Professionals approaching pain management from a non-pharmacologic perspective use diverse techniques to address the needs of their clients. Those trained in the Western medical model are increasingly working in interdisciplinary teams. Within mainstream healthcare, this can include physical and occupational therapists, psychologists, and nurses—all under the direction of a physician.
Interdisciplinary Pain Rehabilitation
Interdisciplinary pain rehabilitation programs are becoming more common, especially for the treatment of chronic pain. In this model, healthcare professionals work from the same facility, with daily meetings about the patients’ progress, sharing the same treatment vision and passing the same message to the patients (Kurklinsky et al., 2016).
In one such program at the Mayo Clinic Comprehensive Pain Rehabilitation Center in Jacksonville, Florida, the goal is to improve function in people with chronic pain. The program provides physical therapy, occupational therapy, a pain psychologist, and a nurse patient-care coordinator.
The physical therapy component focuses on general reconditioning with graded exposure to activity, gradual reduction of fear-avoidance behaviors, and incremental elimination of other pain behaviors. The occupational therapy component focuses on the role of moderation and balance in daily activities. The pain psychologist leads up to three group therapy sessions each day—addressing anger, anxiety, and fear; identifying pain cycles; and discussing behavioral change, pain, and depression. A nurse manages medications and medication tapering and also communicates with primary and specialty care providers outside of the pain team to assist with continuity of care into the future (Kurklinsky et al., 2016).
Physical and Occupational Therapy
As non-drug practitioners, physical and occupational therapists are well positioned to provide education on pain management for patients with acute and chronic pain. Education focuses on assessing and changing habits and patterns of movement that cause pain and dysfunction. Treatment often involves individual or small group sessions, and can include manual therapy, movement analysis, and supportive technologies and equipment. Clients are instructed to mobilize and strengthen muscles and improve patterns of movement, often focusing on restrictions in tendons, joints, and connective tissue.
Therapeutic exercise and proprioceptive training are active treatment techniques designed to address pain, improve strength and range of motion, increase blood flow, improve proprioception,* and prevent muscle guarding, spasms, and contractures. Exercise programs directed by a physical or occupational therapist are tailored to the individual patient, based on assessment of impairments, patient preference, and co-morbidities.
*Proprioception: Our unconscious sensory awareness of balance and equilibrium, our body’s position in space, and the force and direction of movement. Proprioception allows us to control our limbs and move about in the world without having to consciously decide the force and direction of each movement.
Therapeutic exercise is particularly effective for patients with low back pain. It has been shown to decrease pain intensity, alleviate disability, and improve physical functions for up to 12 months following treatment (Ishak et al., 2016).
Proprioceptive training, in which passive and active sensory feedback exercises are used to improve motor function, may be more effective than traditional exercise in the treatment of low back and neck pain. For patients with musculoskeletal conditions such as chronic neck pain, knee ligament reconstruction, ankle injury, and osteoarthritis, training consists of active multi-joint or whole body movement as well as whole body balance training. Proprioceptive training proved most beneficial for improving function in knee osteoarthritis, leading to significant functional improvement (Aman et al., 2015).
Manual Therapy
Manual therapy is a specialized area within many professions, particularly physical therapy, osteopathy, and chiropractic. Manual therapists use a variety of non-surgical techniques directed to the patient’s spine and extremities for the purpose of assessing, diagnosing, and treating various symptoms and conditions. Manual therapy techniques can be categorized into four major groups: (1) manipulation, (2) mobilization, (3) static stretching, and (4) muscle energy techniques. The definition and purpose of manual therapy varies across healthcare professionals (Clar et al., 2014).
Manual therapists mobilize areas of the spine or other painful joints using their hands, forearms, or elbows to apply a force with a therapeutic intent. Spinal manipulation and mobilization are commonly used treatment modalities for back pain, particularly by physical therapists, osteopaths, and chiropractors (Clar et al., 2014).
A 2010 review of scientific evidence on manual therapies for a range of conditions concluded that spinal manipulation or mobilization may be helpful for several conditions in addition to back pain, including migraine and neck-related headaches, neck pain, upper- and lower-extremity joint conditions, and whiplash-associated disorders. The review also identified a number of conditions for which spinal manipulation or mobilization appears not to be helpful (including asthma, hypertension, and menstrual pain) or the evidence is inconclusive (fibromyalgia, mid-back pain, premenstrual syndrome, sciatica, and temporomandibular joint disorders) (NCCIH, 2012).
Other Nondrug Techniques
Other common pain management techniques used to treat and manage pain include electrical stimulation, therapeutic ultrasound, heat/cold therapy, and dry needling. These techniques are widely used by physical and occupational therapists, osteopaths, and chiropractors.
TENS
TENS (Transcutaneous Electrical Nerve Stimulator)
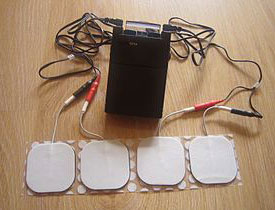
Transcutaneous Electrical Nerve Stimulator. Source: Wikipedia.
Transcutaneous electrical nerve stimulation (TENS) is used to relieve a variety of painful conditions. Controlled clinical trials have demonstrated that TENS can relieve pain, but the mechanism remains largely unknown. For this reason, clinicians use TENS largely by trial and error, and the optimal setting of stimulation parameters is still a matter of debate (Buonocore et al., 2013).
Therapeutic Ultrasound
Therapeutic ultrasound is used for the treatment of soft tissue injuries and pain. It involves the use of ultrasonic sound waves applied directly to a patient’s skin, which causes the underlying tissue to vibrate and mildly heat, improving blood flow to the affected tissue. The thermal effect is thought to cause changes in nerve conduction velocity, increase enzymatic activity, cause changes in contractile activity of skeletal muscles, increase collagen tissue extensibility, increase local blood flow, increase the pain threshold, and reduce muscle spasm (Ebadi et al., 2012).
Non-thermal, mechanical effects are achieved through the application of pulsed, low-intensity ultrasound. In animal studies, pulsed low-intensity therapeutic ultrasound has been used with beneficial effects on cartilage repair (MacIntyre et al., 2013).
Heat/Cold Therapy
The application of heat and cold to reduce pain or promote comfort is a common intervention. However, there are few studies investigating the impact of heat or cold on pain or function. Heat is commonly used to treat pain in combination with other treatments. Thermal agents apply heat either superficially or deeply. Superficial methods include hot packs, warm whirlpools, and paraffin. Deep heat, such as ultrasound, can increase the temperature of the tissues 3 to 5 centimeters in depth. Heat has the advantage of inducing relaxation and decreasing joint stiffness, muscle spasm, and guarding. It assists in increasing range of motion and increases superficial circulation.
Dry Needling
Dry needling is the penetration of a needle through the skin without introduction of any drug (Chou et al., 2012). Dry needling uses a thin, flexible needle to stimulate underlying myofascial trigger points,* muscular, and connective tissues for the management of neuro-musculoskeletal pain and movement impairments. Dry needling is used by physical therapists to treat pain and reduce or restore impairments of body structure and function (APTA, 2013).
*Trigger point: a hyperirritable nodule or knot in the fascia surrounding the muscle.
Although there is strong evidence to support the use of dry needling in the treatment of various neuromuscular pain syndromes, the American Physical Therapy Association and several State Boards of Physical Therapy have narrowed their definition of dry needling to an “intramuscular” procedure. These professional organizations have equated dry needling with the term “intramuscular manual therapy” (IMT) or “trigger point dry needling” (TDN) (Dunning et al., 2014).
Back Next