Natural History of HIV Infection
Natural History of HIV Infection
- Viral transmission
- Primary HIV infection
- Seroconversion
- Asymptomatic HIV infection
- Symptomatic HIV infection
- AIDS
The first three constitute the window period.
A person with untreated HIV infection will experience several stages in infection. These include viral transmission, primary HIV infection, seroconversion, asymptomatic HIV infection, symptomatic HIV infection, and AIDS. These stages as sometimes called the “natural history” of disease progression and are described below. The natural history of HIV infection has been altered dramatically in developed countries because of new medications. In countries where there is no access to these expensive medications, or in cases where people do not become aware of their HIV infection until very late, the disease progresses as described below.
Viral Transmission
Viral transmission is the initial infection with HIV. People infected with HIV may become infectious to others within 5 days. They are infectious before the onset of any symptoms, and they will remain infectious for the rest of their lives.
Primary HIV Infection
During the first few weeks of HIV infection, individuals have a very high level of virus (viral load) in their bloodstream. The high viral load means the individual can easily pass the virus to others. Unfortunately, during primary infection many people are unaware that they are infected.
In this stage, about half of infected people have symptoms of fever, swollen glands (in the neck, armpits, groin), rash, fatigue, and a sore throat. These symptoms, which resemble mononucleosis, go away in a few weeks, but the individual continues to be infectious to others.
It is extremely important that healthcare providers consider the diagnosis of primary HIV infection if clients engage in behaviors that put them at risk for HIV and are presenting with the above symptoms. If individuals experience these symptoms after having unprotected sex or sharing needles, they should seek medical care and tell their provider why they are concerned about HIV infection.
Window Period and Seroconversion
The window period begins with initial infection and continues until the virus can be detected by an HIV antibody test. Seroconversion is the term for the point at which HIV antibodies are detectable and the window period ends.
Natural Course of Untreated HIV Infection
The first two weeks following infection are highly contagious but not detectable by HIV tests (see figure below). Antibodies may begin to appear after 2 weeks but take up to 12 weeks or longer to reach seroconversion. As is seen on the line curves, the viral load continues to increase until there are sufficient antibodies to suppress, but not kill, the virus. Once the antibodies become active, an untreated patient may be asymptomatic for 10 years before the antibodies are no longer able to suppress the virus and the person becomes symptomatic.
Natural Course of Untreated HIV Infection
Source: Adapted from Conway & Bartlett, 2003.
Asymptomatic HIV Infection
Following seroconversion, a person infected with HIV is asymptomatic (has no noticeable signs or symptoms). The person may look and feel healthy, but can still pass the virus to others. It is not unusual for an HIV-infected person to live 10 years or longer without any outward physical signs of progression to AIDS. Meanwhile, the person’s blood and other systems are affected by HIV, which would be reflected in laboratory tests. Unless a person in this stage has been tested for HIV, they will probably not be aware they are infected.
Symptomatic HIV Infection
During the symptomatic stage of HIV infection, a person begins to have noticeable physical symptoms that are related to HIV infection. Anyone who has symptoms like these and has engaged in behaviors that transmit HIV should seek medical advice. The only way to know for sure if you are infected with HIV is to take an HIV antibody test.
Although no symptoms are specific only to HIV infection, some common symptoms are:
- Persistent low-grade fever
- Pronounced weight loss that is not due to dieting
- Persistent headaches
- Diarrhea that lasts more than 1 month
- Difficulty recovering from colds and the flu
- Being sicker than they normally would with ordinary illnesses
- Recurrent vaginal yeast infections in women
- Thrush/yeast infection coating the mouth or tongue
Apply Your Knowledge
Q: A client comes into your clinic complaining of a fever of 99 ºF for 3 weeks, weight loss of 15 pounds in the past 2 months, and diarrhea for 6 weeks. He claims he has not changed his regular diet and is not trying to lose weight. He states he has had a lingering cold for weeks and just doesn’t feel good or have energy. What additional history and physical factors would you need to assess?
A: These are classic symptoms of an HIV infection, but could also be a gastrointestinal or respiratory virus. Sexual history, diet history, and family history of GI diseases would need to be assessed. A chest x-ray, CBC, basic metabolic panel, and thyroid levels should be ordered to rule out pneumonia, infections, thyroid health, and inflammatory conditions. It is said as high as 90% of a diagnosis can be determined by a thorough history alone.
AIDS
Did you know . . .
An AIDS diagnosis can only be made by a licensed healthcare provider and, once the diagnosis is made, the person is always considered to have AIDS.
An AIDS diagnosis is based on the result of HIV-specific blood tests and/or on the person’s physical condition. Established AIDS-defining illnesses, white blood cell counts, and other conditions are specifically linked to making an AIDS diagnosis. Once a person is diagnosed with AIDS, even if they later feel better, they do not “go backwards” in the classification system for HIV infection. They are always considered to have AIDS.
People who have an AIDS diagnosis may often appear to a casual observer to be quite healthy, but they continue to be infectious and can pass the virus to others. Over time, people with AIDS frequently have a reduced white blood count and develop poorer health. They may also have a significant amount of virus present in their blood, measureable as viral load.
Cofactors
A cofactor is a separate condition that can change or speed up the course of disease. There are several cofactors that can increase the rate of progression to AIDS. They include a person’s age, certain genetic factors, and possibly drug use, smoking, nutrition, and HCV.
Time from Infection to Death
If the infection is untreated, the average time from HIV infection to death is 10 to 12 years. Early detection and continuing medical treatment have been shown to prolong life for many more years.
AIDS Surveillance Case Definition
[This section was taken from CDC, 2014.]
