Changes in behavior occur in the vast majority of people with dementia. These changes are referred to as behavioral and psychological symptoms of dementia (BPSD) or neuropsychiatric symptoms of dementia (NSP). More than 90% of people affected with dementia will eventually experience some type of challenging behavior associated with their dementia (Wang et al., 2020).
In some patients, behavioral and psychological symptoms appear before memory deficits develop. The severity of the symptoms can increase with disease progression, affecting the quality of life of both people with dementia and their caregivers. Though memory deficits are the best studied aspects of Alzheimer’s, it is behavioral and psychological symptoms that are often the greatest source of burden for everyone involved (Mao et al., 2020).
Behavioral changes associated with dementia range from mild to severe; symptoms can be constant but usually come and go. They are associated with significant client and caregiver distress, increased rates of institutionalization, and increased mortality (Mao et al., 2020).
Among the many behavioral and psychological symptoms associated with Alzheimer’s disease and other types of dementia, depression*, apathy, agitation, aggression, delusions, and hallucinations are some of the most common. These behavioral changes can lead to wandering, rummaging, hoarding, obsessive-compulsive behaviors, and sleep disturbances.
Common causes of behavioral changes include:
- Brain changes due to dementia.
- Unmet physical needs such as pain, discomfort, or fatigue.
- Boredom, lack of socialization, lack of meaningful activities.
- Frustration due to inability to understand, figure out, or complete a task.
- Cold, heat, noise, uncomfortable chairs, too much or too little light.
*See Module 4: Treatable and Irreversible Dementias for more on depression.
Understanding Needs Driven Behaviors [4:49]
https://www.youtube.com/watch?v=GSpRCUVroGg
Source: Health Services Advisory Group, Inc., 2014.
7.1 Areas of the Brain Related to Behavioral Control
Structural and neurochemical changes in the brain affect a person’s ability to process and act on information. These changes can affect a person’s behavioral control, self-awareness, and their awareness of other people’s emotions. A person’s ability to interpret other people’s emotional cues and social behaviors can also be affected by cognitive changes (UCSF, 2023)
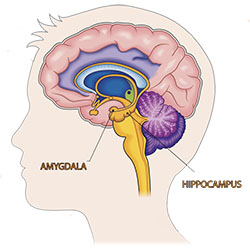
National Institutes of Health, Source: iStock/jambojam. Public domain.
In Alzheimer’s disease, behavioral symptoms may be mainly due to frontal lobe abnormalities. Apathy has also been associated with frontal structures, while delusions have been correlated with frontal, parietal, and temporal structures. Depressive symptoms are thought to be due to damage to deeper brain structures, while agitation has been associated with temporal and frontal structures (Rouch et al., 2014).
Behavioral changes such as anxiety, agitation, depression, fear, and anger have been associated with damage to the amygdala, which is responsible for emotional control and is anatomically linked to the hippocampus.
7.2 Challenging Behaviors Associated with Brain Deterioration
Changes to the brain often, although not always, can lead to a variety of challenging behaviors. Dementia lowers a person’s ability to handle excessive noise, temperature changes, and high levels of commotion often found in public areas. Some of the most common challenging behaviors in people with dementia are apathy, agitation, and aggression, and depending on the type of dementia, delusions and hallucinations. Physical behaviors such as wandering, obsessions, and calling out are often related to a person’s inability to communicate their needs.
7.2.1 Apathy
Apathy is a lack of interest or emotion, loss of motivation, indifference, and a blunting of emotions. It is one of the most common neuropsychiatric features of dementia, affecting 50–70% of people with the condition (Baber et al., 2021).
The presence of apathy in people with Alzheimer’s disease is associated with increased functional impairment, a greater likelihood of rapid functional decline, and a lower self-reported quality of life. It is also associated with poorer performance in basic and instrumental activities of daily living, more rapid disease progression, and increased mortality in people with Alzheimer’s disease (Dolphin et al., 2023).
Apathy is under-recognized, under-diagnosed, and poorly managed. It can be frustrating for caregivers, who often find it frustrating when it appears that the person with dementia is capable of doing a task but simply does not bother or will only do so with strong encouragement (Baber et al., 2021).
Apathy and depression often occur together. In Alzheimer’s disease, apathy is associated with loss of nerve cells and disconnections within specific parts of the brain, including the amygdala. This disconnection within brain circuits suggests that impaired transmission of a key neurotransmitter called acetylcholine* is involved in apathy pathophysiology (Rea et al., 2014).
