Synthetic designer drugs are basically human experiments without informed consent. Every drug we take that is prescribed by a physician has gone through the most rigorous testing: First in animals. . . and then in humans. And in humans it is done so carefully—you measure the doses, you first find out if there’s any dose that becomes toxic. Then you go into trials with people who are sick to see if it helps them. In the case of designer drugs none of these precautions have been taken, none of the care has been taken.
Chemists can make anything, anywhere in the world. Some can be poisonous, downright toxic, some can promote addiction, some can destroy brain cells—you don’t know. You are simply walking into a cave without a flashlight, and you are hoping there aren’t bears, or scorpions, or rabid bats, or chasms, or crevices that you can fall into. That is why I call it a human experiment without any knowledge on what these drugs can promote in your brain and to the rest of your body.
Dr. Bertha Madras
Harvard Medical School
Over the last decade, designer drugs have exploded onto the illicit drug scene. When their molecular structure is published, amateur and professional chemists reproduce these drugs, alter them to increase their potency, and flood the market with dangerous untested compounds that are undetectable by most known tests. Very little is known about the effects these drugs will have on the human nervous system because their chemical structure has been tweaked and modified so rapidly and so often that it is impossible for researchers and law enforcement to keep up with the changes.
Designer drugs are synthetic compounds whose molecular structures have been modified based on chemically similar illicit drugs. The newly created substances can often be purchased legally because their modified chemical structures are not covered under existing drug laws. Since, in many cases, designer drugs are not yet illegal, they are inaccurately referred to as “legal highs” or “herbal highs.”
Designer drugs are characterized by the U.N. Office on Drugs and Crime as novel* psychoactive substances (NPS) and are defined as “substances of abuse, either in a pure form or a preparation, that are not controlled by the 1961 Single Convention on Narcotic Drugs or the 1971 Convention on Psychotropic Substances, but which may pose a public health threat” (UNODC, 2014a).
*Novel: Materials identified but never reported in scientific or patent literature—made by changing or modifying known materials.
Designer drugs can be placed into eight groups, although there is some overlap and there are differences in definitions among researchers, law enforcement, and clinicians. This course will focus on three of the groups: (1) synthetic cathinones (bath salts), (2) synthetic cannabinoids, and (3) synthetic hallucinogens, primarily NBOMe.
The other five groups are beyond the scope of this course, but they are listed briefly as follows:
- Aminoindanes: similar to amphetamine; first developed in the 1970s for their analgesic and bronchodilation properties. Aminoindanes have a strong effect on the release and re-uptake of serotonin. This group of designer drugs includes highly potent selective serotonin releasing agents such as MDAI and 5-IAI—and ETAI, which is an analogue of fenfluramine, a substance formerly marketed as an appetite suppressant. Street names of MDAI include MDAI gold, while 2-AI has been found in party pills known as pink champagnes (UNODC, 2014b).
- Ketamine and phencyclidine-type substances: closely related to phencyclidine (also known as PCP or “angel dust”). Phencyclidine was originally investigated as an intravenous anesthetic in the 1950s but was later withdrawn due to undesired hallucinogenic and delirium effects. Following the withdrawal of phencyclidine, ketamine was synthesized as an anesthetic in 1962, and subsequently patented in Belgium and in the United States. In the early 1970s, ketamine was marketed as a medical alternative to phencyclidine. Ketamine and phencyclidine have similar modes of action, affecting a range of central neurotransmitters. Ketamine is frequently sold as ecstasy. Street names for ketamine include K, special K, kit kat, tac, tic, cat valium, cat tranquilizer, vitamin K, ket, and super K (UNODC, 2014b).
- Piperazines: Although not derived from plants, piperazines are so named because of their chemical similarity to piperidine, a part of the chemical piperine, found in the black pepper plant. Some piperazines have been evaluated as potential therapeutic agents but never brought to market. One piperazine, BZP, was initially developed as a potential antidepressant but was found to have similar properties to amphetamine and therefore liable to abuse. In the 1980s, BZP was used in Hungary to manufacture piberaline, a substance marketed as an antidepressant, but later withdrawn (UNODC, 2014b).
