*This course has been retired. There is no replacement course at this time. Please click here to view the current ATrain course listings.
Darrell, a 62-year-old male patient has been admitted to the hospital for respiratory distress after an exacerbation of his COPD during flu season. He also has uncontrolled diabetes mellitus, hypertension, and a lower lobe pneumonia. He has been on a ventilator (assist control) for five days. He is receiving antibiotics for the pneumonia.
Upon completion of the morning assessment, the nurse notices a thick white coating on his tongue and mouth and around the endotracheal tube. She plans to provide oral care several times during her shift. Later in the day she notices that the white coating on the tongue is difficult to scrape off but thinks it is just a stubborn film on his tongue. Or is it something more?
- Did you recognize the clinical signs of an oral yeast infection?
- What risk factors did Darrell have to increase the development of oral candida?
- What tests are done to diagnose candida? What are the causes?
- How is it transmitted? Is it infectious?
- What are the different types of yeast infections?
- What is the nurse’s role in treating fungal infections?
- What prevention and treatment strategies are available?
- What is the role of healthcare professionals in helping people avoid common yeast infections?
- Do you have yeast in and on your body? If so, is it in control?
If you struggled to answer these questions, we will discuss each of these issues to prepare you to begin your own assault against candida yeast infections.
Yeasts That Infect
Yeast infections are also known as fungal infections and are caused by the fungus candida. Yeast are single celled organisms and classified in the biology Kingdom Fungus, which also includes mushrooms and molds. It is different from other microorganisms such as bacteria, protozoa, and amoeba. Candida is the genus level name for a fungus, and there are more than 150 different kinds of candida (McCombs, n.d.). Healthcare workers are often more familiar with Candida albicans, a common fungal skin infection, but there are dozens of variations and types of fungal infections. A very serious fungus that has developed a resistance to current antifungal treatments is called Candida auris. It is because of this growing threat within hospitals and for long-term care patients, that there is a need for healthcare workers to be better informed about candida.
Candida auris
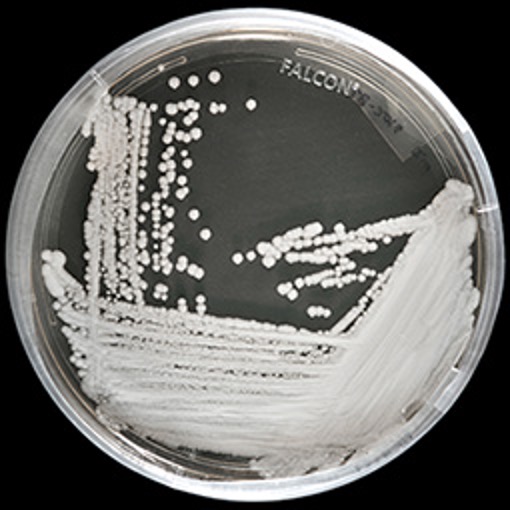
Source: NHS.UK.
Most fungi dwell normally within and on-top of the human body creating a natural competitor against normal bacteria, which is also on and in the body. Candida is known as an opportunistic microbe, and given the right opportunity, candida yeast can become overgrown and cause an infection (Vázquez-González et al., 2013). When the normal human environment is disrupted, and the human immune system is diminished candidiasis may result. Candidiasis is any fungal infection due to any type of candida that has become out of control in the human body (Huether & McCance, 2008).
Fungal disorders are also called mycoses and when caused by a topical fungus affecting the epidermis, the disorder of the skin is called tinea. The second Latin name identifies the area of the body infected ; consider Tinea capitus, which is a fungal infection of the scalp; Tinea corporis, which is a yeast infection of the body; Tinea pedis, which is a fungal infection of the feet. Other names for candida include moniliasis and oidomycosis.
Candida albicans

Source: Shutterstock.
Candida albicans is a gram-positive budding yeast, and of more than twenty types of fungal infections it is the most common. Like other opportunistic pathologic yeast, Candida albicans is found in humans where ideal growth environments exist. Candida exists as normal flora in the human intestines. It grows within the gastrointestinal tract from the mouth through the small intestines and is found in the mouth of up to 60% of healthy adults (Erdogan & Rao, 2015). Albicans is one of the most common fungal species to be isolated on medical devices and on human tissues. It is one of several forms that cause candidiasis. The other five most common forms of candida are C. tropicalis, C. parapsilosis, C. glabrata, C.krusei, and C. auris, which combined are responsible for up to 90% of all human candidiasis (Martins et al., 2014).
