Within healthcare facilities, prevention is an important component of any infection control program. Environmental control factors, engineering, and work practice controls, as well as training and education of healthcare workers, are all part of a comprehensive infection prevention program.
Standard Precautions
Standard Precautions are the minimum infection prevention practices that apply to all patient care, regardless of suspected or confirmed infection status of the patient, in any setting where healthcare is delivered. These practices are designed to both protect healthcare workers and prevent them from spreading infections to patients. Standard Precautions include:
- Hand hygiene.
- Use of personal protective equipment (e.g., gloves, masks, eyewear).
- Respiratory hygiene / cough etiquette.
- Sharps safety (engineering and work practice controls).
- Safe injection practices (i.e., aseptic technique for parenteral medications).
- Sterile instruments and devices.
- Clean and disinfected environmental surfaces.
If exposures to blood or other body fluids are reasonably anticipated, facilities are required by the Occupational Safety and Health Administration (OSHA) Bloodborne Pathogens Standard to develop an Exposure Control Plan.
An Exposure Control Plan is designed to protect staff who may be exposed to blood and other body fluids. By protecting staff, facilities also control exposure incident costs. Such a plan is meant to be a “living” document—a source for answering bloodborne pathogen–related questions and an assurance that exposure control activities are in place.
Percutaneous Exposures
Occupational exposure to viruses and other pathogens can occur following percutaneous injury*, mucous membrane exposure (such as eyes, nose and mouth) or non-intact skin exposure to blood and body fluids. Percutaneous injuries carry the greatest risk of infection, accounting for 66–95% of all occupational exposures to bloodborne pathogens (Auta et al., 2018).
*Percutaneous injury: when a needle or other sharp object penetrates the skin.
Globally each year, percutaneous injuries result in approximately 66,000 HBV infections, 16,000 HCV infections and 1,000 HIV infections. More than 90% of these infections occur in developing countries where adherence to standard precautions is poor (Auta et al., 2018).
In the U.S., EPINet publishes annual data that provides a picture of sharp object injury and blood and body fluid exposure patterns in healthcare settings. According to data from 41 participating hospitals, most sharps injuries were among nurses and doctors with more than half occurring during an intramuscular (IM) or subcutaneous injection or during suturing (ISC, 2021).
Nearly half or injuries occurred in the OR/recovery areas. About 2/3 of injuries were to the left hand although over 90% of the injured workers were right-handed. In most cases (90%) the sharp was contaminated (ISC, 2021). Additional exposure findings:
- Was blood visible on device: yes = 69%
- What was the purpose of the device: injection, IM/subcutaneous = 26%; suturing = 28%
- What was the time of injury: during use = 53%
- Did the needle or sharp have a safety design: no = 56%
- Was the safety mechanisms on the needle or sharp activated: no = 67%
ISC, 2021
Needlesticks, Sharps Injuries, and Blood and Body Fluid Exposures
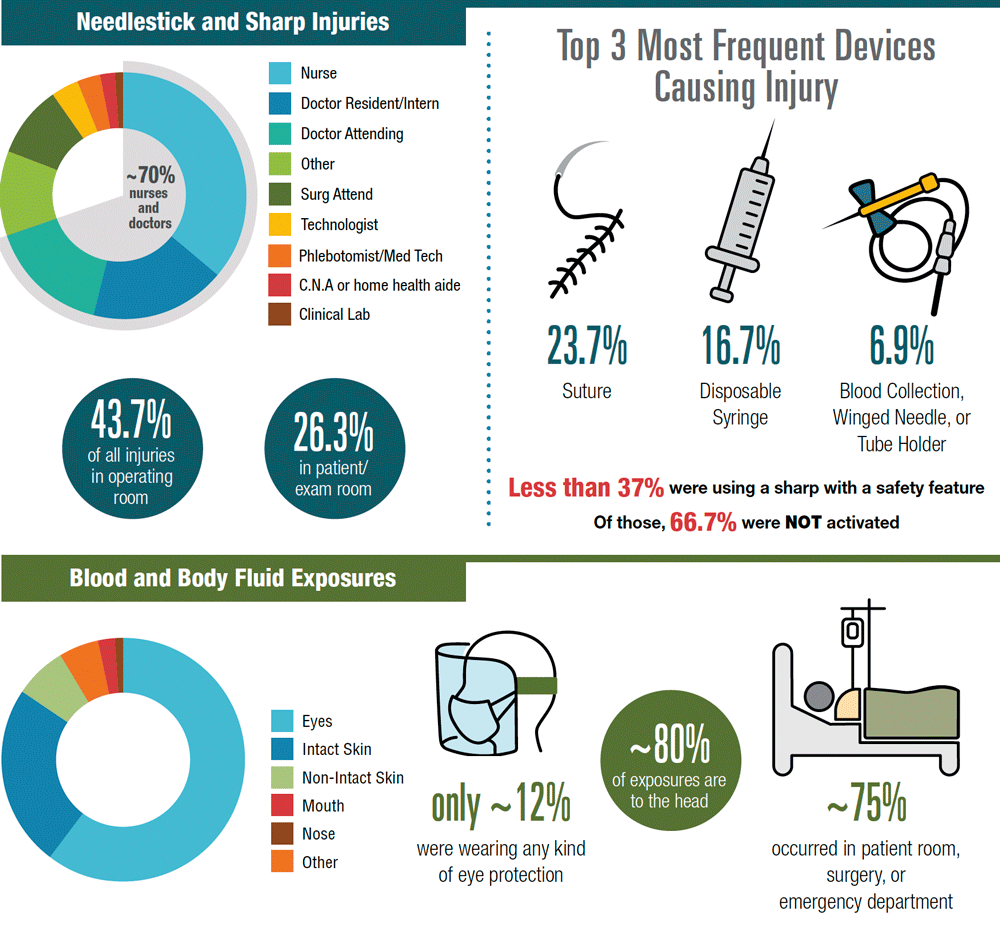
Blood Occupational Exposure Data for Needlesticks, Sharps Injuries, and Blood and Body Fluid Exposures2020 EPINet®. Used with permission.
