Metabolic Changes
Metabolism is all of the chemical reactions that take place in a living organism to keep it alive. It includes anabolism (the building up of things) and catabolism (the breaking down of things). In our bodies the chemical reactions of anabolism build new cells and maintain tissues—and usually need energy. Catabolism uses larger compounds to create smaller ones, releasing energy for physical activity of all kinds. Body weight is catabolism minus anabolism (Nordqvist, 2017; Raman, 2017; Manini, 2010).
The speed of metabolism is affected by four key elements:
- Resting metabolic rate (RMR): calories burned while sleeping/resting
- Thermic effect of food (TEF): calories burned through digesting and absorbing food
- Exercise: calories burned by exercising
- Non-exercise activity thermogenesis (NEAT): calories burned doing such things as standing, wiggling or fidgeting, doing household chores (Nordqvist, 2017; Raman, 2017; Manini, 2010).
Metabolism is also affected by:
- Age
- Height
- Muscle mass
- Hormonal factors
- Gender
As we age, metabolism slows for a variety of reasons including reduced activity, muscle loss, and the aging of the body’s internal parts. Research has shown that while more than one-quarter of Americans age 50 to 65 do not exercise outside of work, that rises to one-third for those over 75 (Raman, 2017; Watson, 2016). Combined with a 29% drop in calories burned through non-exercise activity thermogenesis (NEAT) by older adults. Regular exercise has been shown to mitigate this drop in metabolism (Nordqvist, 2017; Raman, 2017; Manini, 2010).
Musculoskeletal Changes
Sarcopenia and osteoporosis are two of the most common musculoskeletal changes that occur with age. Osteoporosis, which involves a gradual loss of bone density and a thinning of bone tissue, is a silent disease because it progresses without symptoms. Sarcopenia is the age-related loss of muscle mass and strength.
Osteoporosis
Osteoporosis, or porous bone, is a disease characterized by low bone mass and structural deterioration of bone tissue, leading to bone fragility and an increased risk of fractures of the hip, spine, and wrist. Men as well as women are affected by osteoporosis, a disease that can be prevented and treated. In the United States, more than 53 million people either already have osteoporosis or are at high risk due to low bone mass (NIH, 2018).
Bone, made mostly of collagen (a protein) and calcium phosphate (a mineral), is both flexible and strong, which helps it withstand stress. Old bone is removed and new bone added throughout the lifetime. New bone is added faster than old is removed until peak bone mass is reached, usually by the late twenties, and resorption slowly begins to exceed formation (NIH, 2018).
In women, bone loss is fastest in the first few years after menopause and continues into postmenopausal years. Osteoporosis mainly affects women but can also affect men; it develops when bone loss occurs too quickly or bone formation occurs too slowly. There are a number of risk factors for osteoporosis, some of which can be changed and others that cannot (NIH, 2018).
Risk factors that cannot be changed:
- Sex. Chances of developing osteoporosis are greater in women, who have less bone tissue and lose bone faster than men because of the changes that happen with menopause.
- Age. Bones become thinner and weaker with age so the risk of osteoporosis increases.
- Body size. Small, thin-boned women are at greater risk.
- Ethnicity. White and Asian women are at highest risk. African American and Hispanic women have a lower but significant risk.
- Family history. Fracture risk may be due, in part, to heredity.
Risk factors that can be changed:
- Sex hormones. Abnormal absence of menstrual periods (amenorrhea), low estrogen level (menopause), and low testosterone level in men can bring on osteoporosis.
- Anorexia nervosa. This eating disorder increases risk.
- Calcium and vitamin D intake. A lifetime diet low in calcium and vitamin D makes one more prone to bone loss.
- Medication use. Long-term use of certain medications, such as glucocorticoids and some anticonvulsants can lead to loss of bone density and fractures.
- Lifestyle. An inactive lifestyle or extended bed rest tends to weaken bones.
- Cigarette smoking. Smoking is bad for bones as well as the heart and lungs.
- Alcohol intake. Excessive consumption of alcohol increases the risk of bone loss and fractures. (NIH, 2018)
Maintaining adequate intake of calcium and vitamin D (needs change with age), engaging in weight-bearing and resistance exercise, not smoking, moderating alcohol intake, and working with one’s physician regarding medications that contribute to bone loss are all important preventive steps (NIH, 2018).
While white women and those of Asian ancestry have an overall higher risk of osteoporosis than do African American and Hispanic women, the risk is still significant for the latter groups, and some special conditions can be relevant. When compared with white women, Asian American, African American, and Hispanic women have been found to consume too little calcium, perhaps because they are more prone to lactose intolerance. Also, Hispanic women are more likely than white women to develop diabetes, which can increase risk for osteoporosis (NIH, 2015a,b,c).
