Cannabis seems unique in its wide array of indications for use. The newly discovered endocannabinoid system not only adds to our understanding of human physiology but also helps us understand how and why cannabis is safe and effective for so many indications. This section reviews the safety profile of cannabis and discusses its potential risks. Then it outlines the therapeutic effects and indications for use and presents information about dosage and administration. Cannabis seems to work synergistically with opioids, and most patients with chronic pain significantly reduce or eliminate their use of opioids; thus, cannabis can be viewed as an opiate-sparing medication (Abrams, 2010; Nielsen et al., 2017). Finally, the section ends with some case examples of patients using medicinal cannabis.
Safety Profile
In its natural form, marijuana is one of the safest substances known to man. . . . It would be unreasonable, arbitrary, and capricious for the DEA to continue to stand between those sufferers and the benefits of this substance in light of the evidence in this record.
Francis Young, 1988
DEA Administrative Law Judge
That statement was made after reviewing more than 5000 pages of evidence during the hearings to reschedule marijuana in 1988. Note that he drew these conclusions in 1988, even before researchers discovered the endocannabinoid system.
By trial and error over centuries of use, humans have learned how to use many herbal plants as medication. With more modern research, physicians have moved from using botanicals to specific chemicals within those plants or synthetic versions of those chemicals. In research studies it is much easier to focus on a particular chemical; however, although these specific chemicals may have stronger and more direct effects, they can come with stronger and sometimes-toxic side effects.
Today clinicians are taught to rely on the scientific method, and double-blind placebo-controlled studies are the gold standard. To safeguard the public, the FDA allows new drugs on the market only after they have met basic safety studies and have been shown to have therapeutic value in clinical trials. This research takes years to come to fruition and, even then, some drugs have been allowed on the market and found to have dangerous side effects or adverse reactions when consumed by a larger population.
This course is about the medicinal use of a plant called cannabis. What’s so different about cannabis?
Cannabis is an ancient drug that has been used by countless individuals over the centuries. It is not a new drug. As noted earlier, cannabis was a very popular medication in early American history. Included on numerous bottles of medicinal cannabis would be the claim that it was “guaranteed under the Pure Food and Drugs Act of June 30, 1906” (see below). This was the forerunner of our FDA process today. Many of our early medications (eg, aspirin) had been found to be safe for medical use based on their historical record, and so they were grandfathered in to the list of FDA-approved drugs. Had it not been for the politically driven reefer-madness campaign of the 1930s, cannabis would have also been grandfathered in as an approved medication based on its safety record and efficacy.
Package Label from Eli Lilly, 1913
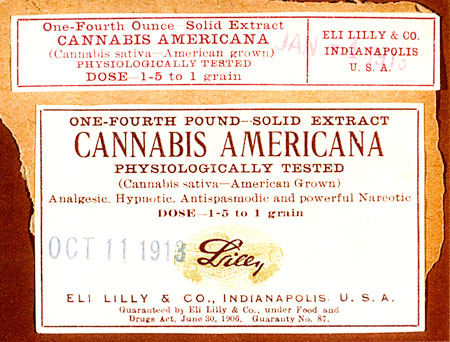
Note that this preparation was “guaranteed” under the Food and Drugs Act of 1906. Source: Courtesy of Patients Out of Time. Used by permission.
Throughout centuries of use there has never been a recorded human death as a result of cannabis consumption. It has a remarkably wide margin of safety. The median lethal dose or LD-50 (dose at which 50% of rats using a drug will die from overdose) of oral THC was 800 to 1900 mg/kg for rats, depending on sex and strain. No cases of death due to toxicity followed a maximum THC dose in dogs (up to 3000 mg/kg) and monkeys (up to 9000 mg/kg) (Grotenhermen, 2007). Stated another way, humans would have to consume 1500 pounds in 15 minutes to induce death. In other words, it is nearly impossible to overdose on this herbal plant. Compare that record to the fact that approximately 120 persons die each year from the use of aspirin or that high doses of acetaminophen can lead to liver damage and death.
Thousands of studies have been funded by the National Institute on Drug Abuse (NIDA) to determine the harmful effects of marijuana. In fact, for many years, researchers could not get federal funding or approval for a study through NIDA if the purpose is to determine its safety or efficacy as a medication (Holland, 2010). Numerous claims have been made, such as marijuana causes cancer, it destroys the immune system, it’s the gateway drug that leads to heroin, it kills brain cells, during pregnancy it will result in fetal abnormalities, and on and on.
Upon taking a closer look, many of these studies have been exposed for their flawed methodology, or the dosage was dramatically increased in an attempt to create a negative outcome. For example, there were early claims of marijuana use causing brain damage based on a study of monkeys that were exposed to cannabis smoke. However, it was discovered that the monkeys were forced to breathe only cannabis smoke for a period of time, and the damage was more likely caused by asphyxiation than cannabis smoke. No subsequent study showed such damage. Another early published study on THC and the immune system managed to show negative results but the dosage used on the rats were extremely high (Zimmer & Morgan, 1997).
In 1974, at Virginia Commonwealth University, research was conducted on rats under the theory that cannabis was carcinogenic. Rather than causing cancer, it was discovered that cannabis was effective in killing the lung-cancer cells. The funding was discontinued and the study was never published in the literature (Munson et al., 1975; Cushing, 2001). Early studies by pulmonologist Donald Tashkin of UCLA found that one cannabis cigarette had the same amount of carcinogenic material in its smoke as four tobacco cigarettes (Wu et al., 1988). The federal government held fast to this claim, but neglected to keep up with Tashkin’s work. Admittedly surprised, Tashkin completed a longitudinal study on thousands of subjects and found no pulmonary disease (Tashkin, 2008).
In 1999 the Institute of Medication (IOM) completed an 18-month study on the medical value of cannabis and found that cannabis is not highly addictive, is not a gateway drug, and is safe for medical use. Specifically the IOM stated that “except for the harms associated with smoking, the adverse effects of marijuana use are within the range of effects tolerated for other medications.” At that time, the study panel maintained some concern regarding administration of cannabis by smoking, yet they clearly noted that for patients suffering from cancer or AIDS the pulmonary risks were inconsequential compared to the disease being treated. For all other patients, the IOM panel found cannabis to be safe enough to allow physicians to conduct “n of 1” (individual case) studies. For example, if a glaucoma patient’s intraocular pressure could not be controlled by standard pharmaceuticals, the physician should be allowed to use cannabis as an individual case study with that patient (Joy et al., 1999).