- In the late 1990s, BZP emerged in New Zealand as a “legal alternative” for MDMA (ecstasy) and methamphetamine. In Europe its use was first reported in Sweden in 1999, but it only became widespread as a novel psychoactive substance from 2004 onward until controls over the substance were introduced by the European Union in 2008. Some of the generic names for these substances include pep pills, social tonics, or simply party pills (UNODC, 2014b). Piperazines are frequently sold as ecstasy and are also used in the manufacture of plastics, resins, pesticides, brake fluid, and other industrial materials.
- Plant-based substances (khat, kratom, salvia divinorum): the khat shrub (Catha edulis) of the Celastraceae family is a plant native to the Horn of Africa and the Arabian Peninsula. Khat (pronounced “cot”) chewing is a social custom there. The psychoactive effects result from the release of cathinone and cathine alkaloids when chewed. The khat shrub became known to Europeans in the late eighteenth century and the active constituents of the plant were isolated later; a “katin” alkaloid was identified in 1887, “cathine” in 1930, and “cathinone” in 1975. In Europe and North America, khat was traditionally used by migrant communities from Ethiopia, Kenya, Somalia, and Yemen, but in recent years its use has spread to Bahrain, Canada, Finland, Ireland, Italy, New Zealand, Norway, Oman, and the United States. Hong Kong reported that khat emerged on their markets in 2009, and it was the second most popular plant-based substance, after salvia divinorum, reported by Member States from 2009 to 2012. Catha edulis is not under international drug control, but cathinone and cathine are listed in Schedules I and III, respectively, of the 1971 Convention (UNODC, 2014b).
- Tryptamines: while some naturally occurring tryptamines are neurotransmitters (serotonin, melatonin, and bufotenin), most are psychoactive hallucinogens found in plants, fungi, and animals. Naturally occurring psilocybin became widespread in the late 1950s in the United States, while synthetic tryptamines appeared on illicit drug markets in the 1990s. Recently, a group of synthetic tryptamines that are derived from DMT and other naturally occurring tryptamines have been reported as novel psychoactive substances. Street names for some tryptamines include foxy-methoxy, alpha-O, alpha, O-DMS, and 5-MEO. Natural tryptamines are available in preparations of dried or brewed mushrooms, while tryptamine derivatives are sold in capsule, tablet, powder, or liquid form (UNODC, 2014b).
Cathinones, Cannabinoids, and Hallucinogens
In the United States (and internationally) synthetic cathinones, synthetic cannabinoids, and synthetic hallucinogens are manufactured and distributed to circumvent drug laws and evade interdiction.* They are intentionally marketed and distributed for recreational use by exploiting inadequacies of existing controlled substance legislation (Weaver et al., 2015).
*Interdiction: A continuum of events focused on interrupting illegal drugs smuggled by air, sea, or land (U.S. Department of Defense).
These compounds (see table below) have evolved rapidly and have largely evaded legal regulation and detection by routine drug testing. Young adults are the primary users, but trends are changing rapidly and use has become popular among members of the military. Acute toxicity is common and multiple deaths have been reported with each of these types of designer drugs (Weaver et al., 2015).
Non-chemists can easily synthesize these compounds with readily available raw materials, or they can obtain the synthetic compounds directly. The chemicals are packaged with labels that do not accurately describe product contents, which may vary substantially regarding chemical content and concentration. Labels often include the phrase, “not for human consumption,” in an attempt to avoid legal risk (Weaver et al., 2015).