Following extensive consultation and peer review, the CDC and the Council of State and Territorial Epidemiologists have revised and combined the surveillance case definitions for human immunodeficiency virus (HIV) infection into a single case definition for people of all ages, which includes adults and adolescents aged ≥13 years and children aged <13 years. The revisions were made to address multiple issues, the most important of which was the need to adapt to recent changes in diagnostic criteria.
Laboratory criteria for defining a confirmed case now accommodate new multi-test algorithms, including criteria for differentiating between HIV-1 and HIV-2 infection and for recognizing early HIV infection. A confirmed case can be classified in one of five HIV infection stages: 0, 1, 2, 3, or unknown.
Early infection, recognized by a negative HIV test within 6 months of HIV diagnosis, is classified as stage 0, and acquired immunodeficiency syndrome (AIDS) is classified as stage 3. Criteria for stage 3 have been simplified by eliminating the need to differentiate between definitive and presumptive diagnoses of opportunistic illnesses.
Clinical (non-laboratory) criteria for defining a case for surveillance purposes have been made more practical by eliminating the requirement for information about laboratory tests. The surveillance case definition is intended primarily for monitoring the HIV infection burden and planning for prevention and care on a population level, not as a basis for clinical decisions for individual patients (CDC, 2014).
Since the first cases of AIDS were reported in the United States in 1981, surveillance case definitions for HIV infection and AIDS have undergone several revisions to respond to diagnostic advances. This new document updates the surveillance case definitions originally published in 2008. It addresses multiple issues, the most important of which was the need to adapt to recent changes in diagnostic criteria.
Other needs that prompted the revision included:
- Recognition of early HIV infection
- Differentiation between HIV-1 and HIV-2 infections
- Consolidation of staging systems for adults/adolescents and children
- Simplification of criteria for opportunistic illnesses indicative of AIDS
- Revision of criteria for reporting diagnoses without laboratory evidence (CDC, 2014)
Stage 3–Defining Opportunistic Illnesses in HIV Infection
- Bacterial infections, multiple or recurrent*
- Candidiasis of bronchi, trachea, or lungs
- Candidiasis of esophagus
- Cervical cancer, invasive†
- Coccidioidomycosis, disseminated or extrapulmonary
- Cryptococcosis, extrapulmonary
- Cryptosporidiosis, chronic intestinal (>1 month’s duration)
- Cytomegalovirus disease (other than liver, spleen, or nodes), onset at age >1 month
- Cytomegalovirus retinitis (with loss of vision)
- Encephalopathy attributed to HIV§
- Herpes simplex: chronic ulcers (>1 month’s duration) or bronchitis, pneumonitis, or esophagitis (onset at age >1 month)
- Histoplasmosis, disseminated or extrapulmonary
- Isosporiasis, chronic intestinal (>1 month’s duration)
- Kaposi sarcoma
- Lymphoma, Burkitt (or equivalent term)
- Lymphoma, immunoblastic (or equivalent term)
- Lymphoma, primary, of brain
- Mycobacterium avium complex or Mycobacterium kansasii, disseminated or extrapulmonary
- Mycobacterium tuberculosis of any site, pulmonary†, disseminated, or extrapulmonary
- Mycobacterium, other species or unidentified species, disseminated or extrapulmonary
- Pneumocystis jirovecii (previously known as “Pneumocystis carinii”) pneumonia
- Pneumonia, recurrent†
- Progressive multifocal leukoencephalopathy
- Salmonella septicemia, recurrent
- Toxoplasmosis of brain, onset at age >1 month
- Wasting syndrome attributed to HIV
* Only among children aged <6 years.
† Only among adults, adolescents, and children aged ≥6 years.
Source: CDC, 2016b.
Clinical Manifestations vs. Opportunistic Infections
When their immune system is suppressed, people have weaker defenses against the wide variety of bacteria, viruses, fungi, and other pathogens that are present almost everywhere. A clinical manifestation is the physical result of some type of illness or infection.
The opportunistic infections associated with HIV include any of the infections that are part of an AIDS-defining classification. For example, the opportunistic infection cytomegalovirus often causes the clinical manifestation of blindness in people with AIDS.
HIV in the Body
Scientists are always learning new information about how HIV affects the body. HIV infection seems to affect many body systems. It is well known that HIV infection causes a gradual, pronounced decline in the immune system’s functioning. People with HIV are at risk for a wide variety of illnesses, both common and exotic.
HIV affects the:
- Kind and number of blood cells
- Amount of fat and muscle distribution in the body
- Structure and functioning of the brain
- Normal functioning of the immune system
- Body’s basic metabolism
HIV infection can cause many painful or uncomfortable conditions, including:
- Confusion or dementia
- Diarrhea
- Fatigue
- Fever
- Nausea or vomiting
- Painful joints, muscles, or nerve pain
- Difficulty with breathing
- Urinary or fecal incontinence
- Vision or hearing loss
- Thrush (yeast infections in the mouth)
- Chronic pneumonias, sinusitis, or bronchitis
- Loss of muscle tissue and body weight
Test Your Knowledge
Opportunistic diseases and infections:
- Are seen only during the window period of HIV infection.
- Affect the kind and number of blood cells in HIV-infected patients.
- Are caused by a suppressed immune system that weakens defenses against bacteria, viruses, and fungi.
- Are the physical result of some type of illness or infection.
Answer: C
HIV in Children
Children show significant differences in their HIV disease progression and their virologic and immunologic responses when compared to adults. Without drug treatment, children may have developmental delay, failure to thrive, recurrent bacterial infections such as P. carinii pneumonia, and other conditions related to low immune response. The antiretroviral treatments that are available for HIV infection may not be available in pediatric formulations. The medications may have different side effects in children than they do in adults.
It is vital that women know their HIV status before and during pregnancy. Antiretroviral treatment significantly reduces the chance that their child will become infected with HIV. Prior to the development of antiretroviral therapies, most HIV-infected children were very sick by 7 years of age.