Since August 2016, National Institutes of Health (NIH) has been working with Office of National Drug Control Policy (ONDCP), the DEA, and the FDA to explore ways to streamline and facilitate research on cannabis. Barriers to research still exist:
- Registration process creates administrative burdens that act as disincentives to researchers. NIDA and DEA have been working to decrease the time for researcher to get Schedule I registration.
- Evaluation of consitutent compounds is hindered by the fact that although CBD does not appear to have abuse potential, all compounds in cannabis are Schedule I. In 2016, DEA began accepting applications from researchers currently registered to conduct clinical research with materials containing 99% CBD for a waiver of some regulatory requirements.
- Single source of marijuana for research. University of Mississippi, through a contract with NIDA, cultivates and distributes research grade cannabis for the United States. The NIDA supply of cannabis has diversified to include different strains, but it is costly and time consuming to grow. (NIDA, 2016)
In 2017 the NIH supported 330 projects totaling almost $140 million on cannabinoid research. Within this investment, 70 projects ($36 million) examined therapeutic properties of cannabinoids, and 26 projects ($15 million) focused on CBD (NIH, 2018).
Health Risks Related to Cannabis
No drug is without risks, and no drug works for everyone. However, given the long recorded history of cannabis used as medication and the inability to find clear evidence of harmful effects despite decades devoted to that goal, unadulterated cannabis can be said to present low risk as a medication.
The following sections discuss risks related to cannabis use, including risks related to its federally illegal status as a Schedule I drug, risks related to smoking cannabis, risks of mental health disorders, risks of impaired driving, and the potential for abuse and addiction. Additionally, certain population groups experience specific health risks related to cannabis use.
Related to Cannabis Prohibition
Over the past several decades Congress and state legislatures have passed numerous laws in the name of the war on drugs, including mandatory minimum prison sentences and asset forfeiture. In addition, a felony conviction of cannabis “manufacturing” or possession can lead to collateral damage, including revocation of professional licenses, loss of employment, loss of federal grant funding for colleges and universities, loss of child custody, and bars on voting, adoption, receiving food stamps, and living in public housing. For some patients, just admitting cannabis use to their healthcare provider or testing positive for THC in a urine drug screen may result in denial of healthcare services.
Despite the fact that cannabis is an illegal drug placed in Schedule I (forbidden medication) so that healthcare providers cannot legally prescribe it, patients throughout the country willingly take the legal risks because of the beneficial effects on their health.
Although cannabis is easy to grow, it requires knowledge and experience to grow medicinal-grade cannabis. If a patient grows it outdoors, the plants must be kept out of sight of prying eyes. If a patient grows it indoors, the plants require extra equipment and a dedicated room that must be protected from visitors. Most patients don’t have this knowledge or, due to their illness, are not able to properly tend to the plant, so they depend on an outside source. Often family members will grow it for the patient or procure it from an outside source, putting themselves in legal jeopardy as well.
When patients must obtain cannabis from an outside source they have no guarantee of the quality of their medication (eg, contamination with pesticides, heavy metals, mold). This is one of the problems of using a Schedule I drug and the cost can be extreme with no insurance coverage. And, of course, as an illegal substance, patients who use cannabis as medication do not receive the basic education about safe administration from healthcare professionals that they do with other medications.
Related to Smoking Cannabis
How many times have you heard someone justify the cannabis prohibition by declaring “We cannot approve of patients smoking their medication”? Actually, before the cannabis prohibition there were several “cigarette” preparations of cannabis developed to treat patients with asthma. We now know that there are cannabinoid receptors in the bronchi and that cannabinoids help to dilate the airways.
Inhaled cannabis smoke has effects on the lung that are similar to tobacco smoke, including increased cough, sputum production, hyperinflation, and upper lobe emphysematous changes. It does not appear that marijuana smoke contributes to the development of chronic obstructive pulmonary disease (Owen et al., 2014). One 1993 study found that cannabis smokers had more outpatient visits than people who do not smoke (NIDA, 2018).
Cannabis smoke does contain tar and other carcinogenic materials and, from a health perspective, it makes sense to avoid this route of administration (NIDA, 2018):
Marijuana smoke contains carcinogenic combustion products, including 50% more benzoprene and 75% more benzanthracene (and more phenols, vinyl chlorides, nitrosamines, reactive oxygen species) than cigarette smoke.
NIDA says that because marijuana smoke is typically inhaled deeper and held for longer, smoking marijuana may lead to four times more tar deposition than cigarette smoking (NIDA, 2018).
Donald Tashkin is the leading U.S. researcher on the clinical effects of smoking cannabis. In his extensive longitudinal study, Tashkin followed thousands of patients for years and evaluated their pulmonary status. He looked at three groups of individuals: cannabis-only smokers, cannabis-and-tobacco smokers, and tobacco-only smokers. To his surprise, the tobacco-only and cannabis-and-tobacco smokers had higher incidences of COPD or lung cancer, but the cannabis-only smokers did not. Tashkin concluded that, although the smoke itself may contain carcinogens, the cannabinoids counter the harmful effects of the smoke (Tashkin, 2008, 2013).
The well-established health risks of secondhand cigarette smoke raise reasonable questions about whether secondhand exposure to cannabis smoke poses similar risks, particularly among vulnerable populations such as children and people with asthma. At this time, little research on this question has been conducted. A 2015 study showed that THC can be measured in the blood of people who do not smoke cannabis and had spent 3 hours in a well-ventilated space with people casually smoking marijuana. Further, nonsmoking people in a confined space with people smoking high-THC marijuana reported mild effects of the drug, including a “contact high,” and had minor motor impairments (NIDA, 2018; Cone et al., 2015). Impairment of lung function equal to that caused by secondhand tobacco smoke has been found in rats exposed to secondhand marijuana smoke, and the effects lasted longer (NIDA, 2018).
A large epidemiologic study of a Los Angeles population looked at 1,212 cancer cases and 1,040 cancer-free controls; they found no positive relationship between smoking cannabis and the investigated cancer types, which included mouth, larynx, lung, and pharynx (Hashibe et al., 2006).
