The most critical aspect of pain assessment is that it be done on a regular basis using a standard format. Pain should be re-assessed after each intervention to evaluate its effect and determine whether an intervention should be modified. The time frame for re-assessment should be directed by the needs of the patient and the hospital or unit policies and procedures.
A self-report by the patient has traditionally been the mainstay of pain assessment, although family caregivers can be used as proxies for patient reports, especially in situations in which communication barriers exist, such as cognitive impairment or language barriers. Family members who act as proxies typically report higher levels of pain than patient self-reports.
Both physiologic and behavioral responses can indicate the presence of pain and should be noted as part of a comprehensive assessment, particularly following surgery. Physiologic responses include tachycardia, increased respiratory rate, and hypertension. Behavioral responses include splinting, grimacing, moaning or grunting, distorted posture, and reluctance to move. A lack of physiologic responses or an absence of behaviors indicating pain may not mean there is an absence of pain.
Good documentation improves communication among clinicians about the current status of the patient’s pain and responses to the plan of care. Documentation is also used as a means of monitoring the quality of pain management within the institution.
In the absence of an objective measure, pain is a subjective individual experience. How we respond to pain is related to genetic features as well as cognitive, motivational, emotional, and psychological states. Pain response is also related to gender, experiences and memories of pain, cultural and social influences, and general health (Sessle, 2012).
Pain Assessment Tools
Selecting a pain assessment tool should be, when possible, a collaborative decision between patient and provider to ensure that the patient is familiar with the tool. If the clinician selects the tool, consideration should be given to the patient’s age; physical, emotional, and cognitive status; and personal preferences. Patients who are alert but unable to talk may be able to point to a number or a face to report their pain (AHRQ, 2008).
Pain Scales
Many pain intensity measures have been developed and validated. Most measure only one aspect of pain (ie, pain intensity) and most use a numeric rating. Some tools measure both pain intensity and pain unpleasantness and use a sliding scale that allows the patient to identify small differences in intensity. The following illustrations show some commonly used pain scales.
Visual Analog Scale
The Visual Analog Scale. The left endpoint corresponds to “no pain” and the right endpoint (100) is defined as “pain as
intense as it can be.”
†A 10-cm baseline is recommended for VAS scales.
Source: Adapted from Acute Pain Management Guideline Panel,
1992 (AHCPR, 1994). Public domain.
Numeric Rating Scale
The Numeric Rating Scale. Indicated for adults and children (>9 years old) in all patient care settings in which patients are able to use numbers to rate the intensity of their pain. The NRS consists of a straight horizontal line numbered at equal intervals from 0 to 10 with anchor words of “no pain,” “moderate pain,” and “worst pain.” Source: Adapted from Acute Pain Management Guideline Panel, 1992 (AHCPR, 1994). Public domain.
The Pain Scale for Professionals
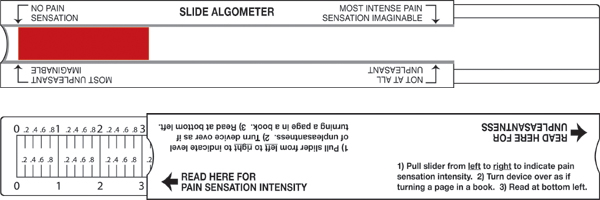
The Pain Scale for Professionals. The patient slides the middle part of the device to the right and left and views the amount of red as a measure of pain sensation. The arrow at the left means “no pain sensation” and the arrow at the right indicates the “most intense pain sensation imaginable.” The sliding part of the device is moved on a different axis for the unpleasantness scale. The arrow at the left means “not at all unpleasant” and the arrow at the right represents pain that is the “most unpleasant imaginable.” Source: The Risk Communication Institute. Used with permission.
Simpler tools such as the verbal rating scale (VRS) classify pain as mild, moderate, or severe. Some studies indicate that older adults prefer to characterize their pain using the VRS. The description can be translated to a number for charting (see following table) and works particularly well if everyone on the unit uses the same scale.
|
Verbal Rating Scale (VRS) |
|
|---|---|
|
Description |
Points Assigned |
|
No pain |
0 |
|
Mild pain |
2 |
|
Moderate |
5 |
|
Severe |
10 |
For patients with limited cognitive ability, scales with drawings or pictures, such as the Wong-Baker FACES™ scale, are useful. Patients with advanced dementia may require behavioral observation to determine the presence of pain.