In 1994 scientists discovered that a short treatment course of the medication AZT for pregnant women dramatically reduced the number and rate of children who became infected perinatally. Cesarean sections for delivery may be warranted in certain cases to reduce HIV transmission. As a result, perinatal HIV infections have substantially declined in the developed world.
Early diagnosis of HIV infection in newborns is now possible. Antiretroviral therapy for infants is now the standard of care, and should be started as soon as the child is determined by testing to be HIV-infected. Apparently uninfected children who are born to HIV-positive mothers are currently treated with antiretroviral medicines for 6 weeks to reduce any possibility of HIV transmission.
Did you know. . .
Women with HIV who take antiretroviral medication during pregnancy as recommended can reduce the risk of transmitting HIV to their babies to less than 1%.
Test Your Knowledge
HIV infection in children:
- Has the same disease progression as adults.
- Has been reduced by using AZT in HIV-infected pregnant women.
- Does not usually cause symptoms until puberty.
- Causes developmental delay when treated with drugs too early.
Answer: B
HIV in Women
Certain strains of HIV may infect women more easily. The strain of HIV present in Thailand seems to transmit more easily to women through sexual intercourse. Scientists believe that women and receptive partners are more easily infected with HIV than insertive partners. Receptive partners are at greater risk for transmission of any sexually transmitted disease, including HIV.
Women infected with HIV are at increased risk for a number of gynecologic problems, including pelvic inflammatory disease (PID), abscesses of the fallopian tubes and ovaries, and recurrent yeast infections.
Some studies have found that HIV-infected women have a higher prevalence of infection with the human papilloma virus (HPV). Cervical dysplasia is a precancerous condition of the cervix caused by certain strains of HPV. Cervical dysplasia in HIV-infected women often becomes more aggressive as the woman’s immune system declines. This may lead to invasive cervical carcinoma, which is an AIDS-indicator condition. It is important for women with HIV to have more frequent Pap tests than those who are not infected.
Several studies have shown that women in the United States who have HIV receive fewer healthcare services and HIV medications than men. This may be because women aren’t diagnosed or tested as frequently.
Access to Medical Care
As the medications that are available to treat HIV infection have become more numerous and complex, HIV care has become a medical specialty. If possible, people who have HIV infection should seek out a physician who is skilled in the treatment of HIV and AIDS.
People in Washington State may gain access to an HIV specialist through the assistance of the case manager(s) in their county. Call your local health department or health district for information on case management programs.
Impact of New Drugs on Clinical Progression
Before 1996 there were three medications available to treat HIV. These drugs were used singly and were of limited benefit. Researchers in 1996 discovered that taking combinations of these and newer medications dramatically reduced the amount of HIV (viral load) in the bloodstream of a person infected with HIV. Two or three different medications are used in combination. Each one targets a separate part of the virus and its replication. The reduction of deaths from AIDS in the United States has been primarily attributed to this combination therapy, called highly active antiretroviral therapy (HAART).
Not everyone with HIV infection benefits from the new drug therapies. Some people cannot tolerate the unpleasant or serious side effects from the medications. Others cannot adhere to the complex treatment schedule. If patients do not take their medication every day according to their physician’s instructions, the drugs do not work effectively and viral resistance may develop.
Cost of new drug therapies can be prohibitive. Insurance programs and government programs for individuals with low income pay for much of the cost of the HIV medicines in many states. These medicines may cost upwards of $2,000 per person each month. People who live in other countries where the medication is unaffordable have very limited access to the newer therapies.
Although the new drug therapies work for many people to keep the amount of virus in their bodies to very low levels, they are not a cure for HIV. Once therapy is discontinued, viral load will increase. Even during treatment, viral replication occurs and the person remains infectious to others.
It is now common to see combination drug therapy referred to simply as ART, or antiretroviral therapy. New drugs and new guidelines for their usage are not uncommon and information about them can be accessed on the CDC and National Institutes of Health (NIH) AIDSinfo websites.
Test Your Knowledge
HAART therapy:
- Is a newly discovered antiretroviral drug.
- Is a cure for HIV/AIDS.
- Decreases viral load to a point where patients are no longer contagious.
- Is the primary reason for the reduction of deaths from AIDS in the United States.
Answer: D
Resistance
Many people find that over time the virus becomes resistant to their medication and they must change medications. This is especially true when the medications are not taken correctly, but it limits the number of possible drug therapies the person might be able to use.
Side Effects
Patients often have unpleasant side effects when they use prescription medications to treat their HIV infection. These side effects include:
- Nausea
- Diarrhea
- Peripheral neuropathy (numbness or pain in feet and hands)
- Lipodystrophy: changes in body fat distribution, which presents with large fat deposits on the back of the neck, on the stomach area and in breast size in women and with pronounced thinning of the arms and legs
- Interference with the metabolism of oral contraceptives
- Osteoporosis
- Diabetes or other changes in glucose metabolism
- Very high cholesterol or triglycerides
- Damage to the nervous system, liver, and/or other body organs
Alternative Therapies
People have relied on alternative (sometimes called complementary) therapies to treat HIV infection for as long as HIV has been known. Many people use these treatments along with therapies from their medical provider. Other people choose to use only alternative therapies. These therapies comprise a wide range of treatments, including vitamins, massage, herbs, naturopathic remedies, and many more. While there is no evidence of harm from these treatments, there is also very little evidence of benefit. Many of these remedies still have not been studied to see if they help.
It is important for people who are taking alternative therapies to tell their medical provider what they are using. There may be harmful side effects from the interactions of the “natural” medicine and antiretrovirals. For example, St. John’s Wort is an herbal remedy often used for depression that interacts negatively with HIV medications.
