The ugly reality is that dementia often manifests as a relentless and cruel assault on personhood, comfort, and dignity. It siphons away control over thoughts and actions, control that we take for granted every waking second of every day.
Michael J. Passmore
Geriatric Psychiatrist, University of British Columbia
2.1 Common Types of Dementia
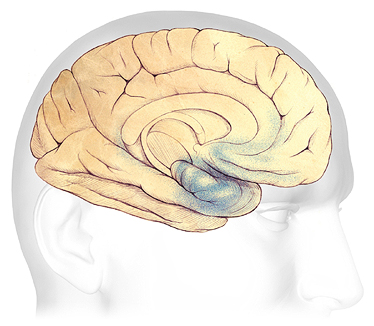
An illustration of the cerebrum, cerebellum, and the brainstem. The outer surface of the cerebrum is made up of a thin layer of nerve cells called the cerebral cortex. ©Zygote Media Group, Inc. Used with permission.
Dementia is a syndrome, a collection or grouping of symptoms—the result of progressive deterioration and loss of brain cells and brain mass. Different types of dementia affect different parts of the brain. Some dementias start in a part of the brain that controls a specific function such as short-term memory or emotion. Other dementias affect the entire brain—or more than one part of the brain—causing other symptoms.
Although a small percentage of people experience early-onset dementia, in general, dementia develops in later adulthood. Aging is a risk factor for developing dementia but nevertheless dementia is not considered a normal part of aging. Determining if someone has dementia is important because some types of cognitive changes can be addressed or even reversed if the underlying cause is identified and treated.
Alzheimer’s disease is the most common cause of dementia, but it isn’t the only cause. Frontal-temporal dementia—which begins in the frontal lobes—is a relatively common type of dementia in those under the age of 60. Vascular dementia and Lewy body dementia are other common types of dementia (see table below). Dementia associated with Parkinson’s disease shares a common etiology with Lewy body dementia.
Some Common Types of Dementia | |||
|---|---|---|---|
Dementia subtype | Characteristic symptoms | Neuropathology | % of cases |
*Alzheimer’s disease (AD) |
|
| 60–80% |
Frontal-temporal dementia |
|
| 5–10%, prevalence thought to be under-estimated |
*Vascular dementia, including post stroke dementia |
|
| 20–30% |
Dementia with Lewy bodies (shares a common etiology with Parkinson’s disease dementia) |
|
| ~5-10% |
Parkinson’s Disease Dementia (shares a common etiology with Lewy body dementia) |
|
|
|
2.1.1 Alzheimer’s Dementia
Alzheimer’s disease (AD) is a progressive, irreversible, age-related brain disorder that affects as many as 5 million Americans over the age of 65. It is the most common type of dementia and is responsible for 60-80% of all cases (ADI, 2019).
Worldwide, more than 50 million people live with dementia and because people are living longer this number is expected to triple by 2050 (ADI, 2019). In Florida, there are 580,000 residents currently living with Alzheimer’s disease. By 2025, this number is expected to increase to more than 720,000 (Alzheimer’s Association, 2023).
Did You Know. . .
For some time now, we have used the term “Alzheimer’s disease and related dementias” to describe dementia and to make it clear that there is more than one kind of dementia. The term neurocognitive disorder is now recognized in the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) as a new term for dementia.
Memory problems are a common early symptom of Alzheimer’s dementia although language difficulties, apathy, depression, and vision and spatial difficulties can also be early symptoms. Although more than twenty types of dementia have been identified, Alzheimer’s dementia is the most frequent (and most studied) cause of dementia in older adults. In general, executive functions are more impaired in Alzheimer’s disease than in other types of dementia.
The exact cause of Alzheimer’s dementia is still unknown. In Alzheimer’s disease, and likely in other forms of dementia, damage within the brain is thought to be due to the formation of beta-amyloid plaques, neurofibrillary tangles, and the degeneration of neurons in the cerebrum.