Candida auris, another type of yeast, has become drug resistant and is spreading in healthcare facilities, quickly becoming a serious concern. The Centers for Disease Control and Prevention (CDC) track candida infections through hospital reporting, in order to understand the transmission, incidence, and susceptibility to treatment. When any pathogen begins to become resistant to current medications, the CDC becomes actively engaged in tracking and creating standard guidelines for treatment across the nation.
Types of Common Human Yeast Infections
Source: Cash & Glass (2014). Images: Wikimedia Commons. Table Design: Author.
no photo available
Cellulitis from C. auris
Location
Any topical skin area
Clinical appearance
Redness, heat and discomfort in affected area, poorly demarcated.
Treatment
Topical antifungals
Intertrigo: Diaper Rash

Diaper rash. Source: Wikimedia Commons. Creative Commons Attribution-Share Alike 3.0 Unported
Diaper rash
Location
Genitals and buttocks of babies
Clinical appearance
Red, warm, burning diffuse rash on buttocks and vaginal skin folds of girls.
Treatment
Topical antifungal
no photo available
Invasive candidiasis
Location
Through bloodstream
Treatment
Oral or IV antifungals: fluconazole, itraconazole, or amphotericin B.
Intertrigo: Axilla (Armpit)

A pathogenic bacterial growth in the armpit. Source: Wikimedia Commons. Public domain.
Intertrigo
Location
Yeast infection in skin folds of breast, groin and armpits.
Clinical appearance
Red, itchy, small bumps with no defined borders.
Treatment
Topical or oral antifungals x 14 days.
no photo available
Interface dermatitis (ID)
Location
Rash on one part of body in response to a fungal infection elsewhere on the body.
Clinical appearance
Red, itchy, blisters on the skin
Treatment
Oral antifungal
no photo available
Thrush (oropharyngeal candidiasis)
Location
Oral cavity
Clinical appearance
White or yellow coating on tongue, lips, gums, roof of mouth and inner cheeks. Redness and soreness in the mouth and throat. Cracking at the corners of the mouth. Sometimes pain when swallowing.
Treatment
Oral swish and spit antifungals
Oral care/toothbrushing
Rinsing after oral glucocorticoid inhaler use Ex. Nystatin, clotrimazole and fluconazole.
Swish with oral chlorhexidine mouthwash.
no photo available
Tinea barbae
Location
Chin and beard of men
Clinical appearance
Flaky, scaly and itchy chin. Similar to tinea corporis or ringworm.
Treatment
Oral antifungals as topical creams and lotions are not effective.
Tinea Capitis

Tinea capitis. Source: Gholamreza Baqeri. Wikimedia Commons. Creative Commons Attribution-Share Alike 4.0 International.
Tinea capitus
Location
Scalp
Clinical appearance
Itchy, scaly bald patches on the head.
Treatment
Ketoconazole 2% shampoo
Tinea Corporis: “Ringworm”

Ringworm in the armpit area. ProjectManhattan. Source: Wikimedia Commons. Creative Commons Attribution-Share Alike 3.0 Unported.
Tinea corporis (ringworm)
Location
Epidermis of the skin anywhere on the body
Clinical appearance
Flaky, scaly and itchy. Circle or ring-shaped with clear center. May have bumps and red patches that turn in to the shape of circles. Small, erythematous and vesicular patches with slightly elevated border forming a ring.
Treatment
Topical antifungal
no photo available
Tinea cruris (jock itch) genital candidiasis
Location
Genitals male & female
Clinical appearance
Itchiness in the vagina, redness and swelling of the vagina and vulva. Pain and burning on urination, discomfort during sex (dyspareunia). Thick, white “cottage-cheese” or “curd-like” discharge from vagina.
Treatment
Intravaginal antifungal suppository, tablet or cream.
no photo available
Tinea manis (hands)
Location
Hands
Clinical appearance
Dry, flaky and peeling hands
Treatment
Topical antifungal cream and lotions for moisturizing the dead dry skin afterwards.