Other drugs, including over-the-counter (OTC) medications, prescription medications, and street drugs, may have serious interactions with antiretroviral medications. It is extremely important that people on HIV medications tell their doctor, pharmacist, and social worker about all other drugs they take.
Case Management
People living with HIV often seek the assistance of an HIV case manager who can help explain the different types of services available. Most states have systems in place to provide prescription and medical assistance to people living with HIV and AIDS. Contact your local health department or district to find case management in your community.
You can also call the Washington State Department of Health Client Services toll-free at 877 376 9316. Children with HIV may also benefit from the Children with Special Health Care Needs program. Care coordinators for this program are located at every county health department or district. Local community-based organizations like the Northwest Family Center in Seattle, and specialty hospitals like Children’s Medical Center in Seattle and Mary Bridge Children’s Hospital in Tacoma, may provide additional support to children and families.
Prevention Strategies
Anthony Fauci, director of the National Institute on Allergy and Infectious Diseases (NIAID), has stated, “Prevention is not unidimensional with HIV, it is a multidimensional, heterogeneous combination of preventions” (NIAID, 2014a).
Fauci accompanied the statement above with a graphic entitled “Combination HIV Prevention” that included:
- HIV Testing/Counseling
- Treatment as Prevention
- Medical Male Circumcision
- STI Treatment
- Microbicides
- Treatment/Prevention of Drug/Alcohol Abuse
- Clean Syringes
- Education/Behavior Modification
- Condoms
- Blood Supply Screening
- ARVs for PMTCT, PEP, PrEP [Antiretroviral therapies for Prevention of Mother to Child Transmission, Post Exposure Prophylaxis, Pre Exposure Prophylaxis] (Fauci, 2014)
No one prevention option works all the time with every target group, but each one has shown, and continues to show, frequent measurable success with many groups. Used together, they have made significant headway against HIV (Fauci, 2014; NIAID, 2014a).
HIV Prevention for Adults and Adolescents with HIV
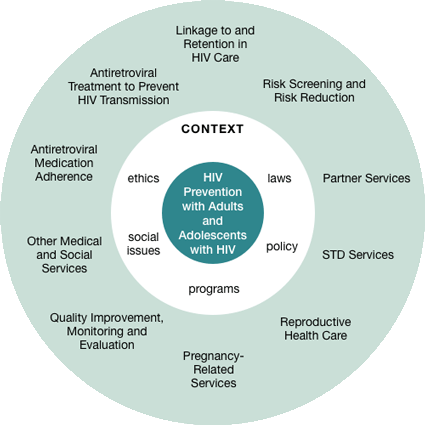
Source: CDC.
Treatment as Prevention
The advent in 1996 of potent combination antiretroviral therapy (ART), sometimes called HAART (highly active antiretroviral therapy) or cART (effective combination antiretroviral therapy), changed the course of the HIV epidemic. These “cocktails” of three or more antiretroviral drugs used in combination gave patients and scientists new hope for fighting the epidemic, and have significantly improved life expectancy—to decades rather than months.
For many years, scientists believed that treating HIV-infected people also significantly reduced their risk of transmitting the infection to sexual and drug-using partners who did not have the virus. The circumstantial evidence was substantial, but no one had conducted a randomized clinical trial—the gold standard for proving an intervention works.
That changed in 2011 with the publication of findings from the HIV Prevention Trials Network (HPTN) 052 study, a randomized clinical trial designed in part to evaluate whether the early initiation of ART can prevent the sexual transmission of HIV among heterosexual couples in which one partner is HIV-infected and the other is not. This landmark study validated that early HIV treatment has a profound prevention benefit; results showed that the risk of transmitting HIV to an uninfected partner was reduced by 96% (HPTN, 2016).
As a concept and a strategy, treating HIV-infected people to improve their health and to reduce the risk of onward transmission—sometimes called treatment as prevention—refers to the personal and public health benefits of using ART to continuously suppress HIV viral load in the blood and genital fluids, which decreases the risk of transmitting the virus to others. The practice has been used since the mid-1990s to prevent mother-to-child, or perinatal, transmission of the virus.
Research published in 1994 showed that zidovudine, more commonly known as AZT, when given to HIV-infected pregnant women and to their newborns reduced the risk of perinatal transmission from about 25% to 8%. Since then, routinely testing pregnant women and treating infected mothers with ART during pregnancy, delivery, and while breastfeeding, when practiced according to recommendations, has reduced the mother’s risk of transmitting HIV to her child by 90%.
Treatment alone won’t solve the global HIV epidemic, but it is an important element of a multi-pronged attack that includes prevention efforts, wise investment of resources, greater access to screening and medical care, and involvement by everyone—local, state, and federal government; faith-based communities; and private groups and individuals. Providing treatment for people who are living with HIV infection must be the first priority and, in order to get treatment, one must be aware of the need. Thus testing and identification of those with HIV infection become the “pivotal entry point into the medical care system for both treatment and prevention” (CDC, 2013).
Vaccine
Work on an HIV vaccine can be traced back three decades to before the first HIV vaccine clinical trial at the National Institutes of Health in 1987, yet one researcher has said recently that he believes the vaccine he is working on is still 8 to 10 years away from proving workable in humans. Discouraging as that may sound, it takes a great deal of time to do the work needed to create a vaccine, and HIV provides some unique challenges (NIAID, 2013; Hayes, 2017; AIDS.gov, 2015).
Vaccines historically have been the most effective means to prevent and even eradicate infectious diseases. Like smallpox and polio vaccines, a preventive HIV vaccine could save millions of lives. Developing safe, effective, and affordable vaccines that can prevent HIV infection in uninfected people is the best hope for controlling and/or ending the HIV epidemic.