In 2001 Ethan Russo led a team that conducted a thorough study of the longitudinal effects of cannabis on the health of four patients in the Compassionate IND program (referred to as the Missoula Study). These four patients had been receiving cannabis from a known source from 11 to 27 years and, although they were theoretically in a research program, no one had been tracking their health status over the years. It is important to note that these patients had been using the government-issued cannabis that was grown on the farm at the University of Mississippi, then shipped to North Carolina for rolling into cigarettes and packaging them in labeled canisters that held approximately 300 cigarettes. The label identified the THC level of the cannabis and the date of processing.
The patients received low-grade medicinal cannabis containing from 2% to 4% THC and some of their shipments were up to 13 years old. The quality was poor and even included stems and seeds. At the time, Irv Rosenfeld received and consumed up to 13 ounces over a 3-week period. A complete set of pulmonary function tests was conducted on each of these patients and no long-term pulmonary damage or disease was noted except for mild bronchitis (Russo et al., 2002).
Risks Related to Mental Health
Several studies have linked marijuana use to increased risk for psychiatric disorders, including psychosis (schizophrenia), depression, anxiety, and substance use disorders. It is not clear whether the cannabis use causes or triggers these conditions.
While cannabis is often used as an anti-anxiolytic medication, one of the most common adverse effects is an acute panic reaction, which usually occurs with novice or inexperienced users or with high doses of THC (as in dronabinol or a high-THC strain of cannabis). This rarely requires any pharmacologic intervention and treatment includes a quiet, relaxing environment with reassurance that the patient is fine and the effects will soon wear off.
Research using longitudinal data from the National Epidemiological Survey on Alcohol and Related Conditions examined associations between marijuana use, mood and anxiety disorders, and substance use disorders. After adjusting for various confounding factors, Blanco and colleagues found no association between marijuana use and mood and anxiety disorders. The only significant associations were increased risk of alcohol use disorders, nicotine dependence, marijuana use disorder, and other drug use disorders (Blanco et al., 2016).
Psychotic symptoms have been described following acute cannabis consumption and claims have been made that cannabis may cause schizophrenia. Some research finds that cannabis did not “cause” schizophrenia, but its use was associated with earlier onset of symptoms and more severe psychosis, especially paranoia. Yet some schizophrenic patients report a reduction in their symptoms with the use of cannabis. Although an association has been noted, no causal relationship has been determined (Macleod et al., 2006).
In 2014, Radhakrishnan and colleagues found:
In individuals with an established psychotic disorder, cannabinoids can exacerbate symptoms, trigger relapse, and have negative consequences on the course of the illness. Several factors appear to moderate these associations, including family history, genetic factors, history of childhood abuse, and the age at onset of cannabis use. Exposure to cannabinoids in adolescence confers a higher risk for psychosis outcomes in later life and the risk is dose-related.
People with preexisting genetic vulnerability may be at increased risk for psychotic disorders when exposed to cannabinoids, as are individuals with a family history of psychotic disorders or a history of childhood trauma. The relationship between cannabis and schizophrenia fulfills many but not all of the standard criteria for causality, including temporality, biologic gradient, biologic plausibility, experimental evidence, consistency, and coherence. At the present time, the evidence indicates that cannabis may be a component cause in the emergence of psychosis, and this warrants serious consideration from the point of view of public health policy.
As cannabis use has increased in some populations, there has been no corresponding increase in the incidence of schizophrenia, which would be expected if cannabis was a causal factor. It is of interest to note that, independent of cannabis use, there are more cannabinoid receptors in the brains of patients with schizophrenia that in normal individuals.
In Brazil researchers at two separate laboratories have been conducting research with CBD as an antipsychotic medication (Crippa, 2010; Takahashi, 2010). Remember that CBD is non-psychoactive and when taken with THC it will dampen the psychoactive effects of THC. Some posit that the use of high-THC-content cannabis by patients prone to schizophrenia may trigger the onset of schizophrenia, while high-CBD content cannabis may help manage the symptoms? More research is needed in this area and, until then, patients with a family history of schizophrenia may be cautioned against the use of medicinal cannabis.
Risks Related to Impaired Driving
THC can impair perception and psychomotor performance, which means that patients may be at increased risk for accidents if operating equipment (eg, driving a vehicle). Research has shown that driving under the influence of cannabis can result in an increase in lane weaving, poor reaction time, and altered attention to the road. Marijuana affects psychomotor skills and cognitive functions critical to driving, including vigilance, drowsiness, time and distance perception, reaction time, divided attention, lane tracking, coordination, and balance. Cannabis used in combination with alcohol makes drivers even more impaired (NIDA, 2019).
Other studies have not shown impairment on these psychomotor tasks and cognitive and executive functions. It is not clear why this is the case. It may stem from different THC doses, time between doses and testing or driving, differences in the tasks used to assess the effects, tolerance developed through frequent use, and other differences (Compton, 2017).
Currently, there is no impairment standard for drivers under the influence of marijuana. There is no chemical test for marijuana impairment, like a BAC or BrAC test for alcohol that quantifies the amount of alcohol in their body, indicates the degree of impairment, and the risk of crash involvement that results from the use of alcohol. THC does not correlate well with impairment. Although very high levels of THC indicate recent consumption (for example, by smoking marijuana), it is unlikely a police officer would encounter a suspect and obtain a sample of blood or oral fluid within a short enough time for high THC levels to be detected. As was mentioned earlier, impairment is observed for 2 to 3 hours after smoking; whereas by an hour after smoking peak THC levels have declined 80% to 90% (Compton, 2017).
There are currently no evidence-based methods to detect marijuana-impaired driving. Testing of blood or urine specimens for THC is problematic because it is impractical, and while tests can confirm the presence of THC, they cannot determine degree of a driver’s impairment. Oral fluid drug screening devices are now available on a limited scale; however, the accuracy and reliability of such devices have not been clearly established (Compton, 2017).
All states have laws prohibiting driving while impaired (under the influence or intoxicated) by alcohol and other drugs, including cannabis. Some states have zero-tolerance statutes. In 2017, 12.8 million people aged 16 or older drove under the influence of illicit drugs in the past year (NIDA, 2019).