Wong-Baker FACES™ Pain Rating Scale
The Wong-Baker FACES scale is especially useful for those who cannot read English and for pediatric patients. Source: Copyright 1983, Wong-Baker FACES™ Foundation, www.WongBakerFACES.org. Used with permission.
Pain Questionnaires
Pain questionnaires typically contain verbal descriptors that help patients distinguish different kinds of pain. One example, the McGill Pain Questionnaire asks patients to describe subjective psychological feelings of pain. Pain descriptors such as pulsing, shooting, stabbing, burning, grueling, radiating, and agonizing (and more than seventy other descriptors) are grouped together to convey a patient’s pain response (Srouji et al., 2010).
The questionnaire combines a list of questions about the nature and frequency of pain with a body-map diagram to pinpoint its location. It uses word lists separated into four classes (sensory, affective, evaluative, and miscellaneous) to assess the total pain experience. After patients are finished rating their pain words, a numerical score is calculated, called the “Pain Rating Index.” Scores vary from 0 to 78, with the higher score indicating greater pain (Srouji et al., 2010).
The Brief Pain Inventory (BPI), developed by the World Health Organization, also uses the questionnaire format to measure pain. The ability to resume activity, maintain a positive affect or mood, and sleep are relevant functions for patients. The BPI uses a numeric rating scale to assess difficulties with walking, general activity, mood, and sleep.
Assessing Pain in Children
Despite decades of research and the availability of effective analgesic approaches, many children continue to experience moderate to severe pain, especially after hospitalization. Overall, the factors affecting children’s pain management are influenced by cooperation (nurses, doctors, parents, children), child (behavior, diagnosis, age), organization (lack of routine instructions for pain relief, lack of time, lack of pain clinics), and nurses (experience, knowledge, attitude) (Aziznejadroshan et al., 2016).
Pain evaluation in small children can be difficult. Previous experiences, fear, anxiety, and discomfort may alter pain perception; thus, poor agreement between instruments and raters is often the norm. In children younger than 7 years of age and in cognitively impaired children, evaluation of pain intensity through self-report instruments can be inaccurate due to poor understanding of the instrument and poor capacity to translate the painful experience into verbal language; therefore, complementary observational pain measurements should be used to assess pain intensity (Kolosovas-Machuca et al., 2016).
Three methods are commonly used to measure a child’s pain intensity:
- Self-reporting: what a child is saying.
- Behavioral measures: what a child is doing (motor response, behavioral responses, facial expression, crying, sleep patterns, decreased activity or eating, body postures, and movements).
- Physiologic measures: how the body is reacting (changes in heartrate, blood pressure, oxygen saturation, palmar sweating, respiration, and sometimes neuroendocrine responses (Srouji et al., 2010).
Children’s capability to describe pain increases with age and experience, and changes throughout their developmental stages. Although observed reports of pain and distress provide helpful information, particularly for younger children, they are reliant on the individuals completing the report (Srouji et al., 2010).
Assessing Pain in Cognitively Intact Adults
For the cognitively intact adult, assessment of pain intensity is most often done by using the 0 to 10 numeric rating scale or the 0 to 5 Wong-Baker FACES scale, or the VRS. Once patients know how to use a pain intensity scale, they should establish “comfort-function” goals. With the clinician’s input, patients can determine the pain intensity at which they are easily able to perform necessary activities with the fewest side effects.
In cognitively intact older adults, management of pain begins with an accurate assessment and includes the impact of pain on the patient’s daily activities. When analgesic treatment and pain-modulating drugs are used, co-morbidities and other risk factors must be carefully considered. The least invasive method of administration should be used—in most cases the oral route is preferred (Age and Ageing, 2013).
Assessing Pain in Cognitively Impaired Adults
The assessment of pain in patients with cognitive impairment is a significant challenge. Cognitively impaired patients tend to voice fewer pain complaints but may become agitated or manifest unusual or sudden changes in behavior when they are in pain. Caregivers may have difficulty knowing when these patients are in pain and when they are experiencing pain relief. This makes the patient vulnerable to both undertreatment and overtreatment.
