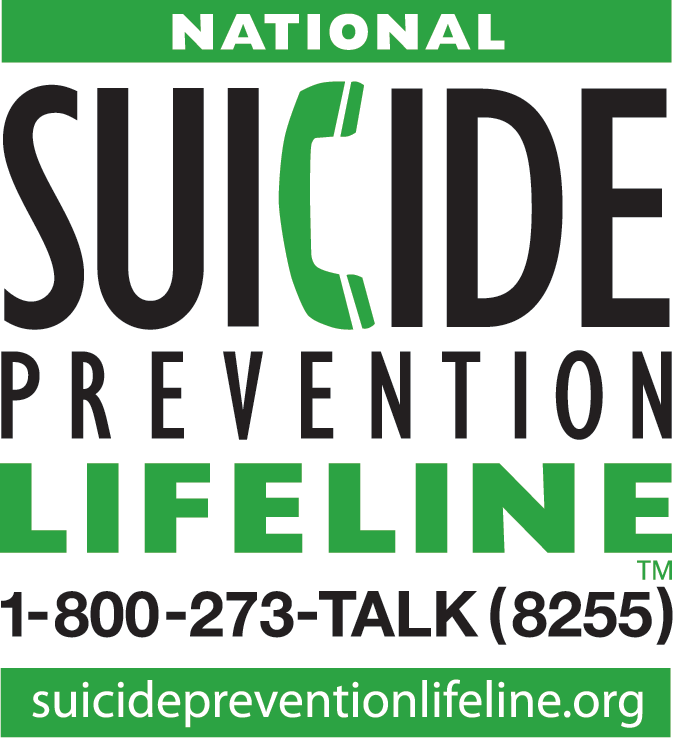
National Suicide Prevention Lifeline. Source: CDC.
Crisis intervention programs provide support and referral services, typically by directing a person in crisis (or a friend or family member of someone at risk) to trained volunteers or professional staff via telephone hotline, online chat, text messaging, or in person. Crisis interventions can put space or time between an individual who may be considering suicide and harmful behavior (Stone et al., 2017).
Crisis lines provide immediate access, often 24 hours a day. They are an access point for emergency care, clinical assessment, referral, and treatment. When other providers are closed and personal support networks are unavailable, crisis lines can be a lifeline for people at risk of suicide.
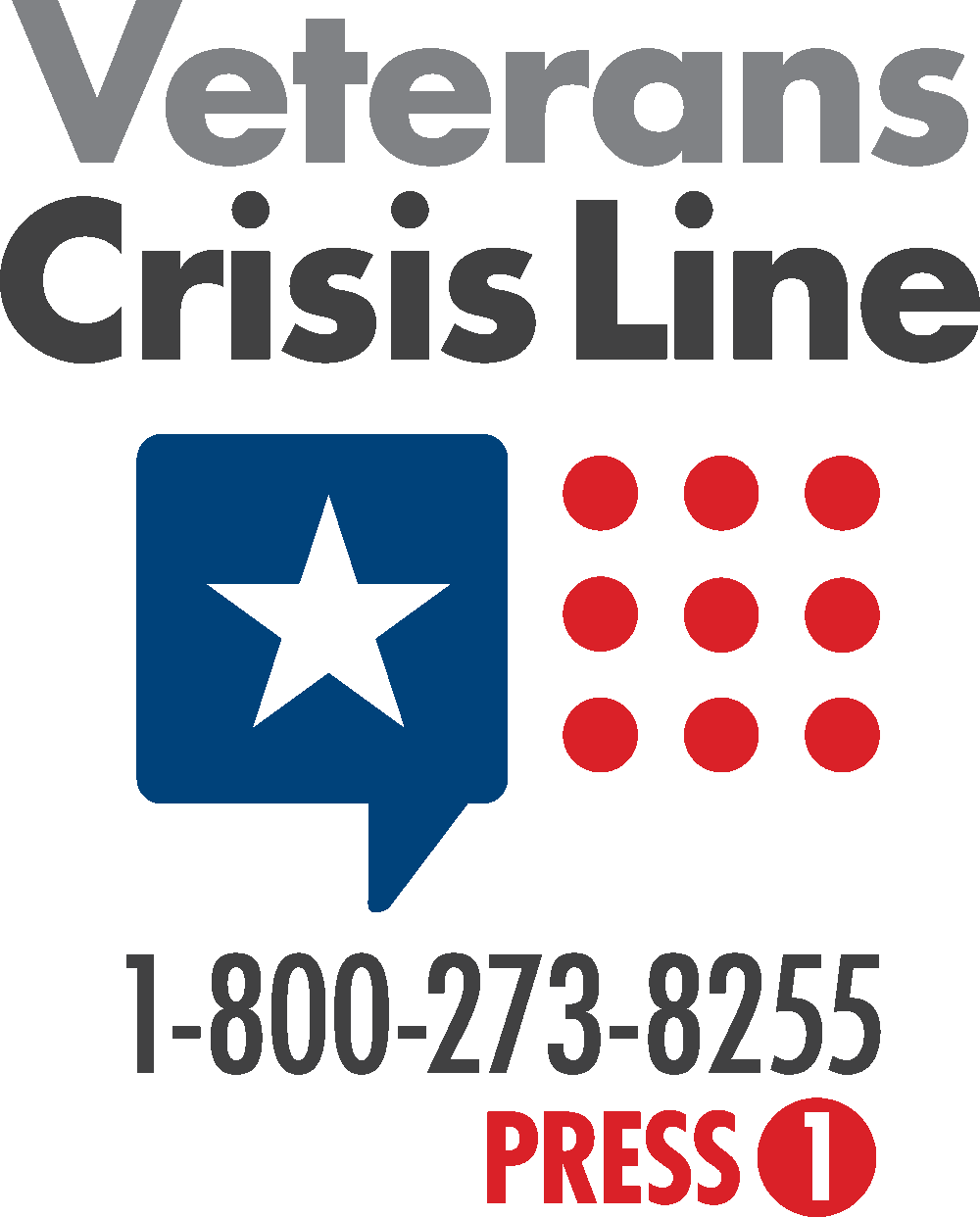
Veterans Crisis Line. Source: Department of Veterans Affairs.