Symptoms and Diagnosis
Bone loss occurs without symptoms, so a person may not know they have osteoporosis until their bones are so weak that a sudden strain, bump, or fall results in a hip fracture or collapsed vertebra. Collapsed vertebra may present as severe back pain, loss of height, or spinal deformities such as kyphosis (severely stooped posture) (NIH, 2018).
A doctor will do a careful medical history and ask about lifestyle to determine risk factors, including family history of fractures, hormone levels, and use of certain medications. The doctor may also do blood or urine tests and may order a bone mineral density test (NIH, 2015).
A bone mineral density (BMD) test can identify osteoporosis, determine risk for fractures, and measure response to osteoporosis treatment. The most widely recognized BMD test is a central dual-energy x-ray absorptiometry, or central DXA test. The test is painless—like having an x-ray, but with much less exposure to radiation and takes about 15 minutes. It can measure bone density at the hip and spine. BMD tests can:
- Detect low bone density before a fracture occurs.
- Confirm a diagnosis of osteoporosis if a fracture has occurred.
- Predict chances of fracturing in the future.
- Determine rate of bone loss, and monitor the effects of treatment if the test is conducted at intervals of a year or more. (NIH, 2018)
Private insurance will sometimes cover BMD tests ordered by a doctor and Medicare may pay for them under certain circumstances for women and men age 65 and older (NIH, 2015).
Treatment
Treatment of osteoporosis involves a comprehensive program targeting nutrition, exercise, and possibly therapeutic medications. Medications for prevention and/or treatment of osteoporosis include: bisphosphonates; calcitonin; estrogen (hormone therapy); estrogen agonists/antagonists (also called selective estrogen receptor modulators or SERMs); parathyroid hormone (PTH) analog; parathyroid hormone-related protein (PTHrp) analog; RANK ligand (RANKL) inhibitor; and tissue-selective estrogen complex (TSEC).
Fall prevention is another important component in dealing with osteoporosis because falls can increase the likelihood of fracturing a bone of the hip, wrist, spine, or other part of the skeleton. Falls can be caused by environmental factors—indoors and outdoors—and by impaired vision or balance, chronic diseases that affect mental or physical functioning, and certain medications, such as sedatives and antidepressants (NIH, 2018). See the section later in this course on Falls—Risks and Prevention for more discussion and guidelines.
Sarcopenia
Sarcopenia is age-related loss of muscle mass and function. Until about age 30, muscles grow larger and stronger, but during the thirties one starts to lose both muscle mass and function. Inactive people can lose 3% to 5% of their muscle mass every decade after age 30, although those who are active will still experience some loss. Sarcopenia will usually happen faster around age 75 but this speeding up can begin between 65 and 80. There is no test or level of loss that triggers a diagnosis of sarcopenia, because loss reduces strength and mobility and any amount is important. However, in the last 10 years, much has been done to define and aid assessment of sarcopenia (Cruz-Jentoft et al., 2019; Liguori et al., 2018; WebMD, 2018b).
In addition to inactivity, research suggests other factors contribute to the development of sarcopenia, including:
- Reduced number of nerve cells that send signals from brain to muscles
- Lowered concentrations of some hormones (growth hormone, testosterone, insulin-like growth factor)
- Decreased ability to convert protein to energy
- Insufficient daily calories or protein to sustain muscle mass (WebMD, 2018b)
Sarcopenia contributes to frailty and the possibility of falls and fractures. Because weakness and loss of stamina are symptoms that often reduce physical activity, a cycle of reduced activity leads to reduced muscle mass and other symptoms noted earlier. The main treatment for sarcopenia is exercise—resistance training or strength training—that increases muscle strength and endurance and can improve the conversion of protein to energy in older adults (WebMD, 2018b).
There are specific requirements for an exercise program to address sarcopenia and patients need to work with a physical therapist or trainer who has experience dealing with sarcopenia when beginning an exercise plan. Sarcopenia is not usually treated with drugs but there are some currently under investigation for treating it. These include:
- Urocortin II (not yet tested in humans)
- Hormone Replacement Therapy (HRT) (subject to controversy) (WebMD, 2018b)
Other treatments also under investigation include exercise training, nutritional supplementation, hormonal therapies, and some novel strategies. However, only physical exercise has so far demonstrated positive effects on managing and preventing sarcopenia (Liguori et al., 2018).
The condition can have a wide range of negative effects on well-being, including disability, poor quality of life, hospitalization, and death, especially in institutionalized elders, and thus higher medical costs for individuals and society (Liguori et al., 2018). Improved understanding and assessment and treatment tools for healthcare providers are critical.