After alcohol, cannabis is the drug most often found in the blood of drivers involved in crashes. Several studies have shown that drivers with THC in their blood were roughly twice as likely to be responsible for a deadly crash or be killed than drivers who had not used drugs or alcohol. However, a large National Highway Traffic Safety Administration (NHTSA) study found no significant increased crash risk traceable to marijuana after controlling for drivers’ age, gender, race, and presence of alcohol (NIDA, 2019).
It is difficult to determine how many automobile crashes are caused by drugged driving because:
- A good roadside test for drug levels in the body does not yet exist.
- Some drugs, such as cannabis, stay in the body for days or weeks after use, making it difficult to determine if the use impaired driving.
- If alcohol is detected to be at illegal levels, police don’t test for the presence of drugs because the alcohol is sufficient for a DUI charge.
- Many drivers involved in car crashes are found to have both alcohol and drugs in their system, so it’s hard to know which substance had the greater effect. (NIDA, 2019)
With chronic use, many patients develop tolerance to the effects that may contribute to impaired driving, though research is lacking on impairment in frequent cannabis users. For users who use less than weekly, 10 mg or more of THC is likely to impair the ability to safely drive, bike, or perform other safety-sensitive activities. Colorado’s Department of Public Health recommends that less-than-weekly users should wait at least 6 hours after smoking or 8 hours after eating or drinking marijuana to allow time for impairment to resolve (Colorado Department of Public Health and Environment, 2018).
Risks Related to Cancer
Researchers have investigated the role cannabis may play in the development of certain kinds of cancers. Gurney and colleagues (2015) conducted a systematic review and meta-analysis on the association between cannabis use and testicular germ cell tumors. They found a statistically significant association between current, frequent, or chronic cannabis use and the incidence of non-seminoma-type testicular germ cell tumors. By comparison, cannabis use was not associated with a statistically significant risk of developing seminoma-type testicular germ cell tumors. Lacking further evidence, an extrapolation of this association to other types of testicular cancer is unwarranted. Gurney and colleagues (2015) found an association between the incidence of testicular cancer (without further specification) and frequent or long-term cannabis use. “There is limited evidence of a statistical association between current, frequent, or chronic cannabis smoking and non-seminoma-type testicular germ cell tumors” (National Academies, 2017).
The National Academies 2017 review of evidence concluded that smoking cannabis does not increase the risk for certain cancers (i.e., lung, head and neck) in adults. Furthermore, there is insufficient evidence to support or refute a statistical association between cannabis smoking and the incidence of esophageal cancer, prostate cancer, cervical cancer, malignant gliomas, non-Hodgkin lymphoma, penile cancer, anal cancer, Kaposi’s sarcoma, or bladder cancer (National Academies, 2017).
Risks Related to Medicinal Cannabis
Healthcare professionals are well aware of the possibility of health risks related to medications even when used under medical supervision. When using any medication, the goal is for the benefit (reason for use) to outweigh the risks (side effects and/or adverse reactions). The usual side effects that accompany the use of cannabis include a mild tachycardia, injected conjunctivae (red eye), dry mouth, short-term memory loss, relaxation, sedation, euphoria (sense of well-being), dizziness, and an increased appetite (“the munchies”). Cannabis is not a hallucinogen, but users may experience an alteration of time perception and/or an increased sensory perception.
A side effect for one patient may be a desired effect for another patient. A cancer patient may use cannabis to control the nausea and increase the appetite (for the benefit or desired effect), yet may also experience the side effects of euphoria (not generally a negative effect) and sedation. Dry mouth may be an undesired side effect for many patients, but a desired effect for ALS patients who have difficulty managing their oral secretions. The tachycardia is usually of little concern to most patients, but could be a risk to persons with cardiac disease. Many pain patients have reported that they never experience the euphoria or “high” that is sought by recreational users.
The low risk of any serious adverse event occurring with initial use of cannabis makes it an ideal first trial medication (if it were legal) for many patients. No medication works for everyone, and if cannabis is not helpful to an individual patient there is essentially no harm done in trying it. If cannabis is an effective medication, then the clinician and patient need to know the potential risks related to chronic use of this herbal medication.
The primary purpose of the Missoula Study was to determine what, if any, were the negative effects of chronic use of smoking cannabis. In addition to the pulmonary function tests, this study of the four long-term federally supplied cannabis patients included exams such as a complete physical exam, chest x-ray, MRI of the brain, neuropsychological testing, hormone and immunological assays, and an EEG. The overall conclusions were that cannabis provided these patients with symptomatic relief from pain, muscle spasms, and intraocular pressure, helped reduce their use of other prescription medications, produced no long-term sequelae, and improved their quality of life. Obviously these four patients are a small sample size, but each of these patients is convinced that cannabis is an essential medication for them (Russo et al., 2004).
Long-term use of cannabis has not been associated with increased mortality in animals or humans. In an animal study, rats were administered 50 mg/kg of THC for a period of 2 years and at the end of the observation the survival rate was higher among the treated rats than in the controls (a higher incidence of cancer was noted in the control rats) (Chan et al., 1996). A longitudinal study of 65,171 Kaiser Permanente Medical Care Program enrollees found no relationship between cannabis use and mortality (Sidney et al., 1997).
Some studies have shown a reduction in sperm count with chronic cannabis use, but it is reversible if cannabis is discontinued. A surprising 2019 study, however, found that men who had smoked marijuana had higher sperm concentration and count and lower serum FSH concentrations than men who had never smoked marijuana (Nassan et al., 2019). Studies are inconclusive regarding the effects of cannabis on male and female sterility.
Much research has been conducted on the effects of THC or cannabis on the immune system:
A large body of data from in vitro studies and animal models indicates that THC and CB2 agonists can lead to decreased resistance to infectious agents, a comparable linkage in humans has yet to be demonstrated. (Cabral et al., 2015)
The negative effects seem to be dose-related, with negative findings associated with excessive dosage.
In clinical studies of HIV-infected men, the use of cannabis was not associated with the onset of AIDS, and no negative drug interactions were found with the use of cannabis in HIV-positive adults taking protease inhibitors (Abrams et al., 2003). There has been some evidence that cannabis use is a risk factor for the progression of fibrosis in chronic hepatitis C patients (Herzode et al., 2005); however, cannabis use improved retention and virologic outcomes in patients treated for hepatitis C with interferon and ribavirin (Sylvestor et al., 2006).