*Acetylcholine: a neurotransmitter found throughout the body responsible for the contraction of muscles and plays a key role in memory, learning, cognition, attention, arousal, motivation. Depletion of this neurotransmitter is associated with Alzheimer’s disease.
7.2.2 Agitation and Aggression
Agitation and aggression are inappropriate verbal or motor behaviors that occur in more than half of people who have dementia. These behaviors can be caused by pain, physical illness, depression, disorientation, separation from family or other unmet needs (NSW Health, 2022).
One example of an agitated behavior is a “catastrophic reaction”. These are instances when a person suddenly becomes tearful, angry, and abusive. These are usually brief episodes caused by frustration over reduced ability to do simple tasks such as getting dressed, misunderstanding what someone has said or misinterpreting environmental cues. A non-aggressive behavioral response to the same situation might be to stop talking and withdrawal (NSW Health, 2022).
Aggression involves physically or verbally threatening behaviors directed at people, objects, or self. Aggression can include verbal insults, shouting, screaming, obscene language, hitting, punching, kicking, pushing and throwing objects, and sexual aggression (Burns et al., 2012, latest available).
Physiologically, aggression may be related to a decrease in the activity of certain neurotransmitters in the brain, especially serotonin* or acetylcholine. Frontal lobe dysfunction, which occurs in frontal-temporal dementia, may be a factor. Aggression may also be related to underlying depression or psychotic symptoms (Burns et al., 2012).
*Serotonin: a neurotransmitter found throughout the body, helps to regulate mood, appetite, digestion, sleep, memory, and sexual desire. There is thought to be a link between serotonin and depression.
Agitated and aggressive behaviors can also be an attempt to communicate, and can be related to feelings of helplessness, loss of control, discomfort, pain, or fear. Agitation and aggression can be a response to a violation of personal space or a perceived threat and often occur during personal care tasks involving close caregiver-resident contact (Burns et al., 2012).
7.2.3 Delusions and Hallucinations (Psychosis)
Psychosis is a disturbance in the perception or appreciation of objective reality. This can include delusions and hallucinations.
Delusions are false ideas or beliefs or a misinterpretation of a situation. Delusions in people with dementia tend to reflect underlying memory loss or perceptual changes, such as the conviction that other people are stealing money or personal items, that their spouse or caregiver is an imposter, or that their spouse is being unfaithful (NSW Health, 2022).
Hallucinations are sensory events in which a person hears, tastes, smells, sees, or feels something that is not there. Visual hallucinations may be vivid in dementia with Lewy bodies, such as seeing brightly colored crocodiles in the house (NSW Health, 2022).
Auditory hallucinations (“voices”) are less common—their presence may indicate an underlying psychiatric disorder. More commonly, auditory illusions occur when the person misinterprets sounds. For example, discussion amongst the care team may be misinterpreted as plotting to kill people. Hallucinations may also be a side effect of prescribed medications (NSW Health, 2022).
Visual hallucinations have been attributed to decreased blood flow in three regions of the brain: (1) a region responsible for the processing of visual information, (2) an area involved with error detection, and (3) an area involved with inhibitory control of visual information (Heitz et al., 2015).
Delusions and hallucinations have also been associated with changes in the amount and availability of certain neurotransmitters within the brain. Excess dopamine as well as an increase in the number of dopamine receptors has been seen in patients with psychosis compared to people without psychosis. Because dopamine is involved with the regulation of many body functions, too much dopamine can cause hyperactivity, fear, and rage.
Urinary tract infections, poor lighting, sensory overload, and a reaction to a medication can also contribute delusions and hallucinations. In a person with new onset of visual hallucinations, the number one cause is medication side effects. For this reason, a person experiencing visual hallucinations should have all medications carefully reviewed.
7.2.4 Wandering or “Walking About”
Wandering for person with dementia is aimless, repetitive, hyperactive, and excessive movement. It can include wandering outside and becoming lost in the community. Wandering is associated with terms such as “elopement” and “getting lost”.
The desire to move about is often related to boredom, pain, discomfort, or disorientation. Wandering is more common in people with Alzheimer’s disease than other types of dementia. This tendency may be related to memories and habits from the past, buried deep in long-term memory.
Healthcare workers often see wandering as a problem and disruptive to their care routines. For safety and convenience, they may try to control or prevent the behavior. However, preventing residents from wandering could mean their losing the associated benefits of walking, including improved circulation, decreased pain and stiffness, improved sleep, and decreased risk of pressure sores and contractures (Adekoya and Guse, 2019).
