Diagnosing Prediabetes
By identifying patients with prediabetes, it is possible to intervene to prevent diabetes and its complications and improve future health. Prediabetes is diagnosed by the same blood sugar screening lab tests as diabetes. The person’s blood sugar levels will show a higher BG than the normal range but below full diabetes, which is between 100 and 125 mg/dL. It is estimated 86 million Americans over age 20 have prediabetes, which is 1 out of every 3 adults (FDA, 2015).
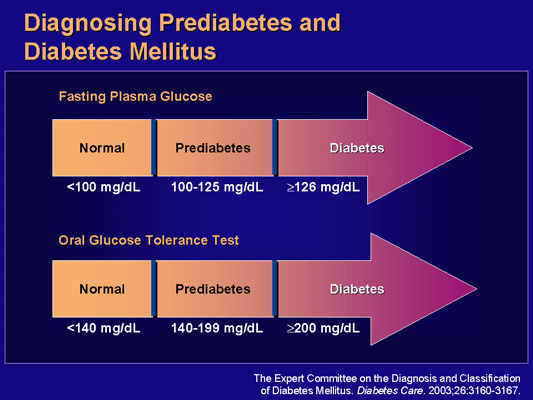
Prediabetes may not manifest with acute symptoms and is mainly detected by blood glucose screening tests. Any of four criteria can be used to diagnose prediabetes: impaired fasting glucose BG > 100–125 mg/dL, impaired glucose tolerance >140–199 mg/dL, A1c >5.7%, <6.5% and positive screening of three abnormalities that qualify as metabolic syndrome:
- Impaired fasting glucose, which is a fasting plasma glucose level between normal and diabetes
- Impaired glucose tolerance, which is an oral glucose-tolerance test result between normal and diabetes
- Presence of three of the five disorders of metabolic syndrome
The chance that a person with prediabetes will progress to type 2 diabetes is high. A person without prediabetes has about a 5% chance of developing diabetes in six years. In contrast, a person with an FPG and an OGTT in the prediabetes range has about a 65% of developing diabetes in six years (Garber et al., 2008).
Managing Prediabetes
The goals of treating prediabetes are to slow its progression into type 2 diabetes and to reduce the person’s chance of developing cardiovascular disease or microvascular complications (retinopathy, nephropathy, and neuropathy) (Garber et al., 2008).
Step one in treating prediabetes is intensive lifestyle management. Without lifestyle changes, 15% to 30% of people with prediabetes will progress to type 2 diabetes within five years (CDC, 2015). The same principles and education are used to treat diabetes.
The first recommendation is weight loss: a weight loss goal of 5% to 10% to be achieved by reducing the person’s intake of calories and increasing the person’s physical activity. Weight loss medications have often been given to help reach this goal; however, the FDA strongly cautions patients about many such pharmaceuticals. Because lifestyle modification and healthy living behaviors can be difficult to maintain for many people, most of them progress to needing pharmacologic assistance for weight loss and lowering BG.
The following cautions are included on weight-loss drugs for prediabetes and T2DM:
- Sibutramine (Meridia). In October 2010 the FDA recommended against further use of this drug, as it is associated with unnecessary cardiovascular risks to patients. The manufacturer (Abbott) voluntarily agreed to stop marketing in the United States.
- Orlistat (Alli, Xenical). In May 2010 the FDA approved a revised label for this drug to include rare but severe liver injury in some people. Some cases have resulted in liver transplant or death. Research shows it reduced the incidence of diabetes by almost 40% in obese people (Torgerson et al., 2004).
- Qsymia (extended-release combination of naltrexone and bupropion). Among other side effects, the manufacturer reports increased incidence of metabolic acidosis and hypoglycemia in diabetic patients who take medication to control hyperglycemia, making it a less than ideal agent for this population.
- Belviq (lorcaserin). The drug has potential for addiction, and may cause heart valve and mental problems and low blood sugar.
Step two in treating prediabetes is anti-diabetic drug therapy, especially for patients at high risk for developing diabetes complications. High-risk patients include those with metabolic syndrome, current cardiovascular disease, progressively worsening hyperglycemia, nonalcoholic fatty liver disease, a history of gestational diabetes, or polycystic ovary syndrome. Metformin has been approved for the treatment of prediabetes by the FDA and is a top tier medication after lifestyle behavior modification, which should include exercise and meal planning education. Acarbose has also been shown to reduce the risk of coronary heart disease and promote weight loss. Other pharmaceutical agents, including amylin analogues and incretin mimetics, have joined the arsenal for physicians to use for people with prediabetes.
People with prediabetes are given the same health coaching and guidance as those with diabetes, and management is focused on behavioral change for healthy lifestyles. Patients with prediabetes should also be treated to reach the same lipid and blood pressure goals as patients with diabetes.
Test Your Knowledge
Prediabetes:
- Is diagnosed when the fasting blood glucose level is >126 mg/dl.
- Usually precedes type 2 diabetes.
- Presents with the same triad of symptoms as diabetes.
- Is not a threat to patients and need not be treated.
Apply Your Knowledge
What national and state health programs are available to help decrease the rising incidence of prediabetes?
Answer: B
Diagnosis of Metabolic Syndrome
Metabolic syndrome is a group of risk factors that raise your risk of heart disease, diabetes, and stroke. The term metabolic refers to the biochemical processes of a body that is functioning normally. Metabolic syndrome identifies a person as having dysfunctional metabolic processes that put the person at risk for comorbidities. The American Heart Association (AHA) and National Heart, Lung, and Blood Institute (NHLBI) identify metabolic syndrome if there are any three of these five criteria:
- Waist circumference
Large waistline (>40 inches in men; >30 inches in women)- For people of non-Asian origin
>102 cm in men or >88 cm in women - For people of Asian origin
>90 cm in men or >80 cm in women
- For people of non-Asian origin
- High triglycerides
>150 mg/dl or on medicines for high triglycerides - Low HDL cholesterol
<40 mg/dl for men, <50 mg/dl for women, or on medicines for low HDL cholesterol - High fasting blood glucose
>100 mg/dl or diagnosed with diabetes or prediabetes - Blood pressure
>130 mm Hg systolic or >85 diastolic or on medicines for hypertension
Managing Metabolic Syndrome
Heart disease is the most common cause of death for people with metabolic syndrome and type 2 diabetes, and the reduction of cardiovascular risk is a top priority. A number of interrelated disorders significantly increase anyone’s chance of developing cardiovascular diseases, with the resulting possibility of myocardial infarction or stroke. These disorders include:
- Central (intra-abdominal or visceral) obesity
- Insulin resistance, type 2 diabetes, or hyperglycemia
- Dyslipidemias (high blood levels of triglycerides, high blood levels of small dense LDL cholesterol particles, and low blood levels of HDL cholesterol)
- Hypertension
While a person can have any one of these problems, each of these cardiometabolic disorders promotes and worsens the others. For example, insulin resistance can lead to hyperlipidemia and hypertension; hypertension increases the likelihood of developing diabetes; and central obesity can lead to insulin resistance and diabetes. People tend to have more than one of these disorders at a time (Buse et al., 2008). Treatment of the metabolic syndrome involves the separate treatment of each of its components, such as diet, exercise, and weight loss, which collectively impact each other.
Test Your Knowledge
Metabolic syndrome is:
- An autoimmune disease.
- No longer accepted as a medical term.
- A cluster of components that must be treated individually.
- A single disorder that puts a person at risk for psoriasis.
Apply Your Knowledge
How can you teach your patients about the lifestyle changes to decrease metabolic syndrome?
Answer: C
