It has been well-established that influenza vaccination reduces influenza-associated illness. CDC estimates that tens of thousands of hospitalizations are averted because of vaccination each year and that vaccination prevents millions of influenza-related illnesses. This is despite that fact that fewer than half of those over the age of 6 months are vaccinated each year. Higher vaccination rates almost certainly would prevent a substantial number of additional cases and hospitalizations.
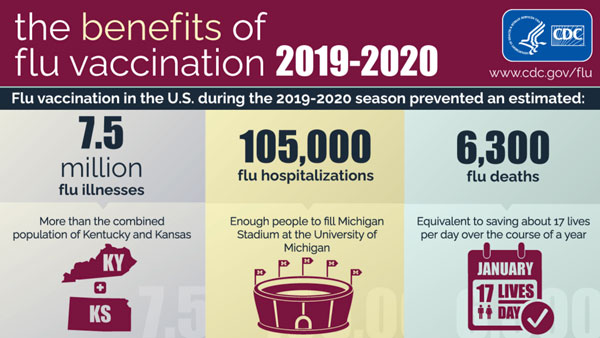
Source: CDC.
Since 2010 CDC has recommended that all people 6 months of age and older receive annual influenza vaccination. Despite gains in the number of people vaccinated each year, we have yet to come close to the goal of universal influenza vaccination.
Influenza Vaccination Coverage, 2020–2021 Season | |
|---|---|
Age group | (2020–2021 rates) |
All people (≥6 months) | 52.0% |
Children (6 months–17 years) | 58.6% |
Adults (18–49 years) | 37.7% |
Adults (50–64) | 54.2% |
Adults 65 and older | 75.2% |
Healthcare personnel | 75.9% |
Flu Vaccination Coverage by Age Group,
Children 6 months–17 years, United States, 2010–2021
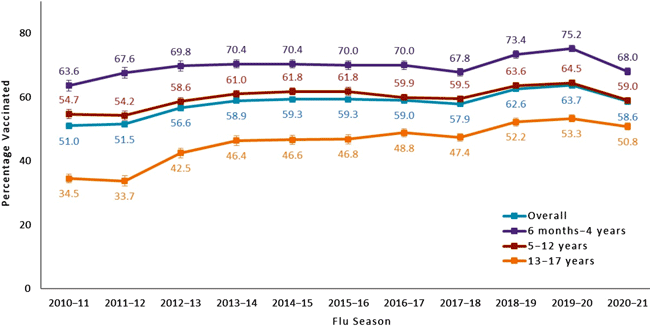
Data Source: National Immunization Survey-Flu (NIS-Flu)
Error bars represent 95% confidence intervals around the estimates.
Source: CDC.
The College of Physicians of Philadelphia provides a fascinating look at the issues associated with vaccines on their History of Vaccines website. It is well worth the time to look over the website and explore “the ways in which vaccines, toxoids, and passive immunization work, how they have been developed, and the role they have played in the improvement of human health.”
Adult Vaccination Rates
For the 2020–2021 season, flu vaccination coverage among adults ≥18 years was 50.2%, a slight increase from the prior season. Half of people ≥6 months were vaccinated during the 2020–2021 season, similar to coverage in the prior season. Flu vaccination coverage has increased for adults over the past three flu seasons and had also been increasing for children until the 2020–2021 season (CDC, October 7, 2021).
Racial/ethnic disparities in flu vaccination coverage persist. Non-Hispanic Black children had lower flu vaccination coverage than children in all other racial/ethnic groups, and Hispanic children had lower coverage than non-Hispanic white children and children of other or multiple other races. Hispanic adults and Black adults had lower flu vaccination coverage than white adults and adults of other races (CDC, October 7, 2021).
Vaccination Rates Decline as Clinic Day Progresses
A retrospective study of 11 primary care practices at the University of Pennsylvania Health System from 2014 to 2017 yielded interesting results. Researchers found that influenza vaccination rates significantly declined as the clinic day progressed.
Offering an “active choice” intervention in which medical assistants were prompted to ask patients about vaccinations and record the answers in patients’ electronic health record for clinicians to review was associated with a significant increase in vaccination rates. Importantly, the active choice intervention was associated with a significant increase in influenza vaccination rates that were similar in magnitude throughout the day.
Source: Kim et al., 2018.