The long-term goal is to develop a safe and effective vaccine that protects people worldwide from getting infected with HIV. However, even if a vaccine only protects some people, it could still have a major impact on the rates of transmission and help control the epidemic, particularly for populations where there is a high rate of HIV transmission. A partially effective vaccine could decrease the number of people who get infected with HIV, further reducing the number of people who can pass the virus on to others.
HIV is a very complex, highly changeable virus, and it is different from other viruses because the human immune system never fully gets rid of it. Most people who are infected with a virus, even a deadly one, recover from the infection, and their immune systems clear the virus from their bodies. Once cleared, an immunity to the virus often develops. But humans do not seem to be able to fully clear HIV and develop immunity to it. The body cannot make effective antibodies and HIV actually targets, invades, and then destroys important cells that the human body needs to fight disease. So far, no person with an established HIV infection has cleared the virus naturally, and this has made it more difficult to develop a preventive HIV vaccine.
Scientists continue to develop and test vaccines in labs, in animals, and even in human subjects. Trials allow researchers to test the efficacy and safety of their vaccine candidate, and each trial has yielded important information on the path to developing a widely effective vaccine, but there are still many challenges to be overcome.
Pre-Exposure Prophylaxis (PrEP)
Pre-exposure prophylaxis (PrEP) is a way for people who do not have HIV to help prevent HIV infection by taking a pill every day. The pill contains two medications that are also used, in combination with others, to treat HIV. When someone is exposed to HIV through sex or injection drug use, PrEP can help stop the virus from establishing a permanent infection (CDC, 2014c).
Currently, the only pill approved by the FDA for use as PrEP for people at very high risk of getting HIV infection is called Truvada, and it contains tenofovir and emtricitabine. These drugs work by blocking important pathways that HIV uses to set up an infection (AIDS.gov, 2014a).
When used consistently, PrEP has been shown to greatly reduce the risk of HIV infection in people who are at substantial risk. In all of the several national and international clinical trials, the risk of getting HIV infection was lower—up to 92% lower—for participants who took the medications consistently than for those who did not. PrEP is much less effective when it is not taken consistently (CDC, 2014c).
PrEP is a powerful HIV prevention tool, and can be combined with condoms and other prevention methods to provide even greater protection than when used alone. People who use PrEP must commit to taking the drug daily and seeing their healthcare provider every 3 months for HIV testing and other followup (CDC, 2014c).
PrEP is not for everyone, and in 2014 the U.S. Public Health Service released the first comprehensive clinical practice guidelines for PrEP, Pre-exposure Prophylaxis for the Prevention of HIV Infection in the United States, 2014: A Clinical Practice Guideline, accompanied by a supplement with forms and counseling guidance.
In 2014 the CDC, in collaboration with others, launched the nation’s first PrEPline, which enables clinicians (physicians, nurse practitioners, and physician assistants) to call toll-free to consult with experts about using pre-exposure prophylaxis (PrEP) with a patient. PrEP will also provide written and online checklists, guidelines, informational material, and educational tools (CDC, 2014c).
Tuberculosis, Other STDs, and Hepatitis B and C
Because of the interrelationships between HIV, tuberculosis (TB), sexually transmitted diseases, HBV, and HCV, a brief discussion of each requires review by health care professionals.
Tuberculosis and HIV
Mycobacterium tuberculosis (TB) is transmitted by airborne droplets from people with active pulmonary or laryngeal TB during coughing, sneezing, or talking. Although TB bacteria can live anywhere in the body, infectious pulmonary or laryngeal TB poses the greatest threat to public health.
Cause of TB
Latent infection, which is asymptomatic and not infectious, can last for a lifetime. A presumptive diagnosis of active TB is made when there are positive test results or acid-fast bacilli (AFB) in sputum or other bodily fluids. The diagnosis is confirmed by identification of M. tuberculosis on culture, which should be followed by drug sensitivity testing of the bacteria.
Epidemiology of TB
Tuberculosis is one of the world’s deadliest diseases. One-third of the world’s population is infected with TB. Thirteen million Americans, an estimated 4.2%, became sick with TB disease and there were approximately 1.5 million TB-related deaths. The CDC estimated that 6% to 10% of all TB cases in America occurred among people who were HIV positive (CDC, 2016).
In 2013, 9,582 TB cases were reported in the United States. This number and the case rate of 3.0 cases/100,000, both decreased over 2012 and are in line with a continuing decrease since the 1992 TB resurgence peak (CDC, 2014e).
In its Communicable Disease Report 2013, the Washington State Department of Health notes that there are approximately 200 to 250 new cases of TB each year and the number of deaths range from 2 to 18 (1980–2012) (WDOH, 2014).
In 2013 (latest figures available) there were 209 cases of TB reported in Washington State, while that number was 185 in 2012. In 2013 only 6 of 39 counties had 5 or more cases. These six counties represent 85.6% of the reported cases, and over one-half (54.5%) were in King County (WDOH, 2014, 2014a).
The incidence rate in Washington State for 2013 rose to 3.0% from 2.7% in 2012, equaling the 2013 national rate, which itself saw a decline from 3.2% the previous year (WA DOH, 2014, 2014a).
Transmission and Progression
When infectious secretions sneezed or coughed by an adult with pulmonary TB are breathed in by another person, the bacteria may come to rest in the lungs. After several weeks the bacteria multiply, and some asymptomatic, pneumonia-like symptoms may occur. The TB bacteria are carried through the bloodstream and lymph system, pumped through the heart, and then disseminated through the body.
The largest amount of bacteria goes to the lungs. In most cases, this process, called primary infection, resolves by itself and something called delayed-type hypersensitivity is established. This is measured with the tuberculin skin test. The incubation period for this primary infection is 2 to 10 weeks. In most cases, a latent state of TB develops. Ninety percent of people with latent TB (LTBI) never experience subsequent disease. Other than a positive tuberculin skin test, people with latent TB infection have no clinical, radiographic (x-ray), or laboratory evidence of TB and cannot transmit TB to others.
