*This course has been retired. There is no replacement course at this time. Please click here to view the current ATrain course listings.
Seasonal influenza differs from pandemic influenza in that it occurs each year, typically during a specific time of the year. Seasonal flu generally causes less illness because the population has some immunity left over from previous, similar influenza strains. In the Northern Hemisphere, winter is the time for seasonal influenza, but the exact timing and duration of influenza seasons vary. While influenza outbreaks can happen as early as October, activity usually peaks in January or later.
The United States 2017–2018 influenza season was a high-severity season with high levels of outpatient clinic and ED visits for influenza-like illness, high influenza-related hospitalization rates, and elevated and geographically widespread influenza activity across the country for an extended period (Garten et al., 2018).
The “peak month of flu activity” is the month with the highest percentage of respiratory specimens testing positive for influenza virus infection during that influenza season. During this 36-year period, flu activity most often peaked in February (15 seasons), followed by December (7 seasons), March (6 seasons), and January (6 seasons) (CDC, 2018b).
Influenza activity in the United States during the 2018–2019 season (September 30, 2018–May 18, 2019) was considered to be of moderate severity. Nationally, influenza-like illness (ILI) activity began increasing in November 2018, peaked during mid-February 2019, and returned to below baseline in mid-April; the season lasted 21 weeks, making it the longest season in 10 years (Xu et al., 2019).
Influenza A viruses predominated, with very little influenza B activity. Two waves of influenza A were notable during this extended season: influenza A(H1N1) viruses from October 2018 to mid-February 2019 and influenza A(H3N2) viruses from February through May 2019 (see below charts). The number of influenza B viruses reported was low compared with previous seasons, accounting for only 4% of influenza viruses. Compared with the 2017–2018 influenza season, rates of hospitalization last season were lower for adults, but were similar for children (Xu et al., 2019).
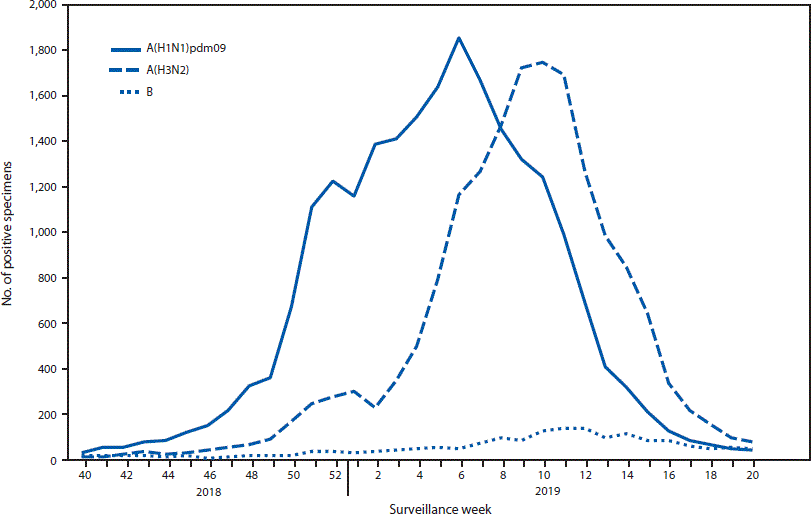
Chart shows two waves of flu activity for 2018–2019. Source: CDC.
https://www.cdc.gov/mmwr/volumes/68/wr/mm6824a3.htm?s_cid=mm6824a3_w
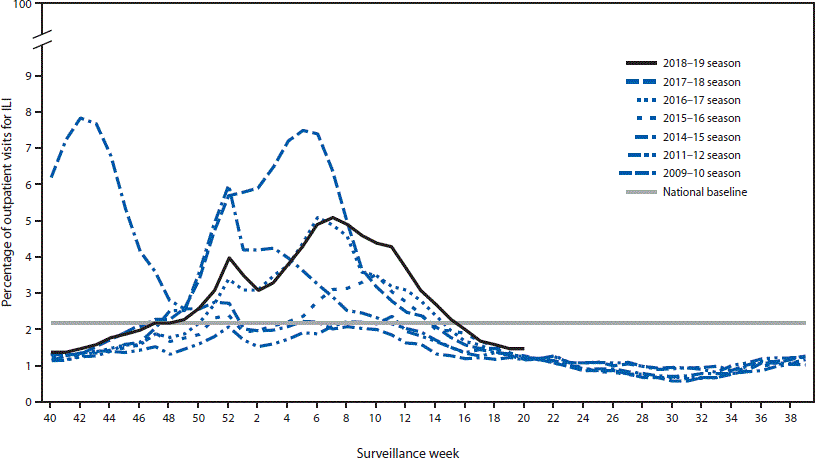
Chart shows flu activity for several recent years. Source: CDC.
https://www.cdc.gov/mmwr/volumes/68/wr/mm6824a3.htm?s_cid=mm6824a3_w
Seasonal Influenza Clinical Features
[Material from this section from CDC 2019, CDC 2015, PB].
Influenza is a contagious respiratory illness caused by influenza viruses. It can cause mild to severe illness resulting in hospitalization or even death. “Classic” influenza is characterized by the abrupt onset of fever, myalgia, sore throat, nonproductive cough, and headache. The fever is usually 101°F to 102°F and accompanied by prostration (bedridden) (CDC, 2019, 2015PB).
