HIV, the virus that causes AIDS, was first identified in 1981. For some people, many years may pass between the time of infection and symptoms of illness begin or are identified. Those who have the virus but are not yet sick may have no symptoms and may not know they are infected. If a person suspects he or she has been exposed to HIV, there are medications that can be taken after exposure to reduce the likelihood of post exposure infection (PEP).
Cause of HIV
HIV Virus
The physical structure of HIV is characterized by a protein shell encapsulating the genetic information and enzymes of the virus; a lipid membrane that circles the protein capsule; and glycoproteins that dot the surface of the virus, which aid in processes such as entry into macrophages and T-helper cells of the host. Source: Courtesy of Zygote Media Group, Inc.
HIV attacks the immune system by destroying CD4+ T cells, a type of white blood cell that is vital to fighting off infection. The destruction of these cells can leave people with untreated HIV vulnerable to life-threatening infections and complications (NIAID, 2020, June 19).
The destructive power of HIV comes from its ability to affect the normal functioning of CD4 cells* by replacing CD4 RNA** with HIV RNA. This process manipulates the CD4 cell into duplicating the HIV virus. Once altered, the CD4 cell can no longer flag dangerous pathogens, affecting the body’s ability fight off opportunistic infections (Wilkins, 2020). Over time, a person’s immune system becomes vulnerable to infections by common disease-causing organisms such as bacteria, fungi or viruses.
*CD4 cells: CD4 cells, also known as T cells, are white blood cells that fight infection and play an important role in your immune system.
**RNA: Ribonucleic acid, or RNA is one of the three major biological macromolecules that are essential for all known forms of life (along with DNA and proteins).
Transmission
HIV Entry Into T Cell
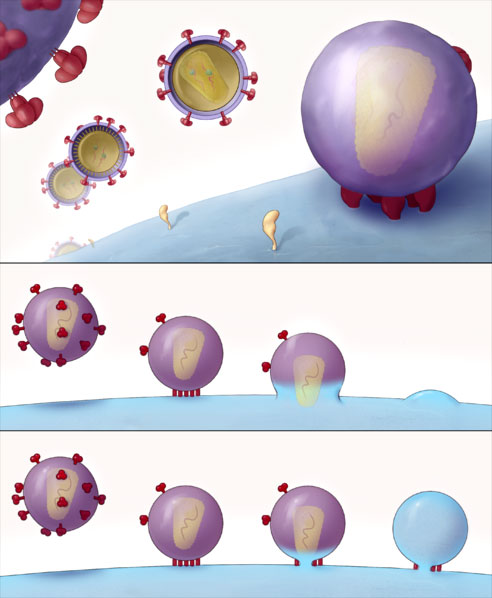
The top panel shows the HIV virus finding and attaching to a T cell. The second and third panels show HIV viruses (dotted with red glycoproteins) attaching to the T cell and depositing the HIV virus particle into the T cell. Source: Sougrat et al., 2007. PLoS Creative Commons Attribution 2.5 license.
HIV is a relatively fragile virus that is not spread by casual contact. For HIV to be transmitted, there must be:
- A source
- A sufficient dose
- Access to the bloodstream of another person
An HIV source is a person (host) who is HIV-positive—a person with sufficient viral load to transmit the virus to another person. One of the predictors of the infectiousness of an HIV-positive person is their viral load—how much HIV is present in the bloodstream. There is a clear connection between higher viral load and increased transmissibility.
HIV can be transmitted through unprotected anal, vaginal, and oral intercourse. It can also be transmitted through accidental needlestick injuries, or by body fluids from an infected person contacting broken skin or mucous membranes of another person. Other routes of transmission:
- An infected person sharing needles or other injection equipment
- A mother passing the virus to her baby either before or during birth
- An infected woman breastfeeding her infant
- A transfusion prior to 1986 of HIV-infected blood or blood products
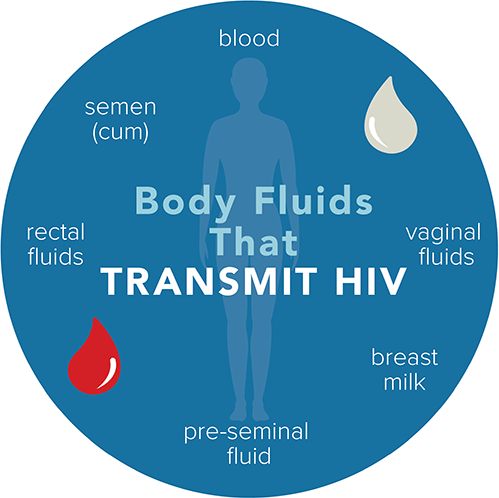
Source: CDC.