Physical and pharmacological restraints are often used to prevent a person from wandering. Apart from the known harmful effects of restraints, such as pressure sores, anxiety, physical violence, falls, and high morbidity and mortality rates, the intervention is also ineffective. Nonpharmacological interventions are a safer and more effective option and include the use of electronic tagging and tracking devices, behavioral approaches, exercise, music therapy, aromatherapy, camouflaging doorknobs and exits, using strips of tape in front of exit doors, locked units, and environmental modifications (Adekoya and Guse, 2019).
A person’s pre-dementia lifestyle may be a factor in whether a person is likely to wander. People who were physically active, had an interest in music, were extroverted and social, and people who dealt with stress by engaging in motor activities are more likely to wander. Learning about a person’s earlier life allows caregivers to understand individual behaviors and consider effective interventions that address wandering.
For older adults with dementia who spend time in an organized setting such as adult daycare, the management of wandering should, at a minimum include (Silverstein & Flaherty, 2018, 2023):
- Identifying the risk for wandering.
- Providing appropriate staffing and supervision.
- Reducing environmental triggers for wandering.
- Using individualized nursing interventions to address the causes of wandering behavior.
7.2.5 Rummaging and Hoarding
It is unclear to what degree obsessive-compulsive behaviors such as rummaging and hoarding are related to brain deterioration. Memory loss, poor judgment, boredom, and confusion can contribute to the impulse to rummage and hoard. Likewise, feelings of paranoia may create a need to protect possessions and rummaging may create a sense of safety and security.
In people with dementia, hoarding might be due to lack of control, a fear of losing money or possessions, the need to “save for a rainy day,” or simply to have something to do. Hoarding is associated with insecurity and anger and may be an attempt to hold onto possessions and memories from the past. Confusion can lead to rummaging through another person’s belongings, which can be particularly frustrating for neighboring residents.
7.2.6 Sleep Disturbances
Sleep disturbances are common in older adults and are of particular concern in people with dementia. Sleep disturbances probably contribute to the onset and severity of some behavioral problems, particularly anxiety, increased confusion, wandering, and sundowning.*
*Sundowning: an inexact and overused term used to describe increased confusion and restlessness in the late afternoon and early evening, possibly due to damage to the part of the brain that regulates sleep patterns.
A least one-third of people with dementia have difficulty sleeping and more than two-thirds of unpaid caregivers report sleep disturbances themselves. The precipitating factor for institutionalization of those with dementia is often a disturbed sleep–wake (circadian) cycle that leads them to remain awake at night, causing stress and fatigue for their families and caregivers. This behavior continues in nursing home environments, where residents experiencing daytime agitation also tend to sleep poorly at night and nap during the day (Figueiro et al., 2020).
The symptoms of sleep disruption vary according to the type of dementia and can include the following features:
- difficulty getting to sleep, decreased total sleep time, and waking often
- increased early-morning awakenings
- decreased slow-wave and rapid-eye-movement (REM) sleep
- episodes of delirium or disorientation during sleep
- increased daytime napping and daytime sleepiness
- agitation, verbally disruptive behaviors, hallucinations
- nighttime wandering (Burns et al., 2012)
Medications that affect daytime alertness can lead to sleep disturbances. In particular, antidepressants, anti-anxiety medications (such as benzodiazepines), and non-benzodiazepines (hypnotics) can negatively affect sleep patterns. These types of medications are commonly prescribed despite a lack of evidence that they are safe to use in cognitively impaired older adults.
7.3 Inappropriate Behaviors
The ability to control and suppress inappropriate behaviors is an important social skill. The loss of this ability—disinhibition—causes a lack of restraint, disregard for social convention, impulsiveness, poor safety awareness, and an inability to stop strong responses, desires, or emotions.
Inappropriate behaviors are particularly common in a person with frontal-temporal dementia. Disinhibition, impulsivity, and socially inappropriate behaviors are common, together with perseveration*, loss of empathy, apathy, and cognitive inflexibility.
*Perseveration: repetition of a word, phrase, of thought. The inability to shift from one idea to another.
Healthcare providers and caregivers may consider a behavior to be inappropriate when, in fact, the behavior is completely appropriate to the situation. For example, wandering is logical for a person who is bored. Loudly expressing frustration is appropriate when a client is cold or in pain. Whether a behavior is labelled “inappropriate” is often related to the amount of distress the behavior causes caregivers.
7.3.1 Anxiety and COVID-19
Extended lockdowns during the COVID-19 pandemic caused a great deal of stress and anxiety in both patients and caregivers due to isolation, restrictions on movement, loss of social contacts and relationships, and loneliness. Increased anxiety due to fear of contagion and grief or even mourning for the loss of family members or friends undermined mental health (Cagnin et al., 2020).
Early studies have indicated that the COVID-19 pandemic and related restrictions negatively impacted both people with dementia and their caregivers. Since the outbreak of COVID-19, worsening cognitive function, neuropsychiatric symptoms, and functional decline in people with dementia have been reported. In an Italian study, researchers found that more than half of people with dementia experienced worsened neuropsychiatric symptoms. The most commonly observed symptoms were increased agitation, apathy, and depression. Caregivers also reported increased levels of burden, anxiety, depression, and distress during the pandemic (Wei et al., 2022).
7.3.2 Employee Response to Inappropriate Behaviors
Direct care workers, as well as licensed staff, often lack dementia-specific training in how to address inappropriate behaviors in their clients with dementia. The most common behaviors you will encounter are anxiety, aggressive behaviors, and difficulties with communication.
To address these behaviors, begin by acknowledging that each person is worthy of respect—this is the basis for person-centered care. Also remember that there is often a reason for unwanted or inappropriate behavior—even if you don’t understand that reason. Use person-centered care as the basis for your interactions with all clients. This means treating clients and caregivers with dignity and respect.
When discussing difficult or unwanted behaviors with caregivers and fellow workers, ask them to describe what they are seeing instead of using generic terms such as “agitation” or “depression”. Consider the cause, frequency, timing, and trajectory of the disturbances, and any relationship to environmental changes or medication changes. There may be a relationship with changes in a person’s environment, or symptoms might worsen in the evenings, following family visits, or when providing personal care (Cloak and Khalili, 2022).
Callie Disrobes at a Birthday Party
Introduction: Older adults with dementia often exhibit unexpected, challenging behaviors that may be difficult for healthcare workers and family members to understand and manage. These behaviors can be caused by fear, hunger, environmental issues, boredom, side effects of medications, loud noises, lack of exercise, or pain, among other things. In this example, Callie is a 96-year-old woman with moderate to severe dementia who participates in activities at a specialized daycare facility 3 times a week. During a birthday party in the dining room, she suddenly (and quietly) began to remove her clothes.
Client Information: Callie is a client at a specialized daycare facility in south Florida. Although she can walk with assistance, she usually prefers to sit quietly by herself in the living room. She rarely interacts with other clients and prefers simply to watch visitors come and go. Callie often smiles but rarely speaks. However, on occasion she has a negative reaction to large crowds or noisy environments. Staff members understand this and try to remove her from these stressors.
Timeline: On a very warm day in August, a family member has arranged for a birthday party in the living room for her mother. All the residents were invited, including Callie, but the staff forgot to take Callie to a quiet part of the room. With everyone’s attention on the celebration, no one noticed that Callie had begun removing her clothing. A staff member turned just in time to see her take off her slacks and underpants.
Intervention: All staff members had received dementia-specific training and knew that when something unexpected happens, the safety and dignity of the client must come first. Rather than immediately trying to get Callie dressed, which might have caused a negative reaction, the activities director simply asked everyone to leave the room for a few minutes. Jennifer, a nursing assistant, sat next to Callie and quietly asked if she could help Callie get dressed. Callie responded with a definite “no” and pulled off the rest of her clothing.
Another staff member brought a sheet to cover Callie but stood by the door to maintain privacy and see if her help was needed. Jennifer stayed by Callie’s side and after a few minutes asked Callie if she could help. Callie’s response this time was that she was cold. Promising her some birthday cake if she would get dressed, Jennifer was able to help Callie get dressed; after Callie had moved to a quiet area (with a piece of cake), the party goers were brought back into the room.
Discussion: Disinhibition, the loss of awareness of what is appropriate behavior, affects many individuals with dementia. If the staff had gotten upset and embarrassed her, Callie may well have reacted negatively. Temporarily removing the others from the room respected Callie’s dignity and gave her a few moments to experience physical discomfort without her clothes. Once the room quieted down, she accepted assistance and a “reward” for getting dressed again.
Staff members discussed the incident in a meeting the next day and agreed that they had forgotten to keep an eye on Callie as the birthday party got underway. They were reminded that Callie is uncomfortable with noise and lots of activity but that overall, they did a good job diffusing the situation while taking Callie’s dignity and safety into account.
Client Perspective: Callie was unable explain why she took off her clothes, but it was clear that she felt no embarrassment when she did it. In fact, when asked about the incident, she claimed she didn’t remember a birthday party or even being in the dining room that day.
Source: Kisses for Elizabeth: A Common Sense Approach to Alzheimer’s and Dementia (2012), by Stephanie Zeman, RN, MSN.