The onset of fever is often so abrupt that the exact hour is recalled by the patient. Myalgias mainly affect the back muscles. Cough is believed to be a result of tracheal epithelial destruction. Additional symptoms may include runny nose, headache, substernal chest burning, and ocular symptoms such as eye pain and sensitivity to light (CDC, 2019, 2015PB).
The incubation period for influenza is usually 2 days, but can vary from 1 to 4 days. The severity of illness depends on whether the immune system has been exposed to related virus variants. Somewhat surprisingly, only about 50% of infected people will develop the classic clinical symptoms of influenza (CDC, 2019, 2015PB).
Systemic symptoms and fever usually last from 2 to 3 days, rarely more than 5 days. They may be decreased by such medications as aspirin* or acetaminophen. Recovery is usually rapid, but some patients may have lingering depression and lack of strength or energy for several weeks (CDC, 2019, 2015PB).
*Aspirin should NOT be used for infants, children, or teenagers because they may be at risk for contracting Reye syndrome following an influenza infection.
Symptoms of the Flu
People who have the flu often feel some or all of these symptoms:
- Fever* or feeling feverish, chills
- Cough
- Sore throat
- Runny or stuffy nose
- Muscle or body aches
- Headaches
- Fatigue
- Vomiting and diarrhea—more common in children than adults
* Not everyone with flu will have a fever.
Complications
[Material from this section from CDC 2019, CDC 2015, PB].
The most frequent complication associated with influenza is pneumonia, especially secondary bacterial pneumonia (eg, Streptococcus pneumoniae, Haemophilus influenzae, or Staphylococcus aureus). Primary influenza viral pneumonia is an uncommon complication but has a high fatality rate. Reye syndrome is a complication that occurs almost exclusively in children taking aspirin, primarily in association with influenza B (or varicella zoster), and presents with severe vomiting and confusion, which may progress to coma due to swelling of the brain (CDC, 2019, 2015PB).
Other complications can include myocarditis and worsening of chronic bronchitis and other chronic pulmonary diseases. People with congestive heart failure may have a worsening of the condition triggered by the flu. Death is reported in less than 1 per 1,000 cases. The majority of deaths occur among individuals 65 years of age and older (CDC, 2019, 2015PB).
If vaccine supply is limited, vaccination efforts should focus on:
- Children 6 months to 4 years
- Adults 50 years and older
- Women who are or will be pregnant during influenza season
- Residents of nursing homes and other chronic-care facilities
- Those who are morbidly obese (body-mass index is 40 or greater)
- Healthcare personnel
- American Indians and Alaskan Natives
- People with chronic pulmonary (including asthma), cardiovascular (except hypertension), renal, hepatic, neurologic, hematologic, or metabolic disorders (including diabetes mellitus)
- People who have a weakened immune system or those that are immunosuppressed (including immunosuppression caused by medications or HIV)
- Children 6 months through 18 years of age and receiving long-term aspirin therapy and who therefore might be at risk for experiencing Reye syndrome after influenza virus infection
- Household contacts and caregivers of children younger than 5 years of age and adults 50 years of age or older, with particular emphasis on vaccinating contacts of children aged younger than 6 months
- Household contacts and caregivers of people with medical conditions that put them at higher risk for severe complications from influenza (CDC, 2019, 2015PB)
Transmission
Influenza is primarily a community-based infection that is transmitted in households and community settings. In humans, influenza is primarily transmitted from person to person via large virus-laden droplets (particles more than 5 microns in diameter) that are generated when infected individuals cough or sneeze. These large droplets can then settle on the mucosal surfaces of the upper respiratory tracts of susceptible people who are nearby (within 3 feet).
Cone-Shaped Dispersion of Sneeze Particles

This photograph captures a sneeze in progress, revealing the plume of salivary droplets as they are expelled in a large cone-shaped array from this man’s open mouth, thereby dramatically illustrating the reason for covering your mouth when coughing or sneezing, in order to protect others from germ exposure. Source: James Gathany, CDC PHIL, 2009.
Transmission can also occur through direct or indirect contact with respiratory secretions, such as when touching surfaces contaminated with influenza virus and then touching the eyes, nose, or mouth. Adults can transmit influenza from the day before symptom onset to approximately 5 days after symptoms begin. Children can transmit influenza to others for 10 or more days.
Healthy adults may be able to infect others beginning 1 day before symptoms develop and up to 5 to 7 days after becoming sick. Some people, especially young children and people with weakened immune systems, might be able to infect others for an even longer time.
A German study yielded information about how and when influenza spreads within a group of people. In the study involving 180 participants, evidence of pre-symptomatic shedding of the influenza virus was observed in 30% of samples 1 day prior to the onset of symptoms. Shedding of virus was greatest on days 1 to 3 of illness (Suess et al., 2012).
Other findings included:
- Quantity of virus shed appeared to be the same for asymptomatic and symptomatic infected subjects
- Those infected with influenza B exhibited the highest viral shedding load
- Antiviral therapy induced a milder clinical course and faster illness resolution but had no effect on viral shedding
- Vaccinated and unvaccinated patients did not differ in terms of clinical course and shedding
- Viable viral shedding, as measured by viral culture, did not persist as long as PCR positivity (Suess et al., 2012)
Watch this fascinating 3-minute video showing how influenza is transmitted and replicated.
Flu Attack! How A Virus Invades Your Body (3:39)
https://www.youtube.com/watch?v=Rpj0emEGShQ