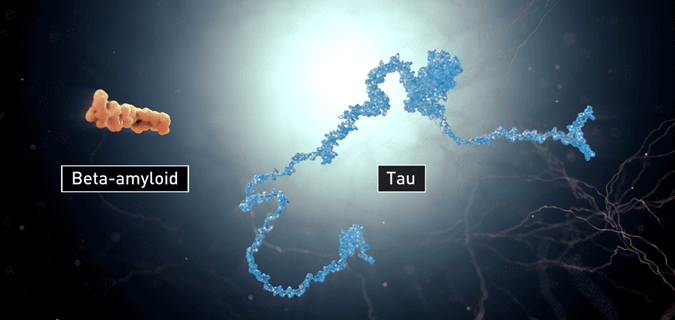
Beta-amyloid plaques and neurofibrillary tangles (tau).
Source: Image courtesy of the National Institute on Aging/National Institutes of Health. Public domain.
Brain imaging techniques such as magnetic resonance imaging (MRIs) as well as autopsies show that Alzheimer’s causes the brain to shrink, that connections between nerves weaken, and nerve cells are damaged and lost. Once a healthy nerve cell begins to deteriorate, it loses its ability to communicate with other neurons, with devastating results.
Degeneration of Cerebral Neurons
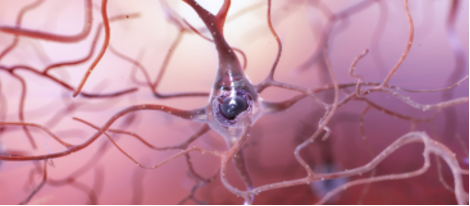

Left: A healthy neuron with many connections to other cells. Right: A dying nerve cell showing the nerve connections weakening and the main body of the cell deteriorating due to the presence of amyloid plaques and tau tangles.
Source: Image courtesy of the National Institute on Aging/National Institutes of Health. Public domain.
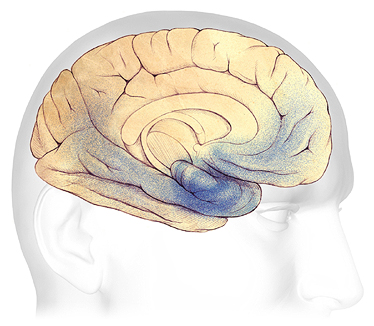
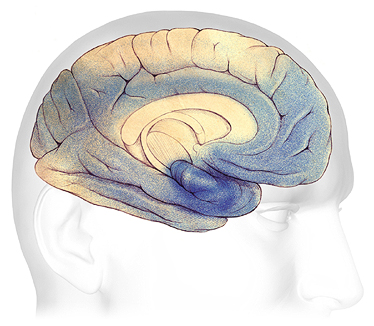
The Progression of Alzheimer’s Disease
A | B | C |
A: Plaques and tangles (shaded in blue) are beginning to form within a part of the temporal lobe called the hippocampus. B: As the disease progresses, damage spreads toward the front and rear of the brain. C: In severe Alzheimer’s, plaques and tangles have caused widespread damage throughout the brain. Source: The Alzheimer’s Association. Used with permission.
In Alzheimer’s disease, plaques and tangles first appear in an area of the temporal lobe called the hippocampus, where new memories are formed (A). As the disease progresses, plaques and tangles spread to the front part of the brain, affecting judgment and other high-level mental functions; symptoms begin to be obvious at this stage (B). In the severe stage (C), plaques and tangles are found throughout the brain. Damage eventually affects memory, emotions, communication, spatial awareness, safety awareness, logical thinking, recognition of loved ones, and the ability to care for oneself.
2.1.2 Vascular Dementia and Vascular Cognitive Impairment
Vascular dementia is one of the most common forms of dementia after Alzheimer’s disease, thought to be the cause of approximately 20–30% of the dementia cases worldwide (ADI, 2019). It usually has a stepwise onset, meaning symptoms can stay the same for a long period of time, then suddenly worsen. Memory may be less affected than in Alzheimer’s disease while fluctuations in mood are more common. Cognitive impairment is often “patchy” because of small vessel damage throughout the brain. Vascular dementia can also affect judgment—but not as strongly as in someone with frontal-temporal dementia.
