By identifying diabetes early many chronic complications can be avoided or minimized. Cardiovascular and microvascular complications may be prevented or delayed when glycemic levels are controlled. A hallmark study known as the Diabetes Control and Complications Trial (DCCT) revealed maintaining blood glucose levels to a near-normal level may significantly reduce chronic complications. The DCCT demonstrated in 1993, in the final report of the study, that microvascular complications could be significantly reduced up to 70% when glycemic goals are within near-normal levels (NIDDK, 2008).
Acute and significant changes in a person’s blood glucose level can cause life-threatening problems. Slow, chronic hyperglycemia is the source of most diabetic illness and death. Longstanding hyperglycemia causes or worsens the following:
- Atherosclerotic arterial disease, leading to hypertension, myocardial infarction, renal vascular insufficiency, and stroke
- Kidney damage (diabetic nephropathy), leading to end-stage renal disease requiring dialysis or kidney transplant
- Eye injury (diabetic retinopathy), with macular edema, retinal hemorrhages, neovascularization, glaucoma, and cataracts, any of which can cause visual impairment or blindness
- Nerve damage (diabetic neuropathy): Peripheral nerve damage leads to injuries of the feet, while autonomic nerve damage weakens bowel/bladder control and/or causes sexual impotence.
- Poor wound healing and a risk for infections, which can lead to limb amputations (Maitra, 2009)
Cardiovascular Damage: Atherosclerosis
The ABCs of Diabetic Care
A—A1c (blood glucose) < 7 percent
B—Blood pressure < 130/80 mm Hg
C—Cholesterol, LDL < 100 mg/dl
Cardiovascular disease is a leading cause of death among all people and 65% of people with diabetes die from heart disease and stroke (NDEP, 2015). Both insulin resistance and the chronic hyperglycemia of type 2 diabetes accelerate the development of atherosclerosis, a disease of large- and medium-size arteries. Atherosclerosis then causes myocardial infarctions, peripheral artery obstructive disease, renal artery disease, and strokes.
Atherosclerosis of a Large Artery

The aorta has been slit lengthwise and laid open to show the extensive atherosclerosis of its walls. White fatty plaque and disrupted lesions cover the inner lining. Source: CDC, 1972.
Atherosclerosis is a major problem in people with diabetes. Atherosclerotic artery disease is a hundred times more likely to cause gangrene of the lower limb in people with diabetes than in people without diabetes. Moreover, atherosclerotic myocardial infarctions are the most common cause of death in people with diabetes (Maitra, 2009). Deaths from cardiovascular disease are 4 times higher in people with diabetes than in other people. An educational focus to reduce illness and cardiovascular disease in people with diabetes is to focus on the ABCs of diabetes, as shown in the box below.
Atherosclerosis is only one of the detrimental cardiovascular consequences of diabetes. For example, people with diabetes tend to have poorer outcomes after ischemic heart injury, and people with diabetes are 2 to 5 times more likely than people without the disease to develop heart failure (Nesto, 2007).
Due to their increased cardiovascular risk, diabetic patients with symptoms suggesting coronary ischemia, especially substernal discomfort brought on by exercise and relieved by rest—should be given an exercise or non-stress ECG. If the test results are abnormal, the patient is referred to a cardiologist.
Management of Cardiovascular Disease
- Diabetic patients who have cardiovascular disease or who have an increased risk for the disease because of their age, family history, a history of smoking, or the presence of hypertension, dyslipidemia, or albuminuria, should be put on an antiplatelet therapy of 81–162 mg/day aspirin.
- Hypertension should be reduced to systolic pressure <130 mm Hg and diastolic pressure <80 mm Hg.
- Preferred medications are ACE inhibitors and angiotensin receptor blockers (ARBs), except in pregnant women.
- Lipid levels should be toward healthy ranges. The primary goal is to reduce LDL cholesterol <100 mg/dl, and statins should be considered.
Source: ADA, 2015.
Test Your Knowledge
Diabetic cardiovascular disease:
- Usually appears as a bleeding disorder in which the patient’s blood clots too slowly.
- Is usually treated with bed rest and a much reduced level of physical activity.
- Is usually the result of atherosclerosis.
- Is uncommon but usually appears as micro hemorrhages in the skin.
