As in any disease, there are modifiable and non-modifiable risk factors that cause the disease. Genetics, gender, ethnicity, and age are all noncontrollable. People with type 1 diabetes who have a genetic predisposition to a heightened and destructive autoimmune response cannot control it. People who are over 65 and of African American descent are at greater risk for developing type 2 diabetes, but cannot control those factors. Following a brief discussion of genetics we want to focus on the controllable risk factors that we can modify to prevent diabetes.
Genetic Factors
Genetics is like being handed a loaded pistol, but the lifestyle behaviors of obesity, overeating, sedentary lifestyle, and so on are what pull the trigger. It has been said 90% of all chronic diseases can be triggered or prevented by lifestyle choices, especially diet and exercise. A person’s genome is a strong determinant of the chance of developing type 2 diabetes. For example, if a dizygotic (fraternal) twin develops type 2 diabetes, the chances are about 25% that the other twin will also develop the disease. The disease risk doubles if the twins are monozygotic (identical): if a monozygotic twin develops type 2 diabetes, the chances are about 50% that the other twin will also develop the disease (Maitra, 2009). People with these genetic predispositions, however, do not always develop clinical diabetes.
It appears that, to develop type 2 diabetes, other health problems must intervene to activate or worsen the insulin resistance and beta cell dysfunction (Maitra, 2009). People with a genetic predisposition may be able to prevent the full development of the disease by health-promoting lifestyle behaviors that prevent overweight and obesity.
Type 2 diabetes is polygenic, meaning that it usually involves the expression of more than one problematic gene. More than twenty variant genes have been documented as potential contributors to the development of type 2 diabetes, and the problematic genes are found on a number of chromosomes. There is no single combination of genes that leads to type 2 diabetes. Instead, the expressions of a variety of combinations of problematic genes may create full development of type 2 diabetes.
“Accumulating data suggest that type 2 diabetes is likely a collection of many closely related diseases with varying but often overlapping primary mechanisms that involve both impaired insulin secretion and insulin resistance” (Grant et al., 2009).
Test Your Knowledge
Type 2 diabetes:
- Is an inevitable disease of aging.
- Is inevitable in people whose families have the disease.
- May develop in genetically predisposed people with additional risk factors.
- Is usually caused by the mutation of a single gene called T2D.
Apply Your Knowledge
Your patient wants to know why he developed type 2 diabetes. What risk factors would you review?
Answer: C
Controllable Risk Factors
Certain health problems are closely associated with the development of type 2 diabetes. These health problems are neither absolute nor independent causes of the disease; that is, not all people with these problems develop type 2 diabetes. Nonetheless, they are major risk factors because they help to initiate or to worsen type 2 diabetes in people with the predisposition for it.
Major risk factors for type 2 diabetes include obesity, physical inactivity, unhealthy diet, hyperglycemia, stress, and chronic inflammation.
Obesity
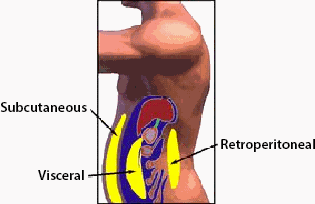
Fat that is inside the abdomen—visceral or intra-abdominal fat—differs metabolically from subcutaneous fat. Intra-abdominal fat is a risk factor for type 2 diabetes. A person’s waist circumference is a good indicator of the amount of fat inside the person’s abdomen (NHLBI, 2015).
Excess body fat causes insulin resistance, and the risk for developing type 2 diabetes increases as the proportion of body fat increases. Body mass index (BMI) is used to measure the proportion of body fat to total body weight. The risk is higher when excess fat has accumulated inside the abdominal cavity, as opposed to under the skin. Excess intra-abdominal fat is a feature of more than 4 out of 5 patients with type 2 diabetes.
Adipose tissue encourages insulin resistance in a number of ways. Excess fat, especially visceral fat, leads to higher blood levels of fatty acids, and fatty acids reduce glucose uptake, causing insulin resistance in skeletal muscle. Additionally, in obese individuals, adipose tissue releases less adiponectin, a hormone that reduces insulin resistance. Excess adipose tissue also secretes additional pro-inflammatory molecules (cytokines), which increase insulin resistance. The increased insulin resistance from all these causes leads to hyperinsulinemia, which further weakens dysfunctional beta cells (ADA, 2015).