Tinea Pedis

Vesicular Athlete’s Foot. Soodleksw. Source: Wikimedia Commons. Public domain.
Tinea pedis (onychomycosis; Tinea unguium)
Location
Foot and nails of the toes
Clinical appearance
Thickened, brittle and white not clear nail. Great toe is most common. Nail bed may separate (onycholysis).
Treatment
Topical and oral antifungal fluconazole 150-300 mg weekly for 2-3 months. Lamisil weekly for several weeks; terbinafine. Topicals are generally not effective.
Tinea Versicolor
Tinea versicolor on the abdomen of a female patient. Sarah Korf. Source: Wikimedia Commons. Creative Commons Attribution-Share Alike 2.0 Generic.
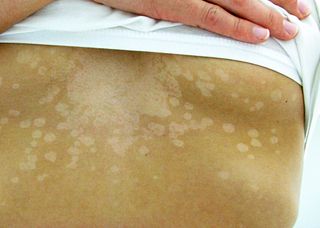
Tinea versicolor (pityriasis versicolor)
Location
Trunk of body front and back
Clinical appearance
Hypopigmented round macules on chest/shoulders/back; appear after skin is tanned from sun. Often asymptomatic
Treatment
Topical selenium sulfide (Selsun Blue shampoo); Ketoconazole (Nizoral) BID x 2 weeks, Oral antifungals
* * *
Skin yeast infections can also appear as a red, flat rash with scalloped edges. Satellite lesions are extensions of the original yeast that grow to extend the rash. As noted above, tinea infections are identified by their location on the body.
Pathology of Candida
Candida are organisms that can be dimorphic or polymorphic, meaning their shape can appear as a single cell or become more pathologic with multiple extensions or filaments from a cell. Candida yeasts are part of the normal pathogens on the body, found on the skin and throughout the intestinal flora, and are kept within ideal limits by natural competition from other microorganisms such as bacteria.
Yeast grow best in humans under conditions of warmth, moisture, and access to sugar for energy. Skin folds that are warm and moist such as the mouth, genitals, or a baby’s diaper region, are ideal reservoirs for yeast growth. Skin folds of obese people, such as under breasts or armpits, are common growth areas for candida. The vagina of females is also an ideal location for yeast overgrowth given the right conditions. Yeast prefer sugar for food and grow well with diets high in sugar, such as in people with diabetes mellitus and uncontrolled blood sugar levels.
Did You Know. . .
Not all yeasts grow in warm areas; consider the mold that grows on your refrigerated food that has been kept too long.
Yeast cells can be seen in different morphologies, or appearances. When they appear ovoid under a microscope they are known as yeast cells. If they look like a cactus with multiple branches, they are known as hyphae; when they are a combination of both round cells and elongated growths they are called pseudo hyphae.
Pseudo Hyphae of Candida albicans
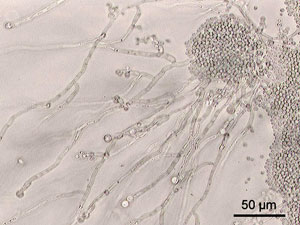
By Y tambe - Own work, CC BY-SA 3.0, https://commons.wikimedia.org/w/index.php?curid=124722. Source: Wikimedia Commons.
When the yeast is in round cells, the cells can move easily to different areas of the body; whereas, when they are in hyphae mode, the filaments can more easily invade surrounding body tissues and create a broader infection. Yeast generally prefers to live on the skin and mucus membranes. When it grows out of control, it impacts the squamous epithelium of the top layer of the skin. Yeast can destroy skin cells and keratin and deposit its own protein layer, which appears as a white cottage-cheese-like appearance, as seen in vaginal and oral infections.
As it destroys topical skin or mucus layers of the host, it is known as pseudomembranous candidiasis. This is more common in those with a weakened immune system, such as infants and elders; those who are immunosuppressed (such as those with diabetes or HIV/AIDS); or those taking medications that may suppress the immune system, such as inhaled steroids, chemotherapy, or radiotherapy.
Another condition is called erythematous candidiasis, which is due to a change in the level of competition between yeast and normal bacteria. Taking antibiotics or smoking can decrease normal colonizing levels of bacteria but not have a negative impact on yeast, so the yeast cells grow out of control. The body’s normal first reaction to any overgrowth is inflammation and an increase in blood flow to the area to deliver antibodies and oxygen. The result is a reddened and painful skin area from vasodilation. The pain is due to the swelling tissues that push on the nerve endings.
