*This course has been retired. There is no replacement course at this time. Please click here to view the current ATrain course listings.
Clinical Symptoms
The clinical symptoms vary depending on the location affected by the yeast. From head to toe, the most common sites for fungal infections include the scalp, skin, mouth, gastrointestinal tract, genitourinary tract, vagina, and nail beds of the hands and feet. The most dangerous type of fungal infection is an invasive infection (or systemic infection) that enters the bloodstream; it is called candidemia. Fungal infections that originate in the oral cavity and extend into the esophagus have a higher potential to become an invasive infection because they become systemic.
Classically, yeast infections look red, warm, sometimes scaly, and continue to spread if not treated. They can be itchy but not generally painful unless directly on the skin of the genitals and buttocks. They generally do not cause a fever but if not treated can cause a sense of malaise and gastrointestinal upset and bloating if in the GI tract. To review the specific symptoms, let’s look at each of them based on locations of the body.
Skin Infections
Topical skin infections include the scalp, head, face, back, chest, axilla, under the breast or in other skin folds, and anywhere on the body from head to toe. When a yeast infection develops on the skin it generally appears red, scaly and inflamed with symptoms of itching and burning, however unique configurations can occur that help diagnose the yeast. An example is the classic shape of a ringworm infection on the skin, called Tinea corporis. Ringworm is misnamed because there is no actual worm on the skin, rather the unique shape caused by the dermatophyte yeast. Superficial skin infections by yeast at the epidermis are caused by fungi called dermatophytes.
Internal Infections
Because yeast is very common as topical normal flora, skin infections can easily develop given the right environment. Additionally, the moist and warm internal environment of the body offers ideal growth for candida.
Vaginal Candidiasis

Speculum exam in candidal vulvovaginitis, showing thick, curd-like plaque on the anterior vaginal wall. A slightly erythematous base is visible close to the center of the image, where some of the plaque was scraped off. Mikael Häggström. Source: Wikimedia Commons. Creative Commons CC0 1.0 Universal Public Domain Dedication.
From head to toe, internal candida infections commonly occur in the mouth, known as oral thrush. It appears as a white sticky coating and can even appear hairy from the extensions of hyphae. It can be easily treated with an oral antifungal, such as a swish and swallow medication. Good oral hygiene for patients on ventilators and rinsing after taking an inhaled glucocorticoid can help prevent this.
Gastrointestinal yeast infections often present as GI bloating, nausea, vomiting, diarrhea and generalized malaise. In diets high in sugar, the GI yeast can easily grow and contribute to belly fat, constipation, poor metabolism of food, and further infection (García-Elorriaga & Rey-Pineda, 2013).
A very common internal yeast infection occurs in the vagina. Symptoms include vaginal itching, foul fishy odor, and white cottage-cheese–like discharge. Upon visualization using a speculum, it is easy to diagnose because of its white discharge. It can be cultured for definitive diagnosis, however, most clinicians will easily recognize it and treat it with antifungals intravaginally, or orally.
Skin yeast infections can also appear as a red, flat rash with scalloped edges. Satellite lesions are extensions of the original yeast that grow to extend the rash. As noted above, tinea infections are identified by their location on the body.
Diagnosing Candida
KOH Test on a Candida Specimen
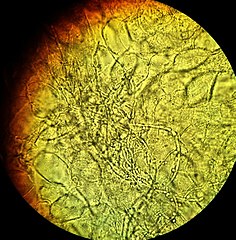
KOH test on a vaginal wet mount showing slings of pseudohyphae of Candida albicans surrounded by vaginal epithelial cells conferring a diagnosis of candidal vulvovaginitis. Mikael Häggström. Source: Wikimedia Commons. Creative Commons CC0 1.0 Universal Public Domain Dedication.
Often a candida infection is easily identifiable but a definitive diagnosis can only be done via a microscope or culturing. A skin scraping or swab sampling can be placed under a microscope, which reveals the typical and classic hyphae or fern-like growths. A single drop of potassium hydroxide, KOH, is often added to the microscopic slide, which dissolves the human skin cell wall and exposes the yeast and identifiable hyphae.