Diseases or disorders that damage the vessels supplying blood to the brain are risk factors for vascular dementia. This includes hypertension, heart rhythm irregularities, diabetes, high cholesterol, smoking, sleep-disordered breathing, and a sedentary lifestyle (UCSF, 2020). The risk of developing dementia from vascular damage can be significant even when individuals have suffered only small strokes or minor damage to the blood vessels (NINDS, 2023, December 19).
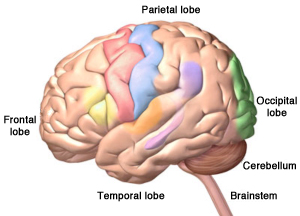
2.1.3 Frontal-temporal Dementia
Frontal-temporal dementia begins in the frontal and temporal lobes of the brain. It is a relatively common type of dementia in people under the age of 60 although new research is showing that it can start in older age. It is thought to be responsible for 5-10% of all cases of dementia. There is no single pathology attributed to frontal-temporal dementia—it is considered a “family” of neurodegenerative disorders.
Behavioral and personality changes associated with frontal-temporal dementia can be striking. This is because the frontal lobes are responsible for many of the traits and behaviors that mediate human behavior. Damage to this part of the brain can lead to mood swings, disinhibition, inappropriate touching, loss of social decorum, and loss of empathy in addition to language difficulties and problems with spatial orientation.
Certain subtypes of frontal-temporal dementia affect judgement, empathy, foresight, and planning. A second subtype affects language skills, reading, writing, and comprehension while a third subtype causes disturbances of motor function and muscle weakness or wasting, without behavioral or language problems (Alzheimer’s Association, 2024).
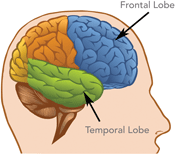

Damage to the brain’s frontal and temporal lobes causes forms of dementia called frontotemporal disorders. On the right, the areas of the brain affected by frontal-temporal dementia are shaded in purple. Left source: National Institute on Aging, public domain. Right source: Alzheimer’s Association, 2020 Used by permission.
Because frontal-temporal dementia can also affect the hippocampus and because of the many variations found in the disease, it is often difficult to tell the difference between frontal-temporal dementia and Alzheimer’s disease. It can also be confused with other psychiatric conditions such as late-onset schizophrenia.
2.1.4 Dementia with Lewy Bodies
Dementia with Lewy bodies (DLB) is another type of progressive dementia. Although DLB is less well-known than Alzheimer’s dementia, it is not rare. DLB is caused by the build-up of abnormal proteins called Lewy bodies inside nerve cells in areas of the brain responsible for certain aspects of memory and motor control. It is not known exactly why Lewy bodies form or how Lewy bodies cause the symptoms of dementia (NINDS, 2024, January 19).
The similarity of symptoms between dementia with Lewy bodies, Parkinson’s disease, and Alzheimer’s disease can make diagnosis difficult. It is possible that either Lewy body dementia is related to these other causes of dementia or that an individual can have more than one type of dementia at the same time. Lewy body dementia usually occurs in people with no known family history of the disease. However, rare familial cases have occasionally been reported (NINDS, 2024, January 19).
Jim's Story
Jim, a 60-year-old executive assistant, began having trouble managing the accounting, paperwork, and other responsibilities of his job. He became increasingly irritable, and his daughter insisted he see a doctor. Jim was diagnosed with depression. He was prescribed an antidepressant, but his thinking and concentration problems worsened. When he could no longer function at work, his doctor diagnosed him with Alzheimer’s disease.
A few months later, Jim developed a tremor in his right hand. He was referred to a neurologist, who finally diagnosed him with dementia with Lewy bodies. Having this diagnosis helped Jim and his daughter plan for the next steps in his treatment and care.
