Each year, we must decide whether to get vaccinated against the flu. Many of us get the vaccine without a second thought, while a significant percentage of healthcare personnel either choose not to get vaccinated or simply never get around to it.
Vaccine Hesitancy
Vaccines are generally safe, effective, and relatively inexpensive. They save about three million lives every year and protect hundreds of millions of people against acute and chronic infections and their consequences. While administering a vaccine is a fairly simple process, the enterprise of vaccination is complex. To invent, test, and produce a vaccine is difficult, and protecting people against infectious diseases requires high levels of organization and participation (Sabin Vaccine Institute, 2020).
For many individuals, the health benefits associated with vaccination is not a sufficient reason to embrace vaccination. Some doubt the benefits of vaccines, worry over their safety, and question the need for them, an attitude referred to as vaccine hesitancy. This differs from vaccine refusal; even those who are vaccinated can harbor hesitancy toward certain aspects of vaccination (Yaqub et al., 2014).
Despite considerable evidence showing vaccines are safe, there is increasing skepticism toward vaccination. Vaccine hesitancy has led to a decline in vaccine uptake and to an increase in the prevalence of vaccine-preventable diseases. Ironically, the objection to vaccines is commonly a consequence of their effectiveness—because individuals have lower exposure to vaccine-preventable diseases, they are less concerned about contracting them, which consequently leads to greater vaccine hesitancy (Fridman, Gershon, Gneezy, 2021).
While coverage rates are helpful for identifying those who reject vaccines, it does little to help us understand hesitant attitudes, their origins, and how to change them. Maintaining high coverage rates ensures that vaccination benefits are delivered widely, but the very act of delivering wide-scale vaccination can make vaccines “victims of their own success.” As the ravages of disease become less familiar to people, it becomes more challenging to explain the benefits of vaccination (Yaqub et al., 2014).
Reasons for Refusing the Flu Vaccine
Why so many people, both in and out of healthcare, decide not to get vaccinated against influenza each year? In a 2021 survey of healthcare personnel, the main reasons cited among unvaccinated healthcare personnel were:
- “I do not need the vaccination” (17.3%)
- “I might experience side effects or get sick from the vaccine” (12.2%)
- “I don’t think the vaccination is effective in preventing flu” (11.8%).
CDC, 2021, October 7
Misconceptions about vaccination include:
- A fear that the immune system will be “overloaded” by vaccines, especially in children.
- The belief that many common diseases have disappeared, and it is no longer necessary to vaccinate against them.
- The belief that more vaccinated than unvaccinated people get sick.
- The belief that hygiene and better nutrition are responsible for the reduction in disease rates, not vaccination.
- The belief that natural immunity is better than vaccine-acquired immunity. (College of Physicians of Philadelphia, 2022)
Main Reasons Reported for Not Getting the Flu Vaccine
Among Healthcare Personnel
Internet Panel Survey, April 2021, USA
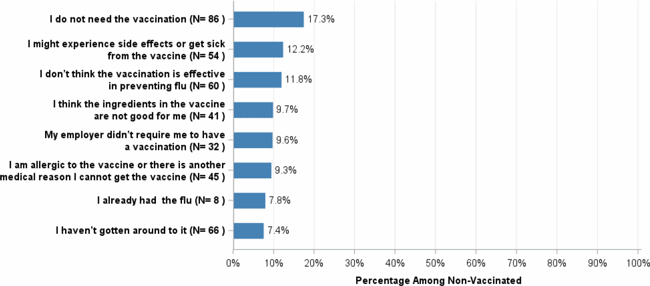
Source: CDC, 2021, October 7.
Reasons for Accepting the Flu Vaccine
When I first started work as a nurse, I never got a flu shot. If I got the flu, I went to work even though I was sick. One year I got the flu shot on a Friday morning and was sick as a dog by the evening. Now I know that I already had the flu when I got the shot—back then I blamed it on the vaccine and didn’t get a shot for several more years. One year I got the flu, missed several days of work, and coughed my lungs out for almost two weeks. After that I thought, this is ridiculous, the flu vaccine will stop all of this. It was a no-brainer. Now I get a shot every year.
ER Nurse, California, 2022
For healthcare personnel, there are many good reasons to get a flu vaccine, not least of which is they are less likely to become ill themselves and much less likely to pass the virus on to their patients and families.
In a 2021 survey of healthcare personnel, the main reasons cited for receiving an influenza vaccine were:
- “To protect myself from flu” (36.0%),
- “Because it was mandatory, or I had to for work” (22.3%) and
- “To reduce flu’s impact on the healthcare system during the COVID-19 pandemic” 10.5%) (CDC, 2021, October 7).
Main Reasons Reported for Getting the Flu Vaccine
Among Healthcare Personnel
Internet Panel Survey, April 2021, USA
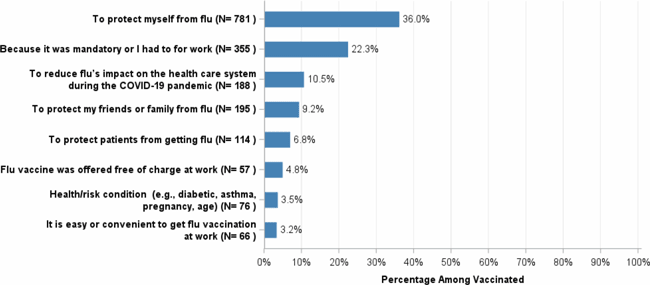
Source: CDC, 2021, October 7.
During the 2009–2010 H1N1 influenza pandemic in France, Germany, and Mexico, the most common reason given to be vaccinated for A/H1N1 pandemic influenza was a physician's advice or recommendation. In the U.S., media advertising was the most important motivating factor, although a physician's advice was nearly as important (Blank et al., 2012).
Encouraging Vaccinations
Useful resources that can help with increasing vaccination coverage among healthcare personnel include CDC’s long-term care web-based toolkit, which provides access to resources, strategies, educational materials, and interventions recommended by the Community Preventive Services Task Force. These resources can be used by healthcare employers to increase influenza vaccination coverage among healthcare personnel and reduce influenza-associated morbidity and mortality among patients (CDC, 2021, October 7).
Given relatively lower COVID-19 vaccination coverage in the same healthcare personnel subgroups that showed lower influenza vaccination coverage, it is especially important to implement systems that support and encourage vaccination, particularly healthcare personnel working at long-term care facilities and home healthcare settings (CDC, 2021, October 7).
Outbreaks of COVID-19 in long-term care facilities have had a critical impact on the health of vulnerable older adults. Many of the long-established public health actions aimed at increasing influenza vaccination coverage among healthcare personnel can be used not only for routine vaccinations but also for improving a COVID-19 vaccination coverage (CDC, 2021, October 7).