Sarcopenia has been underrecognized because it has proven difficult to identify, but very recent research (Cruz-Jentoft et al., 2019) details work, especially over the last ten years, to refine and advance a definition for sarcopenia, create tools clinicians can use for assessment, and advance knowledge of the condition and its treatment options.
In 2010 the European Working Group on Sarcopenia in Older People (EWGSOP), established a widely accepted definition in which
[T]he diagnosis of sarcopenia requires the presence of both low muscle mass and low muscle function, which can be defined by low muscle strength or low physical performance (Liguori et al., 2019)
In 2018 the definition was revised to reflect additional scientific and clinical evidence from the last ten years (Cruz-Jentoft et al., 2019).
Integumentary Changes
The integumentary system consists of the skin, hair, and nails; it has a variety of functions. It acts as a waterproof shield and insulates the body against extremes of temperature. It also helps to regulate temperature, cushion and protect the deeper tissues, shield the body from sunlight and harmful chemicals, and excrete wastes. The skin contains sensory receptors to detect pain, sensation, pressure, and temperature and is involved in vitamin D synthesis (MedlinePlus, 2019d, 2018e).
Skin
Skin is the largest organ of the integumentary system (and of the body) and contains three primary layers: (1) the epidermis, (2) dermis, and (3) hypodermis. The outermost layer, the epidermis, is a waterproof barrier and contains no blood vessels. The dermis lies just below the epidermis and contains connective tissue, nerve endings for touch and temperature, and hair follicles, sweat glands, sebaceous glands, and lymphatic and blood vessels. The hypodermis lies below the dermis and connects it to underlying muscle and bone.
Cross Section of Human Skin
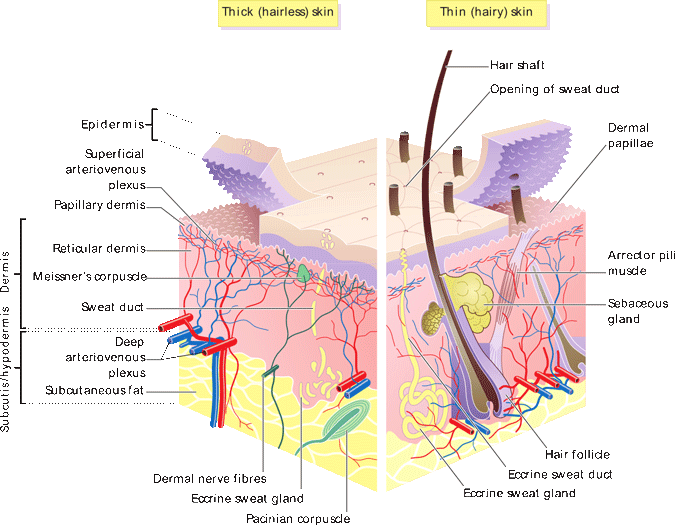
Source: Wikimedia Commons. Author: Madhero88. Original is at https://en.wikipedia.org/wiki/File:Skin_layers.png.
As we age, structures within the skin begin to atrophy and lose elasticity and turgor. A decrease in the number of nerve endings leads to decreased sensation. Melanocytes (pigment-producing cells) decrease, causing gray hair and making the skin more susceptible to sun damage.
As age progresses, the epidermis begins to thin, reducing its protective function and allowing chemicals and pathogens easier access to the body. Adipose tissue also decreases with age, reducing the ability of the skin to cushion the body against trauma and to protect against environmental temperature change. Reduced collagen causes skin to tear more easily.
Older adults who spend most of their time in a bed, chair, or wheelchair can develop pressure sores and related skin damage. The following are important to avoid the problem:
- Change position every one to two hours.
- Keep sheets flat and unwrinkled.
- Help the person practice movement.
- Keep skin clean and dry.
- Massage (not sore areas).
- Use pads or protectors (especially for heels and elbows).
- Observe a good varied diet with enough protein. (HealthinAging.org, 2015).
Hair and Nails
With a decrease in the pigment melanin produced in the hair follicles, hair color fades and turns gray or white. Hair strands become smaller and many hair follicles stop producing hair altogether, causing hair thinning and baldness. Nails grow more slowly and may become dull or yellowed and brittle. Sudden hair loss or the development of nail pits, ridges, lines, changes in shape, or other changes should be checked by a healthcare provider (MedlinePlus, 2019).
Heat Intolerance
Older adults adjust less well to sudden changes in temperature and are more prone to heat stress than younger people. They are more likely than younger people to have a chronic medical condition that changes normal body responses to heat. They are also more likely to be taking prescription medications that inhibit perspiration or impair the body’s ability to regulate temperature (CDC, 2017).