In extremely rare cases, HIV can be transmitted by sharing razors or toothbrushes, if infected blood from one person is deposited on the toothbrush or razor and the blood entered the bloodstream of another person.
In settings such as hospital operating rooms, other fluids—cerebrospinal fluid, synovial fluid, pleural fluid, pericardial fluid, amniotic fluid—may be considered potentially infectious if the source is HIV-positive. These fluids are generally not found outside the hospital setting.
HIV transmission can occur during practices such as tattooing, blood-sharing activities such as “blood brother” rituals or any other type of ritualistic ceremonies where blood is exchanged, or when unsterilized equipment contaminated with blood is shared. Up to 40% of new HIV infections are transmitted by people who are unaware they have the virus.
Improvements in public awareness has helped decrease HIV/AIDS cases due to the availability of prompt testing and treatment. Pre-exposure prophylaxis (PrEP) has been shown to be effective in preventing HIV for those at higher risk.
PrEP is highly effective for preventing HIV when taken as prescribed. It reduces the risk of getting HIV from sex by about 99%. It also reduces the risk of getting HIV from injection drug use by at least 74% (CDC, 2021, August 6).
In late 2021, the FDA approved Apretude, an extended-release injectable medication for use in at-risk adults and adolescents weighing at least 77 pounds for pre-exposure prophylaxis to reduce the risk of sexually acquired HIV. Apretude is given first as two injections administered one month apart, and then every two months thereafter. Patients can either start their treatment with Apretude or take oral cabotegravir (Vocabria) for four weeks to assess how well they tolerate the drug (FDA, 2021, December 20).
Transmission During Pregnancy and Breastfeeding
An HIV-infected woman can transmit the virus to her baby during pregnancy, during the birth process, or following pregnancy by breastfeeding. HIV is transmitted from an HIV-infected woman to her baby in about 25% of pregnancies if intervention with antiretroviral medications does not occur.
The perinatal transmission rate has dropped dramatically in the U.S. due to the widespread use of zidovudine (AZT, Retrovir) by HIV-infected pregnant women. When a woman’s health is monitored closely and she receives antiretroviral therapies during pregnancy, the risk of HIV transmission to the newborn drops to a 1 in 1000 chance (HIV.gov, 2021, February 10).
A predictor of how infectious the woman will be to her baby is her viral load. Women with new or recent infections or people in later stages of infection tend to have higher viral loads and may be more infectious.
In some pregnancies, a cesarean section may be recommended to reduce the risk of transmission from mother to baby. Advice should be provided on an individual basis by a medical provider with experience in treating HIV-positive pregnant women. Most states, including Florida, require pregnant women to be counseled regarding risks around HIV and offered voluntary HIV testing.
For a woman with HIV, the risk of transmitting HIV to her baby can be 1% or less if she:
- Takes HIV medicine as prescribed throughout pregnancy, birth, and delivery.
- Gives HIV medicine to her baby for 4 to 6 weeks after giving birth.
- Does not breastfeed or pre-chew her baby’s food.
CDC, 2020, August
When a pregnant woman tests positive for HIV, in addition to medical and support services, she should also be referred to the Healthy Start Care Coordination System. For more information on the availability of services, contact the Family Health Line at 800 451-BABY or the Florida AIDS Hotline at 800 FLA-AIDS.
Untreated HIV
If left untreated, HIV progresses in a predictable pattern: sometimes called the “natural history of disease progression”. Infection begins with entry of the virus into the host’s bloodstream (viral transmission). In 1 to 2 weeks, the virus begins to establish itself in the body and change the functioning of the immune system’s CD4 cells (primary HIV infection).
Seroconversion occurs when antibodies to the HIV virus can be identified by laboratory test. During this asymptomatic phase, an infected person will look and feel healthy, but the virus is active and continues to damage the immune system.
As the disease progresses, symptoms begin to appear, which may include skin rash, night sweats, mouth ulcers, weight loss, and fungal infections. Finally, AIDS develops, which is a CD4+ T-lymphocyte count of <200 cells/μL or CD4+ T-lymphocyte percentage of total lymphocytes of <14, or documentation of an “AIDS-defining condition.”
This “natural progression” has been dramatically altered in developed countries because of new medications. In countries where there is no access to medications because of access or cost, or in cases where people do not become aware of their HIV infection until very late, the disease progresses as described above (Melhuish & Lewthwaite, 2018).
Transmission by People Unaware of Their HIV Status
Globally, many people infected with HIV have not been tested and about 6 million people are unaware that they are living with the virus. About 15% of those in the U.S. are unaware they are infected (~162,000 people), a decline from the 25% in 2003. Awareness of HIV status is critical because most people who know they are infected will reduce behaviors that could transmit the virus (HIV.gov, 2021, June 25).
