The loss of any individual to suicide cannot typically be explained by individual factors alone. A web of biological, psychological, social, environmental, and situational concerns influence suicidal ideation and behaviors. Childhood trauma, substance abuse, poverty, and untreated mental health problems are common risk factors. Unfortunately, many people cannot get help because of provider shortages, stigma, and the cost of care.
Preventing suicide requires culture change, access to care, research, and community engagement. It also requires ongoing coordination with all sectors, institutions, and stakeholders. Because suicide is a national tragedy that affects all of us, to be successful, everyone must be engaged (HHS, 2021, January 19).
1.1 In the United States

Source: CDC, 2024, April 24.
U.S. suicide rates are not limited to any gender, age, socioeconomic, or ethnic group. Among children, teenagers, and young adults, suicide is the second leading cause of death, while among middle-aged adults, suicide is the fifth leading cause of death (NCHS, 2022, March 3). In 2022, more than 49,000 Americans died from suicide, making it the eleventh leading cause of death overall. Remarkably, in 2021 there were twice as many suicides in the United States as homicides (NCHS, 2024, July 23).
Since the National Strategy for Suicide Prevention was updated in 2024, prevention efforts have expanded and multiplied, increasing our understanding of suicide prevention practices in healthcare systems and communities. New partners have become engaged, including organizations and businesses that had not previously viewed suicide prevention as part of their mission.
Although funding still may not reflect the impact of suicide in the U.S., more resources are being dedicated than ever before. For example, the President’s Roadmap to Empower Veterans and End a National Tragedy of Suicide (PREVENTS) was launched in 2019. In July of 2022 the Federal Communications Commission designated 988 as the national number for mental health crises (HHS, 2021, January 19).
Source: CDC, 2024, April 24.
During the COVID pandemic, there was a record increase in the homicide rate and a spike in the number of drug overdose deaths. It was thought that the number and rate of suicides would follow that pattern—particularly after suicides had risen every year between 2004 and 2019. However, between 2018 and 2019, there was a minor decline in suicide, which continued into the pandemic year of 2020 (CDC, 2021, November 5).
Suicide Rates in the United States (by state; per 100,000; 2020)
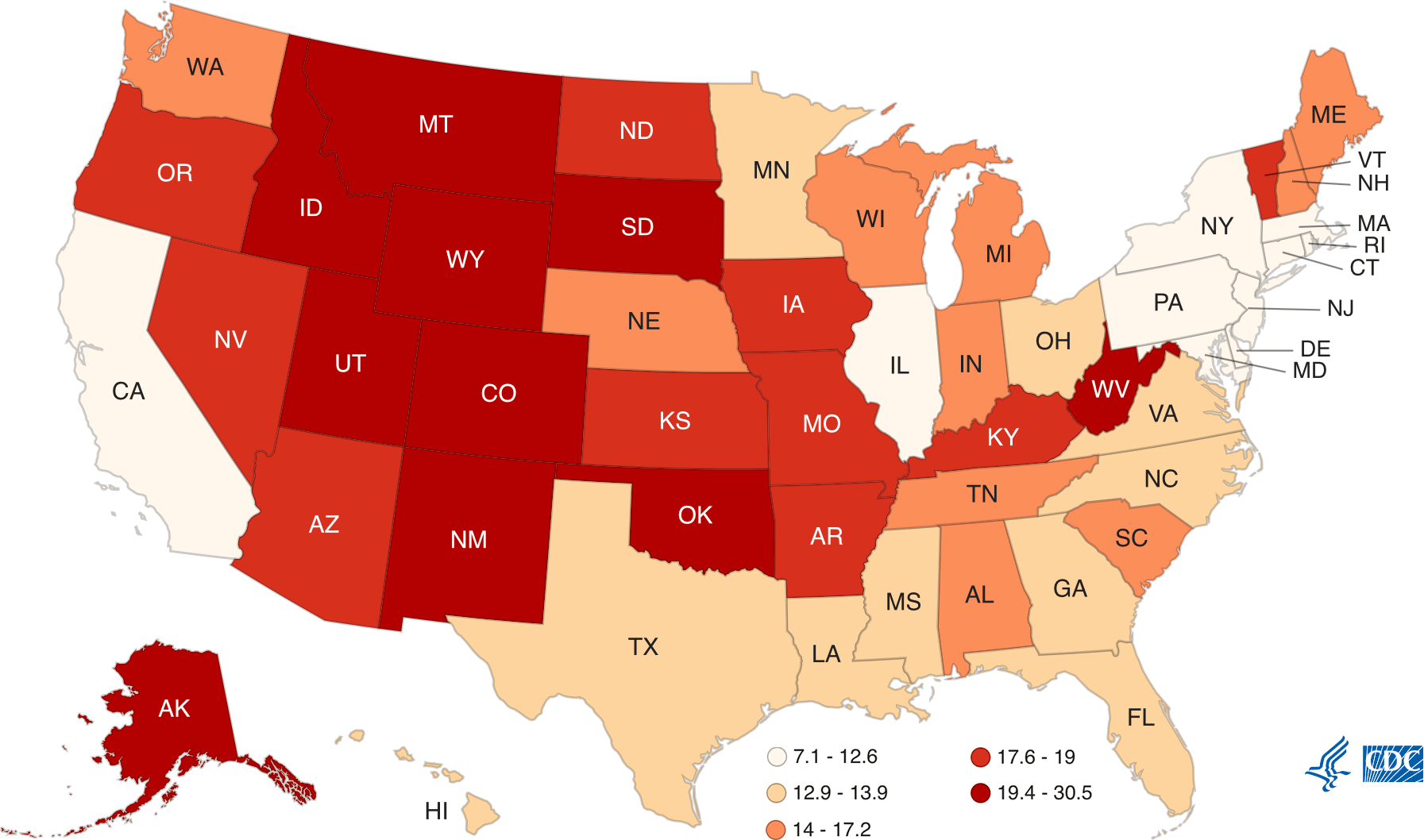
Suicide rates vary from state to state. Washington State, as well as other Western states (excluding California), have some of the highest rates of suicide in the country. Source: CDC.