Vaccination Rates Among Children
Influenza-associated deaths in children (less than 18 years) were added as a nationally notifiable condition in 2004. For children in the U.S., influenza vaccination rates are higher in young children but decrease with increasing age. During the 2020-2021 flu season vaccination rates in children were as follows:
- 6 months–4 years: 68%
- 5–12 years: 59%
- 13–17 years: 50.8%
- All children: 58.6%
Healthcare Worker Vaccination Rates
Overall, 75.9% of healthcare personnel reported receiving influenza vaccination during the 2020–21 season. Coverage was lower than in the previous season (80.7% for 2019–20) (CDC, October 7, 2021).
During the 2020-2021 flu season, physicians, nurses, and pharmacists had the highest coverage (91.3%, 90.3%, and 90.3%). Coverage significantly decreased in 2020–21 season among assistant/aides, pharmacists, and healthcare workers with an associate or bachelor’s degree (CDC, October 7, 2021).
As in previous seasons, non-clinical personnel and assistants/aides, healthcare personnel working in long term care facilities or home health care settings and healthcare personnel with less than a college degree had the lowest coverage among all occupations, work settings and education levels, respectively (CDC, October 7, 2021).
Did You Know. . .
Workplace vaccination programs that have been successful in increasing coverage in hospital settings could be implemented in long-term care and other settings with lower vaccination coverage.
Employers can use the long-term care web-based toolkit developed by CDC and the National Vaccine Program Office to access resources, strategies, and educational materials for increasing influenza vaccination among healthcare personnel in long-term care settings (Black et al., 2017).
Low vaccination rates are certainly at least partly related to high staff turnover, especially in long term care. It is not uncommon for a long-term facility's staff to turn over completely every few years. Newly hired managers may not adhere to existing policies related to vaccinations, or they may decide to discard such policies and implement new ones.
Issues related to COVID-19 vaccination has shed light on some of the difficulties faced by organizations trying to increase flu vaccination rates. In March 2021, data from 300 long-term care facilities across the U.S. highlighted disparities in COVID-19 vaccination coverage, with a 30% difference in coverage between physicians and other advanced practice providers (75.1%) and aides (45.6%) (Lee et al., 2021).
Among aides, lower COVID vaccination coverage was observed in facilities located in more socially vulnerable zip code areas. This suggests that COVID vaccination disparities among job categories mirror social disparities in general as well as disparities in the surrounding communities. Vaccination promotion and outreach efforts focused on socially vulnerable and marginalized groups and communities could help address inequities (Lee et al., 2021).
Healthcare workers with the most patient contact had the lowest COVID vaccination coverage (like flu vaccination rates). In long-term care facilities, where residents were highly vaccinated, COVID transmission occurred through unvaccinated staff members (Lee et al., 2021).
This finding has equity implications: aides in nursing homes are disproportionately women and members of racial and ethnic minority groups, with median hourly wages of $13–$15 per hour. Aides are more likely to have underlying conditions that put them at risk for adverse outcomes from COVID-19. As vaccination was made available on site, vaccine hesitancy may have been an important contributor to under-vaccination in these facilities (Lee et al, 2021).
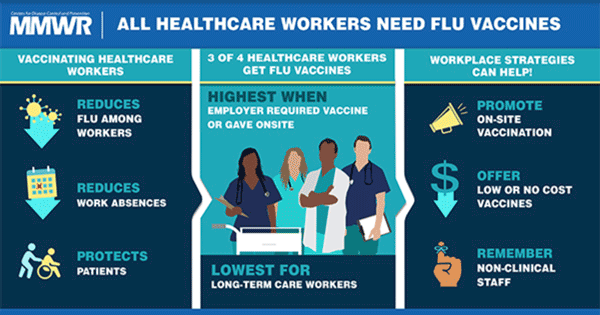
Source: Morbidity and Mortality Weekly Report, 2018.
Vaccination Rates by Healthcare Setting
[Material in this section from CDC, 2021, October 17 unless otherwise cited.]
By setting, coverage was highest among healthcare personnel working in hospitals (91.6%) and lowest among healthcare personnel working in long-term care facilities and home health care settings (66.0%). An employer vaccination requirement was one of the strongest factors associated with vaccine receipt; coverage was the highest among healthcare personnel who were required by their employer to be vaccinated (95.9%), and the lowest among healthcare personnel whose employers neither required nor recommended vaccination (46.0%).
Receipt of a COVID-19 vaccine was the second strongest factor correlated with higher influenza vaccination coverage. Implementing workplace strategies to improve vaccination coverage among healthcare personnel, particularly those working in long-term care and home healthcare settings, ensures that healthcare personnel and patients are protected against influenza. Reducing the overall burden of respiratory illnesses by maximizing healthcare personnel influenza vaccination uptake can protect healthcare personnel and vulnerable populations and conserve healthcare resources for the treatment of COVID-19 patients.
