To remedy the impact of implicit bias, consider social determinants that can be changed and improved, such as opportunities for quality education, good paying jobs, access to quality clinical care, healthy foods, green spaces, and secure and affordable housing. Education and training on implicit bias should be offered to all members of the community, including law enforcement, educators, and healthcare professionals. This can help healthcare providers understand the impact of bias on marginalized groups.
Diversifying hiring practices and actively seeking out and recruiting candidates from underrepresented groups creates a more inclusive and equitable workplace. Supporting community organizations that promote equality and inclusion, provide job training, education, and other services to marginalized groups can help remedy the impact of bias.
Policies that encourage individuals to report incidents of bias or discrimination are important. Once an incident has been reported, healthcare organizations must provide support and resources to address and remedy the situation. Holding individuals and organizations accountable for actions that perpetuate bias or discrimination can go a long way to remedy the impact of implicit bias.
Diversity, Equity, and Inclusion (DEI) Initiatives
Educating the healthcare workforce is one of the first and most common approaches to fostering cultural competence and reducing bias in the workplace (Guerrier, 2022). The extent to which training is effective in reducing bias depends on the duration and frequency of the training, the level of interaction and engagement of participants, and the design and delivery of the training program.
Diversity, equity, and inclusion (DEI) initiatives are provided in most healthcare organizations in the United States. These programs promote an appreciation and respect for differences and similarities in the workplace, including encouraging respect for the perspectives, approaches, and competencies of coworkers and clients. Inclusion helps people feel valued for their unique qualities while promoting collaboration within a diverse group.
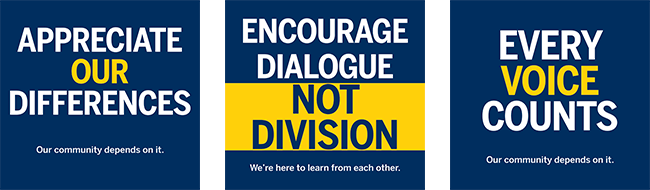
Source: University of Michigan, used with permission.
National Research Programs
The National Institutes of Health is working to reduce bias in healthcare by addressing the lack of diversity that has plagued healthcare research in the past. The program, called All of Us, is enrolling a large group of people that reflect the diversity of the United States. This includes people who haven’t taken part in--or have been left out of--health research before.
All of Us welcomes participants of all backgrounds and walks of life, from all regions of the country, whether they are healthy or sick. The program is a national effort to accelerate health research by exploring the relationship between lifestyle, environment, and genetics (Mapes et al., 2020). All of Us hopes to improve what is called precision medicine by building a diverse database that can inform thousands of studies on a variety of health conditions. The goal is to create more opportunities to:
- Base care on the individual.
- Consider a person’s environment, lifestyle, family health history and genetic makeup.
- Give providers the information they need to make customized recommendations for people of different backgrounds, ages, and regions.
- Provide information about how to be healthier.
- Reduce healthcare costs by matching the right person with the right treatment the first time.
NIH, 2021, July 16
Another program from the National Institutes of Health is the UNITE Initiative, which is working to identify and address structural racism within the scientific community. UNITE aims to establish an equitable and civil culture within the biomedical research enterprise and reduce barriers to racial equity in the biomedical research workforce. To reach this goal, UNITE identifies opportunities, makes recommendations, and develops and implements strategies to increase inclusivity and diversity in science. (NIH, 2022, March 2).
Health Literacy Programs
Health literacy programs help people obtain, process, and understand basic health information and services needed to make appropriate health decisions. Research by the Institute of Medicine (IOM) indicated that over 90 million people residing in the U.S. have difficulty understanding and acting on health information (NCCC, Nd).
The view of health literacy as solely the responsibility of a patient has expanded to include healthcare professionals and healthcare systems. To improve health literacy, healthcare organizations must remove systemic barriers when communicating health information to patients and the community and understand the broader socio-cultural contexts in which health literacy is experienced (NCCC, Nd).
Implying that an individual or community is responsible for increased risk of adverse outcomes is counterproductive. Some members of disproportionately affected groups may be unable to follow health recommendations due to inequitable resource allocation or a lack of inclusive infrastructure (CDC, 2021, August 24).
Sustaining the Gains
Bias training is most effective when it is designed with context and professional identity in mind. Training in teams helps individuals feel comfortable sharing their biases and accepting their vulnerabilities. Training that enhances collaboration and openness reinforces behavioral change (Sukhera, 2020).
Sustaining the effects of bias education and training requires visible support of organizational leaders. Rather than focusing exclusively on training others, leaders must consider their own approaches to equity and diversity. Leaders who model a more inclusive approach and integrate bias training with other initiatives are more successful than those who rely on training alone (Sukhera, 2020).

Source: CDC.
Case: Katherine and Her Mother in Spain
My mother came to visit me when I studied abroad in Spain. One rainy day while we were sightseeing, she slipped on some marble steps and fell to the ground, hitting her head. She was in pain and seemed disoriented, so I decided we should go to the hospital.
While we were waiting to be seen by the doctor, I was so scared. I had asked the women at the front desk if there was anyone who spoke English, but they said no. Even though I had been studying in Spain for several months, I hadn’t learned anything about medical issues and felt uncomfortable speaking in Spanish with the staff. As I waited for her name to be called, I kept looking up medical terms in Spanish on my phone and writing them down in case I needed them. I was afraid my mother had a concussion from hitting her head during the fall. Knowing that any errors I made in Spanish could possibly affect the doctor’s decisions really upset me.
During the consultation, I was the mediator between my mother and anyone who came into the examination room. I could tell my mother was frustrated and worried by her inability to communicate with anyone, and I was afraid that I wasn’t using the correct terms to describe what happened to her with the medical staff.
The doctor mentioned something about medical tests and medications she would prescribe, and so we’re waiting in the intake room again with all the other patients. How can I be sure they correctly understand what happened? I’m not sure what’s going to happen next. My mother is so important to me. I just want to be sure she is healthy and that there were no complications.
Think About It
- How would you feel if this happened to you?
- Do you think someone could have a similar experience when seeking care at your organization? If so, who would that person be?
- What would happen if someone with language assistance needs entered your organization today?
- Would their story sound like Katherine and her mother’s? (HHS, 2022)