Definitions
Suicide is defined as death caused by self-directed injurious behavior with intent to die.
A suicide attempt is when someone harms themself with any intent to end their life but does not die as a result.
Suicidal ideation refers to thinking about, considering, or planning suicide.
1.2 In Washington State
Washington State has a coordinated approach to suicide prevention, with multiple partners and state agencies utilizing guidance from the Action Alliance for Suicide Prevention (AASP). Formed in 2016, AASP is now the coordinated body that informs policy and programmatic change and makes recommendations for the Washington State Suicide Prevention Plan (WSDOH, 2021).
Even before the pandemic, Washington’s rate of deaths by suicide was about 14% higher than the national rate (WSDOH, 2021). It has been higher than the national average for more than 10 years. During the last decade, over 11,000 people died as a result of suicide, most commonly by firearms (48%), followed by suffocation and poisoning (deGrauw, 2021).
In Washington State (2018 suicide data, latest available):
- 75% were male
- 65% happened at home
- 41% had a history of suicidal thoughts
- 35% left a suicide note
- 19% served in the military (WSDOH, 2020, November)
Washington State Suicide Deaths by Means, 2017
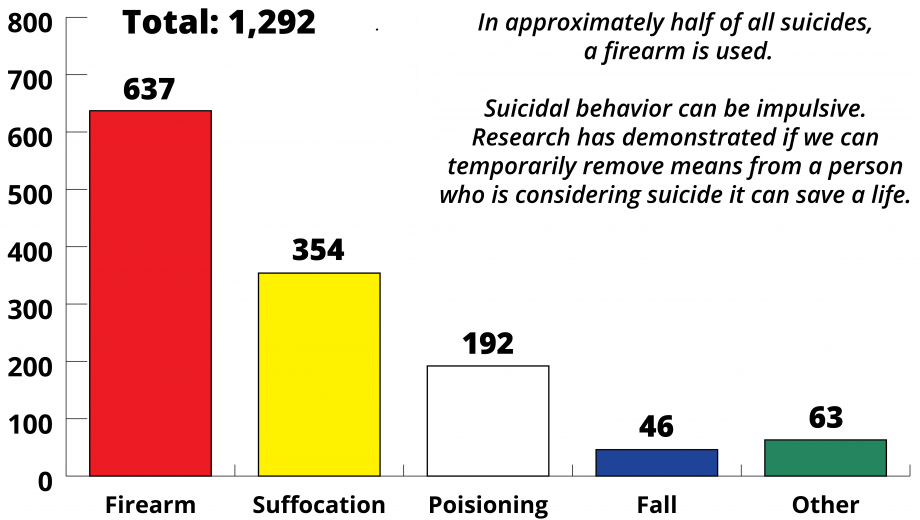
Source: WA Department of Health, 2017: Washington State suicide deaths by means.
Suicide rates vary in different parts of Washington. From 2013 to 2017, suicide rates were higher than the state rate in six counties:
- Clallam
- Grays Harbor
- Okanogan,
- Pierce
- Skamania
- Stevens (WSDOH, 2016)
Seven counties in Washington have small populations and had too few suicides to calculate a suicide rate. This does not mean that there are no suicides in these counties; county-level data do not always accurately reflect suicide losses in communities. For example, in 2013 both the Spokane Tribe of Indians and the Colville Confederated Tribes declared a suicide state of emergency because of high numbers of suicide deaths (WSDOH, 2016).
In Washington and nationally, suicide rates are higher outside urban areas and highest in small-town rural areas. The suicide rate in King County is lower than the state rate, but it has the largest population and the highest number of suicides in the state (WSDOH, 2016).
Additional resources are needed to meet increasing workloads that have grown beyond current funded capacity. The state needs to invest in the AASP’s recommendations for a system with services in suicide prevention, intervention, treatment, and postvention (resources provided in the aftermath of suicide) to support individuals and families and prevent future deaths by suicide (WSDOH, 2021).
Key Points about Suicide
- Suicide is a preventable public health problem, not a personal weakness or family failure.
- People in Washington have a role in suicide prevention—it is not the responsibility of the health system alone.
- People generally avoid discussing suicide.
- Suicide prevention involves changing risk factors, such as childhood trauma, isolation, access to lethal means, and lack of access to appropriate behavioral healthcare.
- Suicide does not affect all communities equally or in the same way.
- People experiencing mental illness, substance use disorders, trauma, loss, and suicidal thinking and behaviors deserve dignity, respect, and the right to make decisions about their care.
Source: Washington State Department of Health, 2016.