Test Your Knowledge
A health problem that directly increases the risk of developing type 2 diabetes is:
- Intra-abdominal fat.
- Periodontal disease.
- Foot injuries.
- Osteoporosis.
Apply Your Knowledge
What is the first behavior modification you should focus on for most people with type 2 diabetes?
Answer: A
Change in Prevalence of Obesity (by BMI) 2005–2010
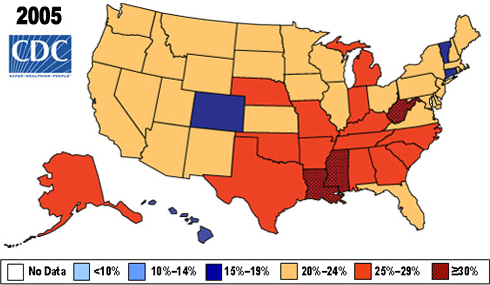
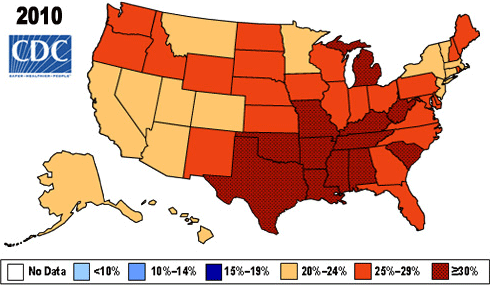
Source: CDC.
Physical Inactivity
Physical inactivity is another major risk factor for the development of type 2 diabetes. In part, this results from the tendency of sedentary people to accumulate triglycerides in their muscle cells and gain weight.
Physical exercise is a powerful counterforce to insulin resistance. Regular exercise improves glycemic control and reduces the risk of developing cardiovascular complications in people with type 2 diabetes. “Furthermore, regular exercise may prevent type 2 diabetes in high-risk individuals” (ADA, 2015).
Poor Diet
Any dietary habits that lead to obesity also increase a person’s chances of progressing from prediabetes to diabetes.
- A high-carbohydrate diet challenges the glucose-lowering ability of a person with prediabetes and accelerates the development of type 2 diabetes.
- A high-fat, low-fiber diet, especially one that includes saturated and trans fats, causes dyslipidemias, which worsen insulin resistance and foster the development of type 2 diabetes.
Hyperglycemia
A controllable risk factor of diabetes mellitus is progressive hyperglycemic states that can be caused by frequent high-carbohydrate consumption. Skeletal muscle and adipose tissue that become overloaded with glucose are less able to take up more glucose, thus hyperglycemia contributes to insulin resistance, prediabetes, and eventually diabetes (Buse et al., 2008).
Stress
Stress activates the sympathetic autonomic nervous system in the “fight or flight” reaction. Cortisol, known as the stress hormone from the adrenals, increases and acts as a counter-regulatory hormone to insulin. Cortisol elevates BG levels in an attempt to deliver glucose to muscle cells so as to fight the stressor. Chronic stress leads to chronic hyperglycemia, which in turn increases insulin resistance and triggers type 2 diabetes in predisposed people.
Chronic Inflammation
Type 2 diabetes alters the functioning of the immune system. Together, insulin resistance, hyperglycemia, and hyperinsulinemia create a persistent inflammatory reaction. At the same time, a chronic inflammatory state leads to chronic hyperglycemia, which then contributes to the progression of type 2 diabetes (O’Connor et al., 2006).
People who are in a constant state of emotional and physical stress are continually in a mild state of inflammation. Their blood shows persistent elevations of molecules of inflammation, such as C-reactive protein and interleukin-6. The pro-inflammatory cytokines causer an elevation in the level of adrenocorticotropic hormone (ACTH), which is the direct stimulant of cortisol secretion. Inflammation increases the level of blood glucose, causing hyperglycemia and eventual insulin resistance. Foods, injury, stress, and other disease processes can all create chronic inflammation.