Numerous case reports suggesting that cannabis use is associated with the occurrence of heart attack. A recent study warned of a possible risk of heart attack with acute cannabis intoxication. Cannabinoids affect the cardiovascular system by raising resting heart rate, dilating blood vessels, making the heart pump harder (Harvard Health Publishing, 2019). Smoking cannabis may put individuals, particularly those at high risk for cardiovascular disease, at increased risk for heart attack (National Academies, 2017). And yet chronic cannabis use has not been associated with cardiovascular risk factors such as blood triglyceride levels and blood pressure in the longitudinal CARDIA study, which began in 1986 (Grotenhermen, 2007). There is no evidence to support or refute a statistical association between chronic effects of cannabis use and the risk of heart attack (National Academies, 2017).
Smoking cannabis may have other cardiovascular effects as well. Numerous reports and studies describe vascular changes that may be associated with stroke, suggesting that smoking increases the risk of stroke. Wolff and colleagues (2013) found that several reports have indicated a close temporal relationship between cannabis smoking and stroke. In a 2015 study, Wolff and colleagues describe the effects that may lead to stroke: orthostatic hypotension with secondary impairment of the auto-regulation of cerebral blood flow, altered cerebral vasomotor function, supine hypertension and swings in blood pressure, cardioembolism with atrial fibrillation, other arrhythmias, vasculopathy, vasospasm, reversible cerebral vasoconstriction syndrome, and multifocal intracranial stenosis (Wolff et al. 2013). Wolff and colleagues (2013) concluded “cannabis has to be considered as harmful, and the cerebrovascular risk when cannabis is consumed is probably underestimated.” Among younger adults (25–34), recreational marijuana use is independently associated with 17% increased likelihood of acute ischemic stroke hospitalization (Rumalla et al., 2016). There is limited evidence of a statistical association between cannabis use and ischemic stroke or subarachnoid hemorrhage (National Academies, 2017).
There is strong evidence that people who use cannabis daily or near daily are more likely to have impaired memory lasting more than a week after quitting (Colorado Department of Public Health and Environment, 2018).
Long-term, daily, or near-daily cannabis use is associated with cyclic vomiting, and is known as cannabinoid hyperemesis syndrome. People who stop using cannabis may find the cyclic vomiting resolves.
Risks for Specific Populations
Pregnant Women
Cannabis is the illicit drug most commonly used during pregnancy. Self-reported prevalence of use during pregnancy ranges from 2% to 28% in some studies (ACOG, 2017). Some research shows that marijuana use during pregnancy is associated with risks such as preterm labor, low birth weight, neonatal intensive care admissions, and stillbirth (CDC, 2018a; Hyatbakhsh, 2013). THC readily crosses the placenta, but it appears unlikely that cannabis causes fetal abnormalities. When socioeconomic variables have been accounted for, there appear to be no significant fetal problems related to cannabis use by the mother (Dreher, 1997).
The American College of Obstetricians and Gynecologists (ACOG) published a Committee Opinion in 2017 on marijuana (Cannabis sativa) use during pregnancy and lactation. ACOG recommends the following:
- Before pregnancy and in early pregnancy, all women should be asked about their use of tobacco, alcohol, and other drugs, including marijuana and other medications used for nonmedical reasons.
- Women reporting marijuana use should be counseled about concerns regarding potential adverse health consequences of continued use during pregnancy.
- Women who are pregnant or contemplating pregnancy should be encouraged to discontinue marijuana use.
- Pregnant women or women who are contemplating pregnancy should be encouraged to discontinue use of marijuana for medicinal purposes in favor or alternative therapy for which there are better pregnancy-specific safety data.
- There are insufficient data to evaluate the effects of marijuana use on infants during lactation and breastfeeding, and in the absence of such data, marijuana use is discouraged. (ACOG, 2017)
Did You Know. . .
One in twenty, or 5%, of women use marijuana while pregnant. (CDC, 2018a)
The research on the subject of cannabis use during pregnancy is mixed, however. A study by Conner and colleagues (2016) shows that although low birth weight and preterm delivery were associated with cannabis use during pregnancy, when researchers isolated the results from tobacco use, there was no statistically significant increase in low birth weight of infants whose mothers used cannabis. The authors concluded that maternal marijuana use during pregnancy is not an independent risk factor for adverse neonatal outcomes after adjusting for confounding factors. The association between maternal marijuana use and adverse outcomes appears attributable to associated tobacco use and other confounding factors (Conner, 2016).
Lactating Mothers and Babies
Marijuana can be passed to babies in their mother’s breastmilk. THC is stored in fat and is slowly released over time, which may mean that even if a woman stops using cannabis, her baby may still be exposed (CDC, 2018a).
THC is present in human milk up to 8 times that of maternal plasma levels, and metabolites are found in infant feces, indicating that THC is absorbed and metabolized by the infant (Reece-Stremtan et al., 2015). It is rapidly distributed to the brain and adipose tissue and stored in fat tissues for weeks to months. It has a long half-life (25–57 hours) and stays positive in the urine for 2 to 3 weeks. Evidence regarding the effects of THC exposure on infant development via breastfeeding alone is sparse and conflicting, and there are no data evaluating neurodevelopmental outcomes beyond the age of 1 year in infants who are only exposed after birth (Reece-Stremtan et al., 2015).
Researchers noted that the potency of marijuana has been steadily increasing, from about 3% in the 1980s to 12% in 2012, so data from previous studies may no longer even be relevant. Furthermore, concern over cannabis use during lactation stems from possible infant sedation and the mother’s potential inability to safely care for her infant while under its influence (Reece-Stremtan et al., 2015).
According to the Academy of Breastfeeding Medicine (ABM), evidence regarding long-term effects of marijuana use by the breastfeeding mother on the infant remains insufficient to recommend complete abstention from starting or continuing breastfeeding. However, they extrapolate in utero exposure and the limited data available to make the following recommendations to health care providers in ABM Clinical Protocol #21:
- Counsel mothers who admit to occasional or rare use to avoid further use or reduce their use as much as possible while breastfeeding, advise them as to its possible long-term neurobehavioral effects, and instruct them to avoid direct exposure of the infant to marijuana and its smoke.
- Strongly advise mothers found with a positive urine screen for THC to discontinue exposure while breastfeeding and counsel them as to its possible long-term neurobehavioral effects.