Among the other 10% of infected individuals, the TB infection undergoes reactivation at some time and they develop active TB. About 5% of newly infected people reactivate within the first 2 years of primary infection and another 5% will do so at some point later in life.
Symptoms of TB
The period from initial exposure to conversion of the tuberculin skin test is 4 to 12 weeks. During this period, the patient shows no symptoms. The progression to active disease and symptoms (such as cough, weight loss, and fever) usually occurs within the first 2 years after infection, but may occur at any time.
Prevention of TB
It is important to recognize the behavioral barriers to TB management, which include deficiencies in treatment regimens, poor client adherence to TB medications, and lack of public awareness. Primary healthcare providers need adequate training in screening, diagnosis, treatment, counseling, and contact tracing for TB through continuing education programs and expert consultation.
Promoting patient adherence to the sometimes-complicated medication schedule also requires consideration of patients’ cultural and ethnic perceptions of their health condition. Providing strategies and services that address the multiple health problems associated with TB (such as alcohol and drug abuse, homelessness, and mental illness) also builds trust and promotes adherence to treatment plans.
A daily regimen of Isoniazid for 9 months is recommended because prospective, randomized trials in HIV-negative people indicate that 12 months of treatment is more effective than 6 months of treatment. Although a 9-month regimen of Isoniazid is the preferred regimen for the treatment of LTBI, a 6-month regimen does provide substantial protection.
In some situations, treatment for 6 months rather than 9 months may be cost-effective and still provide a favorable outcome. Thus, based on local conditions, health departments or providers may conclude that a 6-month rather than a 9-month course of Isoniazid is preferred.
Clinical trials have shown that daily preventive therapy for 12 months reduces the risk for TB disease by more than 90% in patients with LTBI who complete a full course of therapy. There is evidence that 6 months of preventive therapy with Isoniazid may also prevent disease in approximately 69% of patients who complete the regimen. Every effort should be made to ensure that patients adhere to this therapy for at least 6 months. Children should receive at least 9 months of preventive therapy.
Treatment of TB and Multidrug-Resistant TB
In order to prevent drug resistance and cure TB, the CDC recommends that TB be treated with a multidrug regimen that may last 6 to 12 months.
Current recommendations can be found in the Washington State Department of Health’s TB Services Manual, updated in 2012, which outlines how public health staff complete TB control tasks in Washington State and is available from the department online.
TB/HIV Co-Infection
People co-infected with HIV/TB are at considerably greater risk of developing TB disease than those with TB alone. Studies suggest that the risk of developing TB disease is 7% to 10% each year for people who are infected with both M. tuberculosis and HIV, whereas it is 10% over a lifetime for a person infected only with M. tuberculosis.
In an HIV-infected person, TB disease can develop in either of two ways. A person who already has latent TB infection can become infected with HIV, and then TB disease can develop as the immune system is weakened. Or, a person who has HIV infection can become infected with M. tuberculosis, and TB disease can then rapidly develop because the immune system is not functioning well.
Any HIV-infected person with a diagnosis of TB disease should be reported as having TB and AIDS. For more information on TB, contact the:
- Communicable disease staff in each county health department/district
- Washington State Department of Health TB program, 1-800-525-0127
Other STDs and HIV
The term STD (sexually transmitted disease) refers to more than twenty-five infectious organisms transmitted through sexual activity and dozens of clinical syndromes that they cause. Sexually transmitted diseases affect men and women and can be transmitted from mothers to babies during pregnancy and childbirth. They are also called sexually transmitted infections (STIs).
Bacterial, Viral, and Other Causes of STD
Bacteria cause STDs including chlamydia, gonorrhea, and syphilis. Viruses cause herpes, genital warts, hepatitis B, and HIV. Scabies are caused by mites, and pubic lice cause “crabs.” Trichomoniasis is caused by tiny organisms called protozoa and “yeast” infections are caused by fungi. Some STDs, such as pelvic inflammatory disease, can have more than one cause, for example, a woman may have both gonorrhea and chlamydia, causing PID. A man may have more than one cause for epididymitis, usually gonorrhea and chlamydia. Non-gonococcal urethritis (NGU) is usually caused by bacteria.
STD, Nationally and Internationally
Since the beginning of the AIDS epidemic, researchers have noted the strong association between HIV and other STDs. The CDC estimates that there are 20 million new STD infections every year, including gonorrhea, chlamydia, and syphilis—the three that physicians are required to report. Half of these new STD infections occur in young people aged 15 to 24 and accrue almost $16 billion in healthcare costs.
Since 2015 saw increases in the three reportable STDs and 1.5 million new cases of chlamydia was the highest of any condition ever reported to the CDC. Gay and bisexual men face the highest, and continually rising, number of syphilis cases, representing 90% of all cases. Syphilis infection increases the rate of HIV infection (CDC, 2016).
Globally, more than 1 million people acquire a sexually transmitted infection (STI) every day. The term STI is often used to reflect the fact that a person may be infected yet show no symptoms of disease. Each year 500 million become ill with chlamydia, gonorrhea, syphilis, and trichomoniasis. Drug resistance, especially for gonorrhea, presents a major challenge to fighting these diseases worldwide (WHO, 2013).
Primary STD infections may cause pregnancy-related complications, congenital infections, infertility, ectopic pregnancy, chronic pelvic pain, and cancers. STDs can also accelerate other infections like HIV.
HIV and STDs
The presence of infection with other STDs increases the risk of HIV transmission because:
- STDs like syphilis and symptomatic herpes can cause breaks in the skin, which provide direct entry for HIV.