In an evaluation of the effectiveness of the National Suicide Prevention Lifeline, 1,085 suicidal individuals who called the hotline completed a standard risk assessment for suicide, and 380 of those completed a followup assessment between 1 and 52 days after the initial assessment. Researchers found that over half of the initial sample had a plan for their suicide when they called. Among followup participants, there was a significant decrease in psychological pain, hopelessness, and intent to die between initiation of the call (time 1) to followup (time 3). Between time 2 (end of the call) to time 3, the effect remained for psychological pain and hopelessness, but was not significant for intent to die, suggesting that greater effort at outreach during and following the call is needed for callers with high levels of suicide intent (Stone et al., 2017).
Community Engagement
Community engagement approaches may involve residents participating in a range of activities, including religious activities, community clean-up and greening activities, and group physical exercise. These activities provide opportunities for residents to become more involved in the community and to connect with other community members, organizations, and resources, resulting in enhanced overall physical health, reduced stress, and decreased depressive symptoms, thereby reducing risk of suicide (Stone et al., 2017).
Among communities disproportionately affected by suicidal behaviors, a one-size-fits-all approach to suicide prevention and community engagement does not work. Messages, interventions, and programs must be tailored to each community:
- Involve community members and leaders from the beginning and respect them as experts on their own community.
- Become familiar with the community’s history, risk and protective factors, cultural norms around language and communication, beliefs about death, and definition of the problem.
- Avoid viewing one or a few members of a community as representative of an entire demographic group.
- Put values of inclusion and equity front and center in decision making and program design.
- Include accessibility concerns such as transportation, cost, language translation, location, space, and materials for people with disabilities.
A recent workshop held in Iqaluit, Nunavut (Arctic Canada) provided guidance on ways to prevent suicide among Indigenous peoples—much of which can be applied to any community engagement effort. Key themes included:
- Acknowledge the impact of colonization.
- Recognize the effects of rapid social and environmental changes on mental wellness and suicide that have taken place in the recent past.
- Be aware of the great variation of suicide rates across communities, even within a single jurisdiction, and the importance of understanding the role of resilience.
- Understand that successful prevention strategies must be community-based and should integrate Indigenous ways of knowing.
- Recognize the importance of involving youth in developing solutions, tightening their relation to the land, and creating strong linkages with Elders and culture.
- Acknowledge the need to move from intention to action and from action to impact. (NIMH, 2017)
Healing of the Canoe
A good example of a program stressing community involvement while respecting local customs and beliefs is the Healing of the Canoe Project, a collaborative project between the Suquamish Tribe, the Port Gamble S’Klallam Tribe, and the Alcohol and Drug Abuse Institute at the University of Washington. It is a curriculum for Native youth focused on suicide and substance abuse prevention. The program uses the Canoe Journey as a metaphor, providing youth the skills needed to navigate their journey through life without being pulled off course by alcohol or drugs—with tribal culture, tradition, and values as compass to guide them and anchor to ground them (Healing of the Canoe, 2019).

Suquamish
Port Gamble S’Klallam
Video: What Is the Healing of the Canoe? [3:34]
https://www.youtube.com/watch?v=waQ4eK7wfb8
Rising Sun
Another innovative, community-based suicide prevention program is Rising Sun (Reducing the Incidence of Suicide in Indigenous Groups—Strengths United through Networks). The program has developed a toolkit, identifying common outcomes to be used in evaluating suicide prevention efforts and interventions across Arctic states. Common outcomes and their measures, developed through engagement with Indigenous peoples’ organizations and community leaders, as well as mental health experts, facilitate data sharing, assessments, and interpretation of interventions across communities in the Arctic region (NIMH, 2017).
The goal of Rising Sun is to generate shared knowledge to help health workers better serve their communities and help policy-makers measure progress, evaluate interventions, and identify regional and cultural challenges. Arriving at common outcomes, is especially important in the Arctic, where the vast geography, high number of remote communities, and breadth of cultural diversity pose challenges for systematic approaches to suicide prevention (NIMH, 2017).