From: National Institutes of Neurological Disorders and Stroke, 2024, January 19.
2.1.5 Parkinson’s Disease Dementia
Although Parkinson’s disease is initially associated with progressive difficulties with movement (slowed movement, postural instability, resting tremors), about 80% of people with Parkinson’s disease will eventually experience behavioral and cognitive changes. Symptoms are mild in the early course of the disease, then progressively worsen. This condition is closely related to Lewy Body dementia—both diseases are caused by the build-up of alpha-synuclein proteins, which clump together, causing damage to nerve cells in the brain.
2.1.6 Post-Stroke Dementia
The risk for cognitive impairment or decline is increased by a history of stroke. As many as two-thirds of stroke patients experience cognitive impairment or cognitive decline following a stroke and approximately one-third go on to develop dementia. The risk for developing dementia may be 10 times greater among individuals with stroke than those without. Mortality rates among stroke patients with dementia are 2 to 6 times greater than among stroke patients without dementia (Teasell et al., 2014).
2.2 Functional Impairments
Cognitive decline and functional changes are intimately related. Changes in vision, hearing, depth perception, reaction time, and gait affect all aspects of daily living. Visual and perceptual changes affect reading, comprehension of form and color, peripheral vision, and the ability to see contrast. Navigating around obstacles such as curbs, breaks in the sidewalk, stairs, and pets becomes more challenging. Because it becomes increasingly difficult to accurately detect motion and process visual information, driving is no longer safe.
Problem solving, self-management, and the ability to focus and pay attention are all affected or altered by dementia. Declines in the ability to think, remember, or reason interfere with a person's daily life and activities. (NINDS, 2023, December 19).
In a Norwegian study, participants living with a diagnosis of dementia reported they became more sensitive to stress, needed more rest in order to concentrate, and felt more fatigue. They reported frustration with increasing forgetfulness and difficulty expressing themselves. Additionally, they reported (Molvik et al., 2024):
- finding it more difficult to orientate themselves to their surroundings
- needing more predictability and more time to prepare for activities
- finding it painful to experience not remembering where they were going
- experiencing “a complete stop in thinking”
Gait variability (changes in stride length and speed) increases from early, mild cognitive impairment throughout all the stages of Alzheimer's disease. Increased gait variability may reflect the progression of cognitive impairment in neurodegenerative diseases, specifically for Alzheimer's disease dementia (Pieruccini-Faria et al., 2021).
Different types and stages of dementia cause different functional impairments. Vascular dementia can affect decision-making and judgment and leads to mood changes. Frontal-temporal dementia causes mood changes, apathy, and disinhibition*, difficulties with language, and weakness or slowing of movement. People with frontal-temporal dementia gradually lose control of their impulses—their behavior is often referred to as “odd,” “socially inappropriate,”, and “schizoid.”
*Disinhibition: a loss of inhibition, a lack of restraint, disregard for social convention, impulsiveness, poor safety awareness, an inability to stop strong responses, desires, or emotions.
Functional impairments associated with dementia with Lewy bodies include progressive cognitive decline, “fluctuations” in alertness and attention, depression, visual hallucinations, and parkinsonian motor symptoms, such as slowness of movement, difficulty walking, or rigidity (stiffness). Dementia with Lewy bodies is also associated with difficulty sleeping, loss of smell, and visual hallucinations (NINDS, 2024, January 19).
Functional impairments associated with Parkinson’s disease dementia include the onset of Parkinson-related movement symptoms followed by mild cognitive impairment and sleep disorders, which involves frequent vivid nightmares and visual hallucinations (NINDS, 2023, December 19). Cognitive issues such as impaired memory, lack of social judgment, language difficulties, and deficits in reasoning can develop over time.
Changes in Vision—Teepa Snow | MedBridge [3:11]
https://www.youtube.com/watch?v=iaUsRa5kNyw