COPD is generally caused by long-term exposure from environmental irritants such as smoke (including second-hand smoke), air pollution, fumes, and wood smoke. A rare cause can be from a deficiency in alpha-1 antitrypsin; without the enzyme, the body is not able to break down mucus, which leads to thick mucus building up in patients with COPD from smoking.
Causes of Emphysema
Cigarette smoking is the primary cause of all types of COPD, and emphysema is caused by long-term environmental exposures. The difference between general COPD and emphysema or bronchitis is the over-inflation and stiffening of the lungs with emphysema, making gas exchange difficult.
Causes of Asthma
Asthma can be triggered by environmental factors that cause the airways to constrict. Why do some people respond to certain environmental irritants and others do not? Genetic studies are looking at autoimmune genetic differences. The exact cause of these differences is not yet known but studies do point to variations in the genetic code.
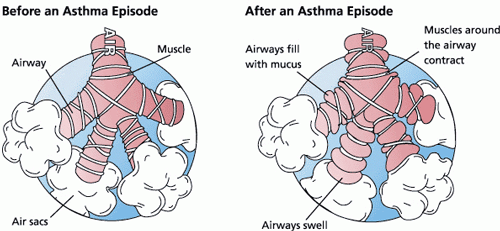
There are two types of asthma, intermittent and persistent. Intermittent asthma can be caused by an occasional allergic reaction to an environmental or emotional trigger, with constriction of the airways for up to two days a week. Persistent asthma becomes uncontrolled without medication. Classic causes of asthma include dust, pollutants, strenuous exercise, and even emotional stress, to all of which the body responds by closing off the airways, which leads to an asthma attack.
The hyperreactivity of the airways in asthma generally progress to bronchoconstriction, airway wall edema, chronic mucus plug formation, and chronic airway remodeling (Glass, 2014).
Source: Wikimedia Commons.
Causes of Chronic Bronchitis
Bronchitis is a type of COPD caused by mucus retention in the lungs and bronchial passageways due to chronic irritation and inflammation.
The cause of acute bronchitis is generally viral or bacterial; however, the cause of chronic bronchitis is a chronic irritant. It is characterized by persistent productive cough and is generally due to smoking. For those non-smokers who develop chronic bronchitis, the cause may be from air pollution, dust, or other environmental triggers. Those with autoimmune diseases may also experience hypersensitivity to triggers. Whereas acute bronchitis may be cured by being treated with antibiotics and cough suppressants, chronic bronchitis has no cure but can be managed with medications.
Risk Factors
As noted earlier, smoking, pollutants, and genetics all play a role in the development of COPD. Smoking is the #1 controllable risk factor for COPD and much attention and effort should be placed on helping people to stop smoking. It is the first intervention a healthcare professional should initiate for a patient with smoking-caused COPD.
Other air pollutants are more difficult as they may not be within someone’s choice or ability, such as those who live in polluted cities, or work in industrial environments with poor air quality. In Asia it is now quite common to see people walking the streets and taking trains and buses wearing simple air filter masks.
Non-controllable risk factors include genetic mutations or autoimmune diseases that react in a hypersensitive or allergic way.
Identifying Patients at Risk
A valid and costly concern for health maintenance organizations (HMOs) and insurance companies is that numerous patients are hospitalized for acute exacerbations of their COPD, which could have been avoided by careful management by their primary physician. A hospitalization from a COPD exacerbation can cost thousands of dollars. The national guidelines and the GOLD standard* for COPD diagnosis and management were created based on numerous clinical studies. It has been adopted by HEDIS** for insurance reimbursement and by the Center for Medicare Services (CMS).
*The Global Initiative for Chronic Obstructive Lung Disease (GOLD) works with healthcare professionals and public health officials to raise awareness of Chronic Obstructive Pulmonary Disease (COPD) and to improve prevention and treatment of this lung disease for patients around the world.
**The Healthcare Effectiveness Data and Information Set (HEDIS) is a tool used by more than 90 percent of America’s health plans to measure performance on important dimensions of care and service. Altogether, HEDIS consists of 94 measures across 7 domains of care.
By surveying and tracking reports of people with COPD across all states, improvements can be made in identifying communities at risk who may benefit from awareness, outreach, and public health efforts in prevention, treatment, and control of the disease. Efforts to survey patients with COPD in all states has been done by the Centers for Disease Control using the Behavioral Risk Factor Surveillance System (BRFSS) (CDC, 2012). Of those who self-identified as COPD, 76% stated they received a diagnostic breathing test, 64% felt the shortness of breath negatively impacted their quality of life, and 55% were taking at least one medication for their COPD (Kosacz, 2012). Because the spirometry test can be costly, it is not used as a general screening tool for COPD; currently there is no general public screening tool in use.
Predisposing factors include the environmental pollutants and also include secondhand smoke, genetic factor of alpha-1 antitrypsin (AAT) deficiency, recurrent or chronic lower respiratory infections, or disease and age over the fifth decade of life.
Apply Your Knowledge
Picture your own patients who have COPD, emphysema, chronic bronchitis, and asthma. How are they the same? How are they different? What similarities in medications do they receive? What interventions applied for each?
Online Resource
YouTube (3:59): Reducing the Risk of COPD
https://www.youtube.com/watch?v=4fEiZ64q-J8
Test Your Knowledge
Which one is a cause of all three types of COPD?
- Inflammation and environmental triggers
- Cigarette smoking
- Industrial pollutants
- Genetic mutations in mucus production
Answer: A