Heat stroke is the most serious heat-related illness in all ages. It occurs when a person is no longer able to control body temperature. This creates a cascade in which body temperature rises rapidly, the body loses its ability to sweat and thus the ability to cool. Body temperatures can rise to 106°F or higher within 10 to 15 minutes. Heat stroke can cause death or permanent disability if emergency treatment is not provided.
Warning signs of heat stroke vary but include the following:
- An extremely high body temperature (above 103°F)
- Hot, red, dry, or damp skin
- Fast, strong pulse
- Headache
- Dizziness
- Nausea
- Confusion
- Losing consciousness
Call 911 right away because this is a medical emergency. In the meantime, move the person to a cooler place and help lower their temperature with cool cloths, spritzing with water, a cool bath, or whatever is at hand. Do not give the person anything to drink(CDC, 2017a).
Heat exhaustion is a milder form of heat-related illness that can develop after several days of exposure to high temperatures and inadequate or unbalanced replacement of fluids.
Warning signs of heat exhaustion vary but may include the following:
- Heavy sweating
- Cold, pale, and clammy skin
- Fast, weak pulse
- Nausea or vomiting
- Muscle cramps
- Tiredness or weakness
- Dizziness
- Headache
- Fainting
Move the person to a cool place, loosen clothing, put cool wet cloths on the body or place in a cool bath. Get immediate medical help if the person is throwing up or if symptoms worsen or last longer than 1 hour (CDC, 2017a).
To protect elders from heat stress, encourage them to drink cool, nonalcoholic beverages and to drink more fluids than normal—not wait until thirsty to drink. However, if the person is on a limited fluid intake or water pills, consult their health professional about safe fluid intake. Avoid very sugary or alcoholic drinks as they cause more loss of body fluid, and avoid extremely cold liquids because they can cause cramps.
Cool showers or baths can be helpful. Do not rely on fans in extreme heat. If the home is not air-conditioned, suggest visiting an air-conditioned public space such as a shopping mall or public library. Contact the local health department for locations of air-conditioned shelters or other suggestions.
Loose, lightweight, light-colored clothing is recommended and, if possible, the older person should remain indoors during the heat of the day. Strenuous activity is to be avoided and plenty of rest is important (CDC, 2017a,b).
Hypothermia
Hypothermia (abnormally low body temperature) and frostbite are both dangerous conditions that can happen when a person is exposed to extremely cold temperatures (CDC, 2019). Hypothermia is caused by prolonged exposure to very cold temperatures resulting in the body losing heat faster than it is produced. If the exposure is long enough, all the body’s stored energy can be used up, leading to a lower body temperature (CDC, 2019). Hypothermia occurs as body temperature falls below 96 or 95 degrees F (CDC, 2019; Mayo Clinic, n.d.).
Bodies lose heat (1) when it is radiated from unprotected body surfaces, (2) due to direct contact with something very cold, or (3) due to wind. Situations can include:
- Wearing clothes that aren’t warm enough for weather conditions
- Staying out in the cold too long
- Being unable to get out of wet clothes or move to a warm, dry location
- Falling into the water, as in a boating accident
- Living in a house that’s too cold, either from poor heating or too much air conditioning (Mayo Clinic, n.d.)
Low body temperature affects brain function, preventing the victim from thinking clearly or moving well. Thus, the person may not even realize what is happening or be able to act to get to safety. Even though hypothermia is most likely to occur at very cold temperatures, it can occur at cool temperatures (above 40 degrees F) if the person becomes chilled (CDC, 2019).
Symptoms of hypothermia usually manifest first as shivering but include the following:
- Shivering
- Slurred speech or mumbling
- Slow, shallow breathing
- Weak pulse
- Clumsiness or lack of coordination
- Drowsiness or very low energy
- Confusion or memory loss
- Loss of consciousness
These may begin gradually, which along with the confused thinking, may prevent the person from realizing what is happening or may lead to risky behaviors (Mayo Clinic, n.d.).
Hypothermia can be a particular problem for older adults because of the body’s decreased ability to regulate and sense temperature. Medical conditions such as Parkinson’s, hypothyroidism, stroke, severe arthritis, diabetes, poor nutrition, trauma, spinal cord injuries, may affect the body’s temperature regulation abilities, as can certain medications including antidepressants, antipsychotics, narcotic pain medications, and sedatives.
Conditions that decrease sensation and movement, interfere with circulation, or cause the body to lose more heat than normal can all contribute to hypothermia (Mayo Clinic, n.d.). In addition, older adults may not be able to communicate that they are cold or move themselves to a warmer location.
In mild cases in older people a diagnosis may not be readily apparent, as for example when an older person who is not outside exhibits confusion, lack of coordination, and speech problems (Mayo Clinic, n.d.)—an important reminder that some symptoms can be shared across many conditions and keeping an open mind and inquiring