Apply Your Knowledge
What pharmaceutical and lifestyle behaviors can help decrease overall cholesterol to recommended levels?
Answer: C
Renal Damage: Nephropathy
In the United States, diabetic kidney damage is the most common cause of end-stage renal disease. This type of kidney damage, diabetic kidney disease (DKD) or diabetic nephropathy, first appears as small amounts of albumin leaking into the urine (microalbuminuria). Without treatment, microalbuminuria progresses to a more significant leakage, macroalbuminuria. Progression from microalbuminuria to macroalbuminuria takes place within 10 to15 years in 20% to 40% of those with type 2 diabetes. Less than ten years afterwards, 20% of patients with macroalbuminuria will develop end-stage renal disease and will need dialysis or a kidney transplant. After myocardial infarction, renal failure is the largest killer of people with diabetes (Maitra, 2009).
Patients with type 2 diabetes should be regularly screened for microalbuminuria, beginning at the time of diagnosis (NKF-KDOQI, 2015). Diabetic retinopathy is often present by the time diabetic kidney disease appears, and albuminuria in a patient with diabetic retinopathy is most likely due to diabetic kidney disease. A serum creatinine level should also be measured yearly as a general assessment of kidney function (ADA, 2015).
Management of Diabetic Kidney Disease
- Improve glycemic control, with a goal of A1c <6.5%; intensive control of hyperglycemia can prevent DKD and may slow the progression of DKD if it already exists.
- Treat hypertension to a goal of <130/80 mm Hg using an ACE inhibitor or an ARB.
- If a patient already has micro- or macroalbuminuria, add an ACE inhibitor or an ARB regardless of the blood pressure (ADA, 2015).
- Reduce blood LDL cholesterol levels to <100 mg/dl and preferably to <70 mg/dl; if medication is needed, a statin is the drug of choice, except in patients on hemodialysis.
- Reduce daily protein intake to 0.8 g/kg of body weight in diabetic patients with chronic kidney disease; this will make proteins approximately 10% of their total daily calories.
- Reduce body weight to within the BMI range of 18.5 to 24.8 kg/m2.
Source: NKF-KDOQI, 2007.
Test Your Knowledge
Diabetic kidney disease is:
- Typically diagnosed by the presence of blood in the urine.
- The most common cause of end-stage renal disease in the United States.
- Typically diagnosed by the presence of glucose in the urine.
- Also called diabetic neuropathy.
Apply Your Knowledge
What foods are included in a low-salt and low-protein diet for someone with chronic kidney disease?
Online Resource
How Does Dialysis Work? [3:17]
https://www.youtube.com/watch?v=fKlY2SKi_dk
Answer: B
Ophthalmic Damage
Diabetes damages the eyes in a number of ways, including diabetic retinopathy, and the onset of cataracts and glaucoma.
Diabetic Retinopathy
Diabetes damages small blood vessels and capillaries throughout the body. Basement membranes are thickened, supportive cells are injured, and the blood vessels in the back of the retina may rupture and leak, exuding fluid and producing tiny hemorrhages. Diabetic retinopathy is a leading cause of new cases of legal blindness among adult Americans (AAO, 2016).
Patchy Vision Induced by Diabetic Retinopathy

The picture on the right simulates the patchy vision that can be produced by diabetic retinopathy. Source: NWS, 2005.
In the retina, micro hemorrhages and fluid leakage first produce macular edema and lipid deposits (hard exudates), both of which can lead to decreased vision. The blood vessel damage also causes reduced perfusion, and this stimulates the second stage of diabetic retinopathy, called proliferative diabetic retinopathy. In proliferative diabetic retinopathy, new blood vessels grow along the surface of the retina, called neovascularization, causing web-like vessels that further disrupt the function of the retina and cause decreased vision (Folberg, 2009).
Cataracts and Glaucoma
Diabetes also increases a patient’s chances of developing cataracts and glaucoma.
Neovascularization of the Retina

A funduscopic view of the optic disc of a person with diabetic retinopathy. Normally, about four large vessels would emerge from the optic disc. Here, a great many extra blood vessels grow across the optic disc and retina. Source: University of Michigan Kellogg Eye Center.