When using the culture method, a simple sterile swab of the infected surface is wiped on the culture medium (e.g., a blood agar petri dish) and allowed to grow in an incubated temperature of 98.6ºF for several days. Yeast and bacterial colonies easily occur within 3 to 5 days. Because candida is part of the normal flora, identifying a true infection is based on the various candida species that may grow in an agar culture, the agar fermentation, and assimilation tests.
Agar Plate Culture of C. Albicans

Source: CDC Public Health Image Library. Public domain.
Clinicians can often recognize a yeast infection based on its location and classic morphology and do not order diagnostic tests but treat right away. For example, when a practitioner sees the classic ring worm formation a topical antifungal is ordered. Occasionally a clinician may observe the skin directly with an ultraviolet light known as a Wood’s lamp. The spores of the yeast become fluorescent with a Wood’s lamp and appear blue-green when exposed to ultraviolet light.
For invasive agents within the bloodstream, non-culture candida detection tests can be done with antigen testing such as the Beta-D-Glucan, or candida PCR, which detects candidal DNA. Candida heat-liable-antigen assays—D-arabinitol assay or D-inositol assay—can also be used based on the laboratory’s preference and equipment. Immunological tests such as skin tests can also be performed.
Treatment of Yeast
Prompt treatment is key to quick destruction of out of control yeast.
Pharmacological treatment of candida depends on the location. The severity of the fungal infection also dictates the type of antifungal to be used for treatment. An acute fungal infection on the skin can often easily be treated with topical antifungals, however if they have become extensive or chronic, often long-term topical agents in addition to oral agents need to be prescribed.
For most acute fungal skin infections, topical antifungals commonly used include:
- Clotrimazole (Lotrimin, Mycelex)
- Ketoconazole (Xolegel)
- Miconazole (aloe vesta antifungal, azolen, baza antifungal, carrington antifungal, critic aid clear, cruex prescription strength, dermafungal, desenex, fungoid tincture, micaderm, micatin, micro-guard, miranel, mitrazol, podactin, remedy antifungal, secura antifungal)
- Terbinafine (Lamisil)
Prescription topical agents for resistant or extensive infections may include:
- Ciclopirox (Loprox, Penlac)
- Ketoconazole (Nizoral)
- Oxiconazole (Oxistat)
Administration of these antifungals are generally via a cream that is applied twice daily for 2 to 4 weeks. The length of application depends of course on the severity of the yeast and if the infection is acute or chronic. A topical ringworm infection may require treatment for 14 days, however a topical great-toenail fungal infection may require months of treatment and be very difficult to get rid of as the yeast have become embedded in the matrix of the nail.
For chronic yeast infections, an oral antifungal should be given and may include (Jaliman, 2019):
- Fluconazole (Diflucan)
- Griseofulvin (Fulvicin P/G, Fulvicin U/F, Grifulvin V, Gris-Peg): oral and spray. May need 8-10 weeks for effect. Cannot take during pregnancy or breastfeeding. May cause birth defects. Men should use condoms for up to six months after treatment to prevent birth defects.
- Itraconazole (Sporanox): 1-2 weeks. Not for use in elderly and children with liver disease.
- Ketoconazole (Nizoral)
- Terbinafine (Lamisil): once daily x 4 weeks
All oral antifungals are processed by the liver’s first-pass effect, which may cause nausea, diarrhea, indigestion, headache, dizziness, and even rashes. These oral antifungals are contraindicated for those with liver disease and lupus.
For severe fungal infections that impact a mechanical device, prescription IV antibiotics that are used include:
- Amphotericin
- Azole antifungals
- Echinocandins such as micafungin
Removal of the mechanic device or tube should also be a priority to avoid entry of the pathogen into the bloodstream.
Alternative medicines and folk medicine have been used to treat yeast infections. Although not endorsed by the American Medical Association, patients may be using these remedies and healthcare professionals should be aware of them. Many studies exist demonstrating the effectiveness of various essential oils(e.g., oregano oil) and even food substances (Alves-Silva, 2013). Studies have even shown effectiveness of apple cider vinegar against topical and intestinal yeasts.