In the absence of accurate self-report, observational tools based on behavioral cues have been developed. The most structured observational tools are based on guidance published by the American Geriatrics Society, which describe six domains for pain assessment in cognitively impaired:
- Facial expression
- Negative vocalization
- Body language
- Changes in activity patterns
- Changes in interpersonal interactions
- Mental status changes (Lichtner et al., 2014)
The interpretation of these behaviors can be complex, due to overlap with other common symptoms such as boredom, hunger, anxiety, depression, or disorientation. This increases the complexity of accurately identifying of pain in patients with dementia and raises questions about the validity of existing instruments. As a result, there is no clear guidance for clinicians and staff on the effective assessment of pain, nor how this should inform treatment and care decision-making (Lichtner et al., 2014).
A large number of systematic reviews have analyzed the relative value and strength of evidence of existing pain tools. In a review of reliability, validity, feasibility, and clinical utility of 28 pain assessment tools used with older adults with dementia, no one tool appeared to be more reliable and valid than the others (Lichtner et al., 2014).
Patient self-report remains the gold standard for pain assessment but in nonverbal older adults the next best option, from a user-centered perspective, becomes the assessment of a person who is most familiar with the patient in everyday life in a hospital or other care setting; this is sometimes referred to as a “silver standard” (Lichtner et al., 2014).
A thorough review of pain assessment tools for nonverbal older adults by Herr, Bursch, and Black of The University of Iowa is available here.
Keeping these challenges in mind, three commonly used behavioral assessment tools serve as examples of those used in assessing pain and evaluating interventions in cognitively impaired adults: the Behavioral Pain Scale, the Pain Assessment Checklist, and the Advanced Dementia Scale.
Behavioral Pain Scale
The Behavioral Pain Scale (BPS) was developed for use with critically ill patients in the ICU. It evaluates and scores three categories of behavior on a 1 to 4 scale:
- Facial expression: 1 for relaxed to 4 for grimacing
- Upper-limb movement: 1 for no movement to 4 for permanently retracted
- Ventilator compliance: 1 for tolerating ventilator to 4 for unable to control ventilation
A cumulative score above 3 may indicate pain is present; the score can be used to evaluate intervention, but cannot be interpreted to mean pain intensity. The patient must be able to respond in all categories of behavior—for example, the BPS should not be used in a patient who is receiving a neuromuscular blocking agent.
Pain Assessment Checklist
Pain behavior checklists differ from pain behavior scales in that they do not evaluate the degree of an observed behavior and do not require a patient to demonstrate all of the behaviors specified, although the patient must be responsive enough to demonstrate some of the behaviors. These checklists are useful in identifying a patient’s “pain signature”—the pain behaviors unique to that individual.
The Pain Assessment Checklist for Seniors with Limited Ability to Communicate (PACSLAC) is a caregiver-administered tool that evaluates sixty behaviors divided into four subscales:
- Facial expressions (13 items)
- Activity/body movements (20 items)
- Social/personality/mood (12 items)
- Physiological indicators/eating and sleeping changes/vocal behaviors (15 items)
A checkmark is made next to any behavior the patient exhibits. The total number of behaviors may be scored but cannot be equated with a pain intensity score. It is unknown if a high score represents more pain than a low score. In other words, a patient who scores 10 out of 60 behaviors does not necessarily have less pain than a patient who scores 20. However, in an individual patient, a change in the total pain score may suggest more or less pain.
Advanced Dementia Scale (PAINAD)
The Pain Assessment in Advanced Dementia Scale (PAINAD) was developed to provide a clinically relevant and easy-to-use observational pain assessment tool for individuals with advanced dementia. The aim of the tool developers was to “develop a tool for measuring pain in non-communicative individuals that would be simple to administer and had a score from 0 to 10” (Herr, et al., 2008). This tool is used when severe dementia is present. This tool involves the assessment of breathing, negative vocalization, facial expression, body language, and consolability.