- Inflammation from STDs such as chlamydia makes it easier for HIV to enter and infect the body.
- HIV is often detected in the pus or other discharge from genital ulcers from HIV-infected men and women.
- Sores can bleed easily and come into contact with vaginal, cervical, oral, urethral, and rectal tissues during sex.
- Inflammation appears to increase HIV viral shedding and the viral load in genital secretions.
STD Transmission
STDs are transmitted in the same way that HIV is transmitted: by anal, vaginal, and oral sex. In addition, skin-to-skin contact is important for the transmission of herpes, genital warts, and HPV infection, syphilis, scabies, and pubic lice.
Symptoms of STD
In the past there was a great emphasis on symptoms as indicators of STD infection. Research has changed this. We now know that 80% of those with chlamydia, 70% of those with herpes, and a great percentage of those with other STDs have no symptoms but can still spread the infections.
Along with prompt testing and treatment for those who do have symptoms, the emphasis in the United States is on screening for infection based on behavioral risk. Patients cannot assume that their healthcare providers do STD testing. In other words, women who are getting a Pap test or yearly exam should not just assume that they are also being tested for chlamydia or any other STD.
Prevention of STD
The following steps will help prevent STD infection:
- Abstain or be in a mutually monogamous relationship with an uninfected partner.
- Know that many STDs have no symptoms.
- Know that birth control pills and shots do not prevent infections—you must use condoms along with other birth control methods.
- Go with your sex partner(s) for tests.
- Avoid douching.
- Learn the right way to use condoms and then use them correctly and consistently every time you have sex.
- Be sure all sex partners are examined and treated if an STD occurs.
- Change the ways you have sex so that there is no risk of infection.
- Learn how to talk about correct use of condoms with all sex partners.
- Practice the prevention you have learned for HIV and hepatitis.
STD Tests
At most sites, new urine tests (urinate in a cup) are available for some STDs. The Western Blot (blood) test for herpes and hybrid capture tests for genital warts may also be available. In most places, however, cultures, wet preps, and blood draws for syphilis remain the standard testing method. It is vital that women get Pap tests, and that both men and women disclose a history of STD during medical workups.
STD Treatment
Treatment for STDs is based on lab work and clinical diagnosis. Treatments vary with each disease or syndrome. Because there is developing resistance to medications for some STDs, check the latest CDC treatment guidelines.
Hepatitis B and HIV
Hepatitis is inflammation of the liver that may be caused by many things, including viruses. Current viruses include hepatitis A (fecal/oral transmission), B, C, D, and others. Hepatitis B (HBV) is a virus that is transmitted by the blood and body fluids of an infected person. There are approximately 10% of people with HIV co-infected with HBV. Transmission of HBV occurs in the same behaviors as becoming infected with HIV, namely unprotected sex and through blood transmission of sharing needles.
Prevention of HBV
A vaccine to prevent HBV is available. Hepatitis B vaccine is administered intramuscularly as a three-dose series over 6 months. More than 90% of people who take the three injections become immune to HBV. Why isn’t everyone vaccinated for HBV? The HBV vaccine is relatively inexpensive for infants and children but more expensive for adults (costing about $150 per person). This cost is the likely reason that most adults are not vaccinated against HBV.
HBV Epidemiology
Each year tens of thousands of people become infected with HBV in the United States. Of these, about 2% to 6% of adults will become chronically infectious carriers of the virus. There are up to 1.4 million carriers of HBV in the United States.
HBV is not transmitted by:
- Breastfeeding
- Sneezing
- Hugging
- Coughing
- Sharing eating utensils or drinking glasses
- Food or water
- Casual contact
Risk Factors for HBV Infection
Unvaccinated people are at higher risk for getting HBV if they:
- Share injection needles/syringes and equipment
- Have sexual intercourse with an infected person or with more than one partner
- Are a man and have sex with a man
- Work where they come in contact with blood or body fluids, such as in a healthcare setting, prison, or home for the developmentally disabled
- Use the personal care items (razors, toothbrushes) of an infected person
- Are on kidney dialysis
- Were born in a part of the world with a high rate of hepatitis B (China, Southeast Asia, Africa, the Pacific Islands, the Middle East, South America, and Alaska)
- Receive a tattoo or body piercing with equipment contaminated with the blood of someone infected with HBV
Progression of HBV
The average incubation period for HBV is about 12 weeks. People are infectious when they are “hepatitis B surface-antigen positive” (HBsAg), either because they are newly infected or because they are chronic carriers.
HBV causes damage to the liver and other body systems, which can range in severity from mild, to severe, to fatal. Most people recover from their HBV infection and do not become carriers. Carriers (about 2%–6% of adults who become infected) have the virus in their body for months, years, or for life. They can infect others with HBV through their blood or other body fluid contact.
Symptoms of HBV
People with HBV may feel fine and look healthy. Some people who are infected with HBV display only mild symptoms, which could include:
- Loss of appetite
- Extreme fatigue
- Abdominal pain
- Jaundice (yellowing of the eyes and skin)
- Joint pain
- Malaise
- Dark urine
- Nausea or vomiting
- Skin rashes
Others who are infected with HBV experience more severe symptoms, and may be incapacitated for weeks or months. Long-term complications may also occur, and include chronic hepatitis, recurring liver disease, liver failure, and cirrhosis (chronic liver damage).