- When advising mothers on the medicinal use of marijuana during lactation, one must take into careful consideration and counsel on the potential risks of exposure of marijuana and benefits of breastfeeding to the infant.
- The lack of long-term followup data on infants exposed to varying amounts of marijuana via human milk, coupled with concerns over negative neurodevelopmental outcomes in children with in utero exposure, should prompt extremely careful consideration of the risks versus benefits of breastfeeding in the setting of moderate or chronic marijuana use. A recommendation of abstaining from any marijuana use is warranted.
- At this time, although the data are not strong enough to recommend not breastfeeding with any marijuana use, ABM urges caution. (Reece-Stremtan et al., 2015)
Children and Teens
In Colorado, medical cannabis has been legal since 2000 and recreational cannabis was legalized in 2012. When Colorado became one of the first two states in the nation to legalize retail marijuana, the Colorado Legislature mandated that the Colorado Department of Public Health and Environment (CDPHE) study the potential public health effect of cannabis use. The 2018 Monitoring Health Concerns Related to Marijuana in Colorado report tracks information about cannabis use among children and teens in this state. In 2017 Healthy Kids Colorado Survey estimated 19.4% of Colorado high school students and 5.2% of middle school students reported using marijuana in the past 30 days. Past-30-day use has remained stable among high school students since 2005 and among middle school students since 2011. Use among high school students in Colorado is not statistically different than national estimates of past-30-day use. Prevalence of use increases with grade level. Frequency of use has declined or remained stable among adolescents. Use of cannabis is higher than smoking cigarettes, but less than alcohol use and nicotine vaping among high school students (MHMRP, 2018).
In 2017 the Child Health Survey estimated 11.2% of homes with children reported cannabis being present in or around the home, which is up from 6.9% in 2014. Survey respondents reported storing marijuana safely by keeping it in child-resistant packaging, out of reach, or in a locked location. Also in 2017 it was estimated that 23,009 homes in Colorado with children aged 1 to 14 years had marijuana in the home and potentially stored unsafely (MHMRP, 2018).
In Colorado homes with children cannabis is smoked, vaporized, or dabbed (83.1%), and 33% reported marijuana edibles being used in the home. It is estimated that approximately 32,800 homes with children aged 1 to 14 had possible second-hand marijuana smoke or vapor exposures (MHMRP, 2018).
The Colorado Retail Marijuana Public Health Advisory Committee reviewed unintentional marijuana exposure relative to marijuana legalization and child-resistant packaging. They found strong evidence that more unintentional marijuana exposures of children occur in states with increased legal access to marijuana, and that exposures can lead to significant clinical effects requiring hospitalization. Evidence shows that child-resistant packaging prevents exposure to children from potentially harmful substances, such as THC (MHMRP, 2018).
Accidental ingestion/exposure in homes with cannabis products, especially edibles, is on an upward trend in Colorado. Data from the Rocky Mountain Poison and Drug Center show that in 2017 edible marijuana products comprised 65.6% of all exposures in children ages 0 to 8 years, followed by smokable products (23.4%) and other marijuana products (10.9%) (MHMRP, 2018).
Children’s Hospital Colorado recommends the following precautions if marijuana products are in the home where children live or visit:
- Keep marijuana up and away and out of the sight of children. Pick a place your children cannot reach.
- Put marijuana away every time, even products you use every day.
- Consider purchasing a medication lock box for safe, convenient storage of marijuana products.
- Talk to your children about marijuana, and teach your children about medicine safety.
- Ask houseguests and visitors to keep purses, bags, or coats that have marijuana products in them away and out of sight when they are in your home.
- If you use a babysitter, choose those who are mature, trained and responsible, and are recommended by someone you trust.
- Ask other parents if they have marijuana products in their home before sending your child to play at their house. Ask that they make sure all products are stored up and away and out of children’s sight.
- Be prepared in case of an emergency; program the poison control number into your phone. (Children’s Hospital Colorado, 2019)
Did You Know. . .
38% of high school students report having used marijuana in their life (CDC, 2018b).
Decline in School Performance
According to the CDC, use of cannabis in adolescence or early adulthood can have a serious impact on a teen’s life. Some research shows that cannabis can have permanent effects on the developing brain when use begins in adolescence, particularly in regular and heavy use (CDC, 2018b). Students who smoke marijuana may get lower grades and may more likely to drop out of high school than their peers who do not use (CDC, 2018b, citing a 2016 systematic review by Broyd et al. of research published between January 2004 and February 2015 on acute and chronic effects of cannabis and cannabinoids and on persistence or recovery after abstinence).
Some studies suggest regular marijuana use in adolescence is associated with altered connectivity and reduced volume of specific brain regions that are involved in a range of executive functions such as memory, learning, and impulse control compared to people who do not use. Other studies have not found significant structural differences between the brains of people who do and do not use the drug (NIDA, 2018). Some studies suggest that marijuana use can cause functional impairment in cognitive abilities but that the degree and duration of the impairment depends on the age at which cannabis use began and how much and how long the person used cannabis (NIDA, 2018).
A longitudinal New Zealand study found that persistent marijuana use disorder with frequent use starting in adolescence was associated with a loss of 6 to 8 IQ points measured in mid-adulthood. In that study, those who used marijuana heavily as teenagers and quit using as adults did not recover the lost IQ points. People who only began using marijuana heavily in adulthood did not lose IQ points. These results suggest that marijuana has its strongest long-term impact on young people whose brains are still busy building new connections and maturing in other ways (NIDA, 2018).
At the 2016 Neuroscience Research Summit on Marijuana and Cannabinoids, Susan Tapert presented on adolescent marijuana use and its influence on learning, memory, and brain changes. She noted that it is presently unclear how the use of marijuana affects the major brain development processes that occur during adolescence, and made five points about what we know about marijuana use and cognition:
- Marijuana adversely influences learning.
- Memory and attention also can show long-term effects.
- These outcomes improved with days to weeks of abstinence.
- The effect of marijuana on cognition appears worse with earlier age of onset.
- Some neuroimaging data support these effects of marijuana. (NIH, 2016)
There is moderate evidence of a statistical association between acute cannabis use and impairment in the cognitive domains of learning, memory, and attention. There is limited evidence of a statistical association between sustained abstinence from cannabis use and impairments in the cognitive domains of learning, memory, and attention (National Academies, 2017).