Management of Diabetic Retinopathy
- Chronic hyperglycemia causes rapid development of diabetic eye problems. Glycemic control, with a goal of A1c <6.5%, is a key to reducing the risk and slowing the progression of diabetic retinopathy.
- Hypertension is an additional risk factor, and blood pressure control, with a goal of <130/80, slows the progression of diabetic retinopathy.
- A high serum level of lipids makes a person with diabetes more likely to develop diabetic retinopathy. Serum LDL cholesterol should be reduced to <100 mg/dl and serum triglycerides should be reduced to <150 mg/dl.
- People with type 2 diabetes should have an initial dilated and comprehensive eye examination by an ophthalmologist or optometrist shortly after the diagnosis of diabetes and annually.
- Patients with any degree of diabetic retinopathy should be referred to a specialized ophthalmologist, who may treat high-risk diabetic retinopathy with laser coagulation therapy.
Source: AAO, 2015.
Test Your Knowledge
Diabetic retinopathy:
- Can cause edema of the macular area of the retina as well as the ingrowth of excess blood vessels.
- Is a macrovascular complication of diabetes and results from atherosclerosis of the small retinal blood vessels.
- Is exacerbated by low blood pressure and low blood levels of LDL cholesterol.
- Cannot be treated or slowed and will inevitably lead to blindness.
Apply Your Knowledge
How can a patient with diabetes track all the guidelines of care for themselves?
Online Resource
National Eye Institute Diabetic Eye Disease Resources: Facts About Diabetes Eye Disease
Answer: A
Nerve Damage: Neuropathy
Diabetes damages the nervous system. The most common problem in people with type 2 diabetes is a symmetric peripheral neuropathy in which patients become less able to feel things with their hands and feet. Diabetic nerve damage begins at the tips of the longest nerves and slowly progresses to shorter and shorter nerves; therefore, sensation is first lost in the toes, then in the ankles, and later in the fingers (Anthony et al., 2009).
People with diabetes who have decreased sensation in their feet can be unaware of foot injuries and tend to suffer injuries that cannot heal without special care. To make matters worse, people with diabetes often have reduced circulation in their feet along with generalized poor wound healing. These conditions cause gangrene of the extremities 100 times as often as people without the disease.
Diabetic neuropathy is not limited to peripheral sensorimotor nerves. Autonomic nerves throughout the body can be damaged by chronic hyperglycemia and cause diabetic autonomic neuropathy, which affects organs involved with autonomic functions. Patients with diabetic autonomic neuropathy can have postural hypotension, incomplete bladder emptying, or sexual dysfunction. Specific symptoms of diabetic autonomic neuropathy include:
- A resting tachycardia of >100 bpm
- Orthostatic hypotension, in which systolic pressure falls >20 mm Hg when the patient stands from a sitting position
- Gastroparesis, in which the stomach empties slowly or not at all
- Constipation, or constipation alternating with diarrhea
- Incomplete bladder emptying, which can cause recurrent urinary tract infections
- Erectile dysfunction
- Poor vision at night
- Asymptomatic heart attack
Management of Diabetic Neuropathy
Patients with type 2 diabetes should annually have their feet and hands tested for sensitivity to pain, temperature, light touch, vibration, and proprioception.
Peripheral neuropathy should be explained to patients so they will take special care to guard against injuries. Glycemic control should be improved to a level of A1c <6.5%. Currently, there are no cures for diabetic neuropathy, but symptoms can be treated. For instance:
For pain
Tricyclic drugs, anticonvulsants, serotonin/norepinephrine uptake inhibitors, or substance P inhibitors
For gastroparesis
Diet change or prokinetic drugs (eg, metoclopramide, erythromycin)
For erectile dysfunction
Phosphodiesterase type 5 inhibitors (eg, sildenafil), intraurethral prostaglandins, or physical erection aids
Source: Ferrante, 2007; ADA, 2015.
Test Your Knowledge
Autonomic diabetic neuropathy:
- Leads to difficulty sensing pain in the feet.
- Is the cause of diabetic Alzheimer’s disease.
- Is a psychological result of depression.
- Can cause a variety of symptoms, such as postural hypotension, incomplete bladder emptying, and sexual dysfunction.
Apply Your Knowledge
How would you explain diabetic peripheral and autonomic neuropathy to a patient with diabetes?