When identifying characteristics of yeast, in addition to the morphology, is the existence of adhesins, which make the yeast stick to surface areas. Adhesins are made of glycosyl phosphatidyl inositol, which has surface sticky glycoproteins that allow it to adhere to the surface of other microorganisms and inorganic surfaces. Invasins* allow the yeast to invade other tissues such as epithelial tissues and cells of the skin.
*Invasins, a class of proteins associated with the penetration of pathogens into host cells. Invasins play a role in promoting entry during the initial stage of infection.
In addition to the typical body locations of the mouth, esophagus, skin, and vagina, yeast becomes dangerous when growing on mechanical devices such as central venous catheters used by patients in hospital and long-term medical facilities. The candida forms a biofilm on the catheter and devices and can prolong a hospital stay. The biofilm can also break off and move to other areas. If it enters the bloodstream, it can become septic for the patient. Depending on where the mechanical device is, the yeast may have easy access to heart valves, kidneys, and the brain.
Additionally, candida secretes hydrolases such as protease, phospholipase, and lipase, which break down cells of the host and make it easy to penetrate and take up nutrients from the host environment. An example is intestinal candida that becomes overgrown, causing post-meal abdominal bloating and fatigue as the yeast grow and use up resources from the host.
Metabolic adaptation is flexible for candida, as they will consume energy from food sources in the gut of the host or can create new fuel through gluconeogenesis. When an overgrowth of yeast occurs, it is said the yeast colonize and then invade human tissue or mucous and can dangerously pass into the bloodstream.
Friendly Yeast
Not all yeast is bad. If you have ever baked bread from “scratch,” you will recall that you add a tablespoon of baker’s yeast to warm water and a tablespoon of sugar. If the water is too hot the yeast won’t grow, and the mixture will make flat, hard bread. With the right temperature of warm water, in just minutes you see bubbles forming as the yeast become activated. These yeast organisms begin to digest the sugar and release gas, accounting for the bubbles. If you add salt, the reaction begins to slow down; yeasts are killed by salt, which disrupts their cell structures. Upon adding flour and other ingredients, the yeast continues to grow until it is ready to be baked. The high baking temperature kills the yeast and the growth stops.
In essence, this process of using yeast to bake bread is similar to the yeast growth within and on our own bodies. Given a warm and moist climate, yeast grow. When exposed to natural competitors, such as bacteria, yeast is held at bay. If deprived of warmth, moisture, and sugar, they cannot flourish. This process suggests strategies for prevention, which we’ll discuss later.
Curative Power of Yeast: Penicillin
Now the positive side of yeast must be told. Yeast are a vital organism in the mix of our gastrointestinal normal flora that help with our digestion of food. Yeast was also key to the discovery of their effectiveness against bacteria, which can harm us. In 1928, Alexander Fleming is known for his discovery of the effectiveness of the penicillin mold against bacteria. How he discovered a “cure” against staphylococcus bacteria was due to yeast. As a Scottish bacteriologist in London, he was studying the bacteria on an agar growth plate that he placed by an open laboratory window at London’s St. Mary’s Hospital. Days later he realized a blue-green mold yeast, known as Penicillium notatum, had blown through the window and contaminated the petri dish. Upon further examination, he saw that the yeast had grown onto the bacteria and killed it and there was a clear ring or around the yeast where bacteria couldn’t grow (Newman, 2019).
Believing that penicillin would not last long enough in humans to kill bacteria, he looked for help in purifying the promising drug. The research continued in 1934 at Oxford University by advanced scientists Howard Florey, Ernst Chain, and Norman Heatley, who were able to purify and test it successfully in mice, and then in humans. Thankfully, the combined efforts of scientists and yeast produced a huge blessing to mankind—penicillin, which effectively kills harmful bacterial infections. Ironically, in the Nobel Prize acceptance speech of Alexander Fleming, he warned that overuse of the penicillin may lead to bacterial resistance, which has since occurred. In summary, yeast can be both foe and friend.
Apply Your Knowledge
How would you explain both the advantages and disadvantages of yeast?