|
Cathinones, Synthetic Cannabinoids, and Synthetic Hallucinogens |
|||
|---|---|---|---|
|
Drug class |
Chemical name |
Chemical origin |
Slang names |
|
Cathinone |
Mephedrone |
Cathinone |
Bath salts (Ivory Wave, Vanilla Sky) meow-meow, M-Cat |
|
Methylone |
|
||
|
Methylenedioxypyrovalerone (MDPV) |
Sextacy |
||
|
Naphyrone |
NRG-1 |
||
|
Cannabinoid |
JWH-018; JWH-073; JWH-250 |
Laboratory of J.W. Huffman |
Spice, K2, K9, Aroma, herbal highs, Scooby Snax |
|
CP 47,497; CP 47,497-C8; CP 59,540; cannabicyclohexanol |
Pfizer laboratory |
||
|
HU-210 |
Hebrew University laboratory |
||
|
UR-144 |
CB2 receptor agonist |
||
|
Oleamide |
Fatty acid |
||
|
XLR-11, AKB-48 |
|
||
|
AM-2201, AM-694 |
|
||
|
Hallucinogen |
25I-NBOMe |
Free University of Berlin |
N-bomb, Solaris, Smiles, Cimbi-5 |
|
25B-NBOMe |
|||
|
25C-NBOMe |
|||
Although the emerging designer drug trend was initially recognized by increased calls to U.S. poison control centers, the incidence of designer drug problems in emergency departments, hospitals, and other medical settings is largely unknown. Only a small percentage of those using designer drugs will come into contact with the healthcare system, but consequences of use can be severe (Weaver et al., 2015).
The growing popularity of designer drugs relates to factors such as novelty, marketing, and accessibility. Designer drug packaging is colorful and attractive, with enticing names for the products to attract younger individuals. Designer drugs are sold without age restriction. Widespread availability, including purchase via the Internet, has contributed to expanded use (Weaver et al., 2015).
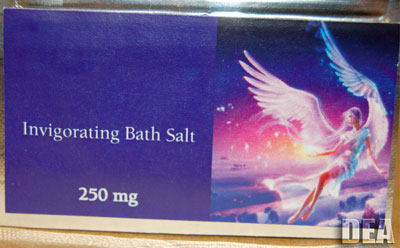
Colorful packaging attracts young users of designer drugs. Source: Drug Enforcement Administration.
Clinicians should keep designer drugs in mind when evaluating substance use in young adults or in anyone presenting with acute neuropsychiatric complaints. Treatment of acute intoxication involves supportive care targeting signs and symptoms. Long-term treatment of designer drug use disorder can be challenging and is complicated by a lack of evidence to guide treatment. Familiarity with designer drugs can help clinicians recognize common adverse reactions and life-threatening consequences (Weaver et al., 2015).
Designer drugs affect the brain in a number of ways. Bath salts—synthetic cathinones—act on transporters for the neurotransmitters dopamine, serotonin, and norepinephrine; cocaine, ecstasy, and amphetamines produce their psychoactive effects through these same transporters. Similarly, the synthetic cannabinoids mimic marijuana by activating the same cannabinoid receptors as THC (tetrahydrocannabinol), the main psychoactive component in marijuana (NIDA, 2015a).
Animal studies have shown that designer drugs cause behavioral effects that resemble the drugs of abuse whose mechanisms they share. However, slight differences in chemical structure cause some different effects. For example, the synthetic cathinone MDPV (discussed in the next module) acts on the dopamine transporter 50 times more strongly than cocaine. Synthetic cannabinoids also act on the nervous system differently than non-synthetic cannabis; they are shorter-lasting than THC and are metabolized differently, which could increase potential for abuse and for medication interactions and other toxic effects. Further understanding of both expected and unexpected effects of designer drugs is needed to address their growing availability and to better inform the public of health and safety risks associated with their use (NIDA, 2015a).
Epidemiology of Emerging Designer Drugs
The appearance of new psychoactive substances (NPS) on the drugs market that are not controlled under international and national drug control laws is not a new phenomenon; many of the substances themselves were first synthesized years ago. The “cat and mouse game,” whereby there is a continuous circumvention of existing legislation as new substances appear, can be traced back to the early years of the twentieth century with international attempts to control esters of morphine.