Online Resource
National Institute of Diabetes and Digestive and Kidney Diseases website:
Answer: D
Foot Damage
Normal daily activities are especially hard on feet and ankles, which support all of the body weight. In diabetes, feet and ankles lose sensation before other parts of the body. The loss of sensation means that people with diabetes lose the ability to adjust to changes in temperature, pressure, and position; therefore, they tend to injure and re-injure their feet and ankles more frequently and more severely than people without diabetes (ADA, 2012).
Lower Extremity Disease over Age 40
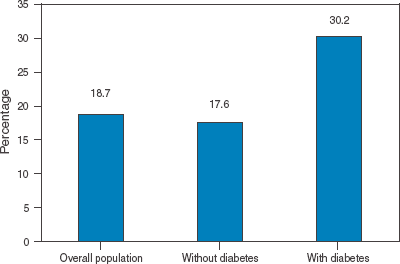
Percent of Americans ≥40 years old with lower extremity disease (ie, peripheral artery disease, peripheral neuropathy, foot ulcers, or lower extremity amputation). Lower extremity disease is almost twice as common in people with diabetes as in those without diabetes. Source: CDC.
As a further complication, people with diabetes have poorer perfusion of peripheral tissues than people without the disease.
Impaired Peripheral Perfusion in Diabetic Foot
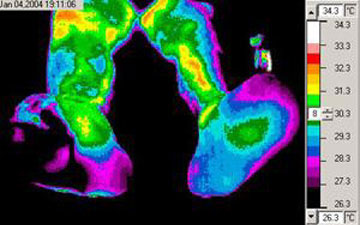
Thermal imaging (heat-sensitive photography) shows that this patient’s left foot is much cooler (the black regions) than the rest of his body, due to decreased peripheral circulation. (The patient is sitting and facing us.)
Source: NASA, 2009.
Wounds and skin infections heal poorly in persons with diabetes. In the United States, diabetes is the leading nontraumatic cause of lower limb amputations (Lipsky et al., 2004).
Management of Diabetic Foot Problems
Patients need annual foot exams, preferably by a diabetic foot specialist. The exam should:
- Inspect skin for abrasions, ulcers, nail infections, or calluses with underlying hemorrhage or discoloration.
- Look for tender areas, swelling, or deformities, such as contractures, joint hyperextension, flexures, and midfoot arthropathy (Charcot arthropathy)
- Test for sensory deficiencies using a tuning fork and a standard 10-g nylon monofilament.
- Test the ankle (Achilles tendon) reflex.
- Assess the perfusion of the foot, checking foot temperature, capillary refill in the toes, and strength of the foot pulses.
- Check shoes, because rubbing and inappropriate pressure points are common causes of foot ulcers.
Patients should be taught not to rely on sensation only, and they should examine their feet daily. They should choose their footwear carefully, keep their nails trimmed, and walk, run, and climb with extra caution.
Patients should be counseled to stop smoking.
Refer patients to foot care specialists for ongoing preventive care and life-long surveillance.
Teach patients with diabetes how to clean and care for their feet.
Source: Lipsky et al., 2004; Boulton et al., 2008; ADA, 2015.
Test Your Knowledge
Foot injuries in patients with diabetes:
- Usually become gangrenous and lead to amputations.
- Receive undue attention and are no more common than foot injuries in people without diabetes.
- Are typically worsened by the increased peripheral circulation that results from hyperglycemia.
- Can heal poorly and are more prone to infection than injuries in people without diabetes.
Apply Your Knowledge
How would you teach a patient with diabetes to check the bottom of their feet when they are obese and can’t see their feet?
Answer: D
Integumentary Damage: Wounds and Infections
Poorly Healing Leg Ulcer in Patient with Previous Amputation

Source: NIDDK, 2007.
Infections are the cause of 5% of the deaths of patients with diabetes, who are especially prone to skin infections, pneumonia, and pyelonephritis. This heightened susceptibility to infection results from a number of factors (Maitra, 2009):
- Sluggish neutrophils with decreases in: chemotaxis, adherence to the endothelium, phagocytosis, and microbiocidal activity
- Decreased production of cytokines by macrophages
- Diminished or impaired local circulation, reducing delivery of oxygen, immune cells, and immune molecules to wounds
- Neuropathy, leading to unawareness of minor injuries
- Patient limitations, such as reduced vision
Management of Diabetic Wounds and Infections
Prevention is the best “treatment” for diabetic infections. Patients should be taught about their neuropathies, how to daily inspect feet, how to purchase protective footwear, and how to care for their feet. They should also be taught that optimal glycemic control reduces their susceptibility to infections.