Because injuries from needles and other sharps have been associated with transmission of hepatitis B, hepatitis C, and HIV, the prevention of sharps injuries is an essential part of Standard Precautions. Needles and other sharp devices should be handled in a manner that prevents injury to the user and to others who may encounter the device during or after routine patient care.
Case Example
An experienced ER nurse recently had a sharps injury to her right hand from a small needle without a safety device. Although she had used this type of needle hundreds of times without incident, in this case she was distracted while talking to a patient. She gave the shot, pulled out the syringe and (usually) immediately disposed of the used sharp in a sharp’s disposal container. While still holding the syringe in her right hand, she stopped to explain to the patient that the medication might cause a flush or redness in the patient’s body. To describe the possible reaction, the nurse swept her hand down the front of her body and stuck herself on her right finger as the syringe turned over in her hand. She washed with soap and water, applied a band aid, and reported the needle stick to her supervisor.
Preventing Occupational Exposures
Hand hygiene is the single most important procedure for preventing the spread of infections, and strict adherence protects both patients and workers. Washing your hands can prevent the spread of germs, including those that are resistant to antibiotics. On average, healthcare workers clean their hands less than half as often as they should.

Source: CDC.
Personal protective equipment should be provided and worn by employees in all instances where they may come into contact with blood or other potentially infectious material. This includes but is not limited to dentistry, phlebotomy, or processing of any bodily fluid specimen, as well as postmortem procedures. Reusable PPE must be cleaned and decontaminated, or laundered, by the employer.
During the COVID-19 pandemic, some infection control standards were relaxed or ignored because PPE was in short supply and many items had to be worn multiple times. To address this, OSHA established the Emergency Temporary Standard for Healthcare for preventing the spread of COVID-19. The standard is aimed at protecting workers facing the highest coronavirus hazards—those working in healthcare settings where suspected or confirmed coronavirus patients are treated. This includes employees in hospitals, nursing homes, and assisted living facilities; emergency responders; home health care workers; and employees in ambulatory care settings where suspected or confirmed coronavirus patients are treated (OSHA, 2021, June 21).
The standard requires facilities to conduct a hazard assessment and have a written plan to mitigate virus spread. It requires healthcare employers to provide some employees with N95 respirators or other personal protective equipment. In addition, covered employers must ensure 6 feet of distance between workers. In situations where this is not possible, employers should erect barriers between employees where feasible (OSHA, 2021, June 21).
The standard also requires covered employers to provide workers with paid time off to get vaccinated and to recover from any side effects. Covered employees who have coronavirus or who may be contagious must work remotely or otherwise be separated from other workers, if possible, or be given paid time off up to $1400 per week (OSHA, 2021, June 21).