|
Pain Assessment in Advanced Dementia (PAINAD) |
||||
|---|---|---|---|---|
|
|
0 |
1 |
2 |
Score* |
|
Breathing |
Normal |
|
|
|
|
Negative vocalization |
None |
|
|
|
|
Facial expression |
Smiling or inexpressive |
|
Facial grimacing |
|
|
Body language |
Relaxed |
|
|
|
|
Consolability |
No need to console |
Distracted or reassured by voice or touch |
Unable to console, distract, or reassure |
|
|
PAINAD Scoring: 1-3 = Mild; 4-6 = Moderate; 7-10 = Severe |
Total: |
|||
Assessment of Cancer Pain
Pain assessment in patients with pain secondary to cancer begins with a thorough discussion of the patient’s goals and expectations for pain management, including balancing pain levels and other patient goals, such as mental alertness. Comprehensive pain assessment also includes pain history, pain intensity, quality of pain, and location of pain. For each pain location, the pattern of pain radiation should be assessed (NCI, 2016).
A review of the patient’s current pain management plan and how he or she has responded to treatment is important. This includes how well the current treatment plan addresses breakthrough or episodic pain. A full assessment also reviews previously attempted pain therapies and reasons for discontinuation; other associated symptoms such as sleep difficulties, fatigue, depression, and anxiety; functional impairment; and any relevant laboratory data and diagnostic imaging. A focused physical examination includes clinical observation of pain behaviors, pain location, and functional limitations (NCI, 2016).
Psychosocial and existential factors that can affect pain must also be assessed and treated. Depression and anxiety in particular can strongly influence the pain experience. Across many different types of pain, research has shown the importance of considering a patient’s sense of self-efficacy over their pain: low self-efficacy, or focus on solely pharmacologic solutions, is likely to increase the use of pain medication (NCI, 2016).
Patients who catastrophize pain (eg, patient reports pain higher than 10 on a 10-point scale) are more likely to require higher doses of pain medication than are patients who do not catastrophize. Catastrophizing is strongly associated with low self-efficacy and reliance on chemical coping strategies (NCI, 2016).
A high baseline pain intensity, neuropathic pain, and incident pain are often more difficult to manage. Certain patient characteristics, such as a personal or family history of illicit drug use, alcoholism, smoking, somatization, mental health issues such as depression or anxiety, and cognitive dysfunction are associated with higher pain expression, higher opioid doses, and longer time to achieve pain control (NCI, 2016).
Several risk-assessment tools have been developed to assist clinicians, such as the Edmonton Classification System for Cancer Pain (ECS-CP) and the Cancer Pain Prognostic Scale (CPPS) (NCI, 2016).
Assessing Gender Differences in Pain Sensitivity
Men and women experience and report pain differently. Specifically, women have been shown to have a lower pain threshold and pain tolerance and stronger responses to analgesics than do men. These differences are present in community-dwelling and clinical samples (Ho et al., 2016).
Differing biologic and psychosocial factors may account for gender differences in pain sensitivity. One commonly studied psychosocial factor is pain-related fear, which includes fear of the sensation of pain, fear of movement or re-injury, and fear of physical activities that are assumed to cause pain. Pain-related fear may contribute to the shift from acute low back pain to chronic low back pain, and numerous studies have demonstrated the association of pain-related fear with disability in patients with chronic and acute low back pain, hip and knee osteoarthritis, and foot and ankle dysfunction (Horn et al., 2014).
An experimental pain study using electrical stimuli found the increased pain experienced by women during a movement task was accounted for by higher reports of fear among women compared to men. In addition to pain-related fear, Robinson and colleagues found women to be more willing to report pain and consider themselves to be more sensitive to pain compared to males. Conversely, some males believe that they have higher pain endurance than women and as compared to the typical male (Horn et al., 2014).
Clinically, gender differences are relevant because a greater percentage of chronic pain sufferers are women. Women also generally report more areas of bodily pain and more pain-related disability compared to men (Horn et al., 2014).
Gender bias (an unintended and systematic neglect of one gender) may play a role in a patient’s access to pain rehabilitation services. Swedish researchers found that men more often than women were referred to physiotherapy and x-ray independent of self-reported pain intensity, pain activity, and pain localization. Higher scores on self-reported pain did not trigger referral to rehabilitation. In fact, a negative trend was found among women. The higher the scores of pain, the less likely that women were referred to rehabilitation (Hammarström et al., 2015).
Back Next