Dating Violence Among Adolescents and Young Adults
A number of studies have linked cannabis use to intimate partner violence. Among young adults, all analyzed patterns of marijuana use during adolescence and early adulthood were associated with a 1.2 to 2.4 times increased risk of intimate partner violence perpetration and victimization (Reingle et al., 2012). Researchers found that any use of marijuana during adolescence and young adulthood increases the risk of intimate partner violence. Consistent users were at greatest risk of perpetration and victimization, independent of alcohol use and other risk factors. Unexpectedly, results indicated that males were more likely to be victims and less likely to be perpetrators of intimate partner violence compared with females (Reingle et al., 2012). A recent review and meta-analysis of literature published between 2003 and 2015 by Johnson and colleagues found that among people ages 11 to 21, adolescent girls who use marijuana may be more likely to commit physical violence against their dating partners, and adolescent boys who use marijuana may be more likely to be victims of physical dating violence (Johnson et al., 2017; MHMRP, 2018). Findings suggest that marijuana use is associated with a 54% increase in the odds of physical dating violence victimization, and a 45% increase in the odds of perpetration (Johnson et al., 2017).
Risks Related to Abuse and Addiction
Since marijuana is commonly referred to as a drug of abuse, the risk of tolerance, dependence, and addiction should be addressed. Tolerance is defined as the need to increase the dose with chronic use to in order to get the same effects. Healthcare professionals commonly see this with the use of opioids for chronic pain; over time patients develop a tolerance and require higher doses to manage their pain. When used medicinally on a regular basis over a period of time, patients who use cannabis often develop a tolerance to the cognitive and psychomotor impairment as well as the psychological “high,” yet they do not develop a tolerance to its medicinal benefits.
The first patient admitted into the Compassionate IND program, Robert Randall, consumed 10 cannabis cigarettes per day for years to control his intraocular pressure. One month, he seemed to be going through his supply faster than usual. Upon further investigation he discovered that his federal prescription had been changed without his or his physician’s knowledge. Each of his cannabis cigarettes contained 0.8 grams of cannabis rather than the usual 1 gram. Not realizing this decrease in dosage, he simply smoked more cigarettes to continue with his daily requirements. Once discovered, his physician complained and the correct dosage was provided in his next cannabis shipment (Randall and O’Leary, 1998). On the other hand, patients have noticed a tolerance to the therapeutic effects with the use of dronabinol (synthetic THC).
Dependence is a term often misused as a synonym for addiction, but the two terms are not synonymous. Dependence (also referred to as physical dependence) is the result of continued regular use of a drug that produces a physiologic change in the central nervous system to the extent that abrupt cessation of the drug causes withdrawal symptoms.
The seriousness of the withdrawal symptoms depends upon the drug being used and the extent of its use (risks increase with higher doses over long periods of time). For those drugs that do produce physical dependence, there is an expected physiologic response that would occur in anyone who used the drug on a regular basis, but this is not by itself indicative of addiction. For some drugs, such as alcohol or benzodiazepines, withdrawal symptoms can be serious and life-threatening. Opioids can cause withdrawal symptoms similar to a severe case of the flu. However withdrawal from cannabis is generally mild in comparison. Cannabis withdrawal symptoms may include irritability, restlessness, difficulty sleeping, decreased appetite, anxiety, anger, and strange dreams. Less common symptoms include headaches, sweating, chills, stomach pain, and general discomfort.
Most of the cannabis withdrawal symptoms begin within 24 hours following abrupt cessation, are most severe 2 to 4 days later, and last 1 to 2 weeks. Withdrawal from cannabis is generally uncomfortable but not dangerous and does not require medical management. Not all persons complain of withdrawal when discontinuing use. A large survey in Australia found approximately 30% of current marijuana users reported withdrawal symptoms when they stopped using cannabis (Teesson et al., 2002).
It seems important to note that some patients begin using cannabis to manage what some researchers consider withdrawal symptoms. Patients have used cannabis as a sleep aid, appetite stimulant, relaxant, and calming agent. If they stop using cannabis, are their initial reasons for use simply reemerging or are they experiencing true withdrawal symptoms?
Cannabis abuse is a very ambiguous and value-laden term, and therefore its use is questionable. “Drug abuse” has often been defined as use of a drug without a prescription or use of an illegal drug. Those notions are not very helpful. Some persons or cultures may not accept the paternalistic notion that only a physician can decide whether a person should use a drug, when to use it, or how often to use it. And the idea that drugs are legal or illegal leads many people to believe that the legal drugs are good and the illegal drugs are bad. Drugs are not inherently good or bad but, as Andrew Weil noted years ago, it is their manner of use that is either bad or good (Weil & Rosen, 1993).
Addiction (sometimes referred to as psychological dependence) is defined as a pattern of drug abuse characterized by an overwhelming preoccupation with the compulsive use of a drug and securing its supply, and a high tendency to relapse if the drug is taken away. Tolerance and dependence are common results of addiction, but are not necessary components of addiction. The new edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) of the American Psychiatric Association (APA) has been developed with the input of thousands of expert psychiatrists over several decades to classify and characterize human mental health disorders, including substance-use disorders. To provide some continuity in the concept/diagnosis of cannabis addiction, clinicians can use the criteria set up in the DSM-5 (as reported in the DSMV, 2013).
According to the DSM-5, substance use disorders has replaced the terms abuse or addiction and they are identified by drug type, so here we use the term cannabis use disorder, and depending upon the number of positive criteria, the person is diagnosed with a mild, moderate or severe cannabis use disorder. Below is a list of the 11 criteria of which at least 2 must be met within a 12-month period:
- Cannabis is often taken in larger amounts or over a longer period than was intended.
- There is a persistent desire or unsuccessful efforts to cut down or control cannabis use.
- A great deal of time is spent in activities necessary to obtain cannabis, use cannabis, or recover from its effects.
- Craving, or a strong desire or urge to use cannabis.
- Recurrent cannabis use resulting in a failure to fulfill major role obligations at work, school, or home.
- Continued cannabis use despite having persistent or recurrent social or interpersonal problems caused or exacerbated by the effects of cannabis.
- Important social, occupational, or recreational activities are given up or reduced because of cannabis use.
- Recurrent cannabis use in situations in which it is physically hazardous.
- Cannabis use is continued despite knowledge of having a persistent or recurrent physical or psychological problem that is likely to have been caused or exacerbated by cannabis.
- Tolerance, as defined by either of the following: (a) a need for markedly increased amounts of cannabis to achieve intoxication or desired effect or (b) markedly diminished effect with continued use of the same amount of cannabis.
- Withdrawal, as manifested by either of the following: (a) The characteristic withdrawal syndrome for cannabis (the following symptoms develop within a week of cessation of cannabis: irritability, anger or aggression; nervousness or anxiety; sleep difficulty; decreased appetite or weight loss; restlessness; depressed mood; and at least one of the following physical symptoms: abdominal pain, shakiness/tremors, sweating, fever, chills, or headache. (b) Cannabis (or a closely related substance) is taken to relieve or avoid withdrawal symptoms.
Addiction to cannabis rarely occurs because, in general, persons who have problems with drug addiction usually prefer more potent psychoactive drugs and caution should be used in making a cannabis use disorder diagnosis to ensure that the problems come from the use of cannabis rather than from the prohibition of cannabis. When dronabinol was initially approved as a medication it was placed in Schedule II of the CSA. After several years on the market, it was down-regulated to Schedule III because of the lack of diversion and little evidence of addiction. Initially, animal studies are used to evaluate the abuse potential of drugs, with the understanding that these do not necessarily reflect similar outcomes in humans. It is important to note that numerous studies have concluded that while cannabis may produce a feeling of euphoria in humans, in general animals will not self-administer THC (DSM-V, 2013).
In 1994 Jack E. Henningfield, of the National Institute on Drug Abuse (NIDA), and Neal L. Benowitz, of the University of California at San Francisco (UCSF), ranked six commonly used drugs by five criteria: withdrawal symptoms (dependence), reinforcement (craving), tolerance, dependence (addiction) potential, and intoxication. They ranked the six drugs from 1 as the most serious to 6 as the least serious. Cannabis (marijuana) was ranked lowest for withdrawal symptoms, tolerance, and dependence (addiction) potential; it ranked close to caffeine in the degree of reinforcement and higher than caffeine and nicotine only in the degree of intoxication (Henningfield & Benowitz, 1994).
Ranking of Six Commonly Used Drugs |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
Withdrawal |
Reinforcement |
Tolerance |
Dependence |
Intoxication |
|||||
|
NIDA |
UCSF |
NIDA |
UCSF |
NIDA |
UCSF |
NIDA |
UCSF |
NIDA |
UCSF |
Nicotine |
3 |
3 |
4 |
4 |
2 |
4 |
1 |
1 |
5 |
6 |
Heroin |
2 |
2 |
2 |
2 |
1 |
2 |
2 |
2 |
2 |
2 |
Cocaine |
4 |
3 |
1 |
1 |
4 |
1 |
3 |
3 |
3 |
3 |
Alcohol |
1 |
1 |
3 |
3 |
3 |
4 |
4 |
4 |
1 |
1 |
Caffeine |
5 |
4 |
6 |
5 |
5 |
3 |
5 |
5 |
6 |
5 |
Marijuana |
6 |
5 |
5 |
6 |
6 |
5 |
6 |
6 |
4 |
4 |
Also in 1994, the U.S. National Comorbidity Study found that 9% of lifetime cannabis users met the DSM-R-III criteria for dependence at some time in their life, compared to 32% of tobacco users, 23% of opiate users, 17% of cocaine users, and 15% of alcohol users (Anthony, et al., 1994). It does appear that early onset of first use of cannabis is associated with an increased risk of later developing addiction. According to the National Survey on Drug Use and Health, in 2015, about 4.0 million people in the United States met the diagnostic criteria for a marijuana use disorder; 138,000 voluntarily sought treatment for their marijuana use.
Research Gaps
The National Academies of Sciences, Engineering, and Medicine (National Academies) Committee on the Health Effects of Marijuana published a report entitled An Evidence Review and Research Agenda (National Academies, 2017). The Committee on the Health Effects of Marijuana consisted of 16 experts in the areas of marijuana, addiction, oncology, cardiology, neurodevelopment, respiratory disease, pediatric and adolescent health, immunology, toxicology, preclinical research, epidemiology, systematic review, and public health. The committee reviewed the current evidence base for the potential efficacy of cannabis or cannabinoids on prioritized health conditions, including chronic pain, cancer, chemotherapy-induced nausea and vomiting, anorexia and weight loss associated with HIV, irritable bowel syndrome, epilepsy, spasticity, Tourette syndrome, amyotrophic lateral sclerosis, Huntington’s disease, Parkinson’s disease, dystonia, dementia, glaucoma, traumatic brain injury, addiction, anxiety, depression, sleep disorders, posttraumatic stress disorder, and schizophrenia and other psychoses.
The committee has identified that research gaps exist concerning the effectiveness of cannabidiol or cannabidiol-enriched cannabis in treating the following conditions:
- Cancer in general
- Chemotherapy-induced nausea and vomiting
- Symptoms of irritable bowel syndrome
- Epilepsy
- Spasticity due to paraplegia from spinal cord injury
- Symptoms associated with amyotrophic lateral sclerosis (ALS)
- Motor function and cognitive performance associated with huntington’s disease
- Motor system symptoms associated with parkinson’s disease or levodopa-induced dyskinesia
- Achieving abstinence or reduction in the use of addictive substances, including cannabis itself
- Sleep outcomes in individuals with primary chronic insomnia
- Post traumatic stress disorder symptoms
- Mental health outcomes in individuals with schizophrenia or schizophreniform psychosis
- Cannabidiol short-term relief from anxiety symptoms (National Academies, 2017)
NIH believes that FDA’s drug review and approval process is the best way to ensure that new medicines, including those derived from marijuana, are appropriately evaluated for safety and effectiveness. To date, the FDA has approved three medications, Marinol (dronabinol), Cesamet (nabilone), and Syndros (oral drabinol solution), for severe nausea and wasting in patients with HIV and cancer. These medications contain synthetically-derived cannabinoids. Dronabinol is identical in chemical structure to delta-9-tetrahydrocannabinol (THC), the main active ingredient found in the marijuana plant; nabilone is similar in structure to THC. With Americans across the country consuming marijuana for health related conditions, there is a pressing need for more research in this area (NIDA, 2016).