Wounds and injuries should be reported to a member of the patient’s diabetes team, and the clinician should then:
- Consult a surgeon for severe wounds.
- Clean and debride the wound.
- Take a culture specimen.
- Start antimicrobials if the wound appears clinically infected. Aerobic gram-positive cocci (typically Staphylococcus aureus or beta-hemolytic streptococci) are the most common skin pathogens, but chronic wounds tend to have mixed infections that include gram-positive and gram-negative aerobes and anaerobes.
- Initiate a diabetic wound care regimen.
- Reassess progress daily for inpatients or in 2 to 5 days for outpatients.
With good care, mild to moderate infections should resolve in 80% to 90% of cases. Severe infections will resolve in 60% to 80% of cases.
Source: Lipsky et al., 2004; Baranoski & Ayello, 2008.
Test Your Knowledge
When caring for a wound in a person with diabetes:
- Antimicrobial drugs should be begun if the wound looks infected, even before culture results are available to identify the microbes.
- You should prepare the patient by warning them that most severe wounds will not heal.
- Hospitalization and a surgical consult are mandatory for almost all wounds.
- Contrary to wounds in healthier people, cleaning and debriding a diabetic wound increases the risk of infection.
Apply Your Knowledge
What products are available for wound care in PWD?
Online Resource
Diabetic Foot Care [5:26]
https://www.youtube.com/watch?v=yb1_E9cjV7M
Answer: A
Reproductive Damage: Male and Female
Chronic hyperglycemia impacts every body system, including the reproductive system. Reproductive health problems for men with diabetes include:
- Erectile dysfunction
- Androgen/testosterone deficiency
- Low libido (sexual desire)
- Retrograde ejaculation (semen flows back into the bladder)
- Balanitis (inflammation of the head of the penis)
Because normal erection depends on the ability of blood vessels to constrict correctly and respond neurologically, men with diabetes who have peripheral vascular disease and neuropathy are at risk for erectile dysfunction. Men with diabetes are three times more likely to have erectile dysfunction than men without diabetes.
Reproductive health problems for women with diabetes include:
- Low libido
- Gestational diabetes
- Fertility problems
- Menstrual irregularities
- Delayed menarche and early menopause
- Vaginal dryness and painful intercourse
- Absent orgasm (as many as 35% of women) (Zarzycki & Zieniewicz, 2005)
Assessment of sexual health needs to evaluated by clinicians and the diabetes team as this impacts quality of life. Careful and tactful questions can be asked, such as “Many people with diabetes have problems with sexual intimacy. How has it been for you? Do you have any concerns you’d like to discuss?” Referrals to psychologists for mental health issues that impact sexual relations may be appropriate. Medications such as tricyclic antidepressants may be needed to resolve sexual issues if the etiology is not physical. Support groups and resources should also be provided, and many are available online for use in the privacy of home.
Because the reproductive system in men involves the urinary tract system, urologic complications need to be assessed.
Psychological Damage: Depression
If you’re tired of just reading about diabetes, imagine having to live with the chronic disease and not ever getting a break from it. Like any chronic disease, diabetes can last a lifetime and requires daily attention, which is exhausting. Diabetes burnout, stress, depression, denial, anxiety, and even anger are all issues that impact mental health for people with diabetes.
Assessment questions should be asked by the diabetes healthcare team to recognize and assess concerns and mental health disorders. Questions that are open ended and nonjudgmental can help patients feel free to discuss real concerns, such as “Many people with diabetes can feel sad or angry or have problems eating. How has it been for you?”
Studies show a relationship between new diagnosis of diabetes and depression. The mentally ill are also at a high risk of developing T2DM due to poor health maintenance, which can complicate blood glucose control and their mental illness. Referrals to advanced prepared psychologists and counseling may be needed. Support groups, online forums, and group education classes can be helpful resources.