In recent years, however, there has been an increasing commodification of the market in new substances. This has been fueled by entrepreneurs and increasingly organized crime groups who have exploited a growing manufacturing capacity in countries such as China and India and globalized trade. Here, the Internet has played a key role in both the advertisement and sale, allowing an open market to develop. This is reflected in the rapid rate of appearance of NPS, which in Europe over the past few years has averaged one new substance every 5–6 days.
Brandt, King, & Evans-Brown, 2014
Designer drug use is most prevalent among young adults, primarily males in their mid-to-late twenties, but ranging from teens to adults 40 years of age. Those who use designer drugs tend to be single and have lower levels of education and income compared to the general population (Weaver et al., 2015).
Because it is so prevalent, synthetic cannabis has been studied more thoroughly than other designer drugs. Its use may be higher in select subpopulations, particularly regular cannabis users and college students. Among high school seniors, the annual prevalence of synthetic cannabis consumption was 11% in 2011 and 2012. Annual prevalence rates among high school seniors dropped to 8% in 2013, but remained more prevalent than any illicit drug except cannabis (annual use of cannabis remained unchanged) (Weaver et al., 2015).
A Monitoring the Future survey looked at synthetic cannabis use in a 2011 survey by asking twelfth graders about their use in the prior 12 months. Annual prevalence was 11.4%, making synthetic cannabis the second most widely used class of illicit drug after marijuana among twelfth graders. Despite the DEA’s scheduling of synthetic cannabis as a Schedule I drug in 2011, use among twelfth graders remained unchanged in 2012 at 11.3%, which suggests either that compliance with the new scheduling had been limited or that producers of these products succeeded in continuing to change their chemical formulas to avoid using the ingredients that had been scheduled (Johnston et al., 2015).
In 2012, for the first time, eighth and tenth graders were asked about their use of synthetic cannabis; annual prevalence rates were 4.4% and 8.8%, respectively. Use in all three grades dropped in 2013, with a sharp and significant decline among twelfth graders. The declines continued into 2014 and were significant for both tenth and twelfth graders (Johnston et al., 2015).
All three grades were asked whether they associated great risk with trying synthetic cannabis once or twice. The level of perceived risk for experimental use was quite low (between 24% and 33%) but has been rising somewhat among twelfth graders. Likely the availability of these drugs over the counter has had the effect of communicating to teens that they must be safe, though they are not (Johnston et al., 2015).
Bath salt (synthetic cathinone) use is lower than that of synthetic cannabinoids. Overall use of hallucinogens remains very low in the United States, and the epidemiology of synthetic hallucinogens is not currently captured in national surveys (Weaver et al., 2015).
Data from the National Crime Survey for England and Wales in 2012 shows that 3.3% of adults aged 18 to 24 years had used mephedrone (a novel synthetic cathinone discussed in the next module) within the previous year. On an international level, data from the European Monitoring Centre for Drugs and Drug Addiction’s early warning system currently receives a report relating to a newly identified substance about once every week (Smith & Robert, 2014).
Marketing designer drug products as “legal high” alternatives may contribute to the perception of greater safety or purity compared to traditional illicit drugs, which could promote increased consumption. Risk factors for adolescent experimentation with and problems resulting from designer drug use include parents with substance use disorders (SUDs), poor family relationships, poor discipline, or high family conflict; adolescents involved with foster care or the criminal justice system are also at risk (Weaver et al., 2015).
In response to rising designer drug use and its consequences, a series of state and federal initiatives have been enacted during the past several years prohibiting the manufacture, sale, and possession of many designer compounds. Although designer drug use has persisted despite regulatory efforts, there may be a national trend toward reduced consumption of some designer drugs. Use appears to be growing in some subpopulations—including the U.S. military—perhaps to evade detection by urine drug screening. Designer drug use is especially prevalent among those in the military who abuse other substances. Patients presenting for consequences of designer drug use are frequently using more than a single drug (Weaver et al., 2015).