Prevention of HBV
A vaccine for HBV has been available since 1982. This vaccine is suitable for people of all ages, even infants. People who may be at risk for infection should get vaccinated. To further reduce the risk of or prevent HBV infection, a person can:
- Abstain from sexual intercourse and/or injecting drug use
- Maintain a monogamous relationship with a partner who is uninfected or vaccinated against HBV
- Use safer sex practices (as defined in the Transmission section)
- Never share needles/syringes or other injection equipment
- Never share toothbrushes, razors, nose clippers, or other personal care items that may come in contact with blood
- Use Standard Precautions with all blood and body fluids
Infants born to mothers who are HBV carriers have a greater than 90% reduction in their chance of becoming infected with HBV, if they receive a shot of hepatitis B immune globulin and hepatitis B vaccine shortly after birth, plus two additional vaccine doses by age 6 months. It is vital that the women and their medical providers are aware that the woman is an HBV carrier. People with HBV should not donate blood, semen, or body organs.
Treatment of HBV
There are no medications available for recently acquired (acute) HBV infection. There are antiviral drugs available for the treatment of chronic HBV infection, however treatment success varies by individual. The vaccine is not used to treat HBV once a person is infected.
Hepatitis C and HIV
Hepatitis C is a liver disease caused by the hepatitis C virus (HCV), which is found in the blood of people who have this disease. Hepatitis C is the leading cause of chronic liver disease in the United States. Hepatitis C was discovered in the late 1980s, although it was likely spread for at least 40 to 50 years prior to that.
HCV Epidemiology
Globally, 180 million people are infected with HCV. An estimated 4.1 million Americans have been infected with HCV and about 3.2 million are chronically infected (meaning they have a current or previous infection with the virus). The CDC estimates that as many as 1 million Americans were infected with HCV from blood transfusions, and that 3.75 million Americans do not know they are HCV-positive. Of these, 2.75 million people are chronically infected and are infectious for HCV.
In the United States, 8,000 to 10,000 deaths per year are attributed to HCV-associated liver disease. The number of deaths from HCV is expected to triple in the next 10 to 20 years.
An estimated 110,000 people in Washington State are infected with HCV.
Transmission of HCV
HCV is transmitted primarily by blood and blood products. Blood transfusions before 1992 and the use of shared or unsterilized needles and syringes have been the main causes of the spread of HCV in the United States. The primary way that HCV is transmitted now is through injecting drug use. Since 1992 all blood for donation in the United States is tested for HCV.
Sexual transmission of HCV is considered low, but it accounts for 10% to 20% of infections. If a pregnant woman is infected with HCV, she may pass the virus to her baby but this occurs in only about 5% of those pregnancies. Household transmission is possible if people share personal care items such as razors, nail clippers, or toothbrushes.
HCV is not transmitted by:
- Breastfeeding (unless blood is present)
- Sneezing
- Hugging
- Kissing
- Coughing
- Sharing eating utensils or drinking glasses
- Food or water
- Casual contact
Progression of HCV
The severity of HCV differs from HIV. The CDC states that, for every hundred people who are infected with HCV:
- About 15% will fully recover and have no liver damage
- 85% may develop long-term chronic infection
- 70% may develop chronic liver disease
- 20% may develop cirrhosis over a period of 20–30 years
- 1%–5% may die from chronic liver disease
Symptoms of HCV
People with HCV may have few or no symptoms for decades. When present, the symptoms of HCV are:
- Nausea and vomiting
- Weakness
- Fever
- Muscle and joint pain
- Jaundice (yellowing of the eyes and skin)
- Dark-colored urine
- Tenderness in the upper abdomen
Prevention of HCV
There is no vaccine to prevent HCV infection. People with HCV should not donate blood, semen, or body organs.
The following steps can protect against HCV infection:
- Follow Standard Precautions to avoid contact with blood or accidental needlesticks.
- Refrain from acquiring tattoos or skin piercings outside of a legitimate business that practices Universal Precautions.
- Refrain from any type of injecting drug use or drug equipment sharing.
- Never share toothbrushes, razors, nail clippers, or other personal care items.
- Cover cuts or sores on the skin.
- People who are HCV-infected may lower the small risk of passing HCV to their sex partner by using latex condoms and practicing safer sex.
- Women who are HCV-infected and wish to have children should discuss their choices beforehand with a medical specialist.
Treatment of HCV
Currently there are approved antiretroviral treatments for HCV. The cost of the treatments can be high, and the side effects can be significant (fatigue, flu-like symptoms, nausea, depression, and anemia). People infected with HCV should abstain from alcohol use to avoid further damage to the liver.
Testing for HCV
Many people who are infected with HCV are unaware of their status. People who should consider testing are:
- Current or former injecting drug users
- People who received blood transfusions or an organ transplant prior to 1992
- Hemophiliacs who received clotting factor concentrates produced before 1987
- People who received chronic hemodialysis
- Infants born to infected mothers
- Healthcare workers who have been occupationally exposed to blood or who have had accidental needlesticks
- People who are sex partners of people with HCV
Testing for HCV is available through physicians and some health departments. In 1999 the Food and Drug Administration approved the first home test for HCV. The test kit, called Hepatitis C Check, is available from the Home Access Health Company. The test is accurate if it has been at least 6 months since the possible exposure to HCV.
Comparison Chart of HIV, HBV, and HCV | |||
|---|---|---|---|
Transmission by | HIV | HBV | HCV |
Blood | Yes | Yes | Yes |
Semen | Yes | Yes | Rarely (more likely if blood present) |
Vaginal fluid | Yes | Yes | Rarely (more likely if blood present) |
Breast milk | Yes | No (but may be transmitted if blood is present) | No (but may be transmitted if blood is present) |
Saliva | No | No | No |
Target in the body | Immune System | Liver | Liver |
Risk of infection after needlestick exposure to infected blood | 0.5% | 1–31% | 2–3% |
Vaccine available? | No | Yes | No |
For more information on Hepatitis B or C, go to the CDC hepatitis website or call the Hepatitis Hotline at 888 443 7232 (888 4HEPCDC). | |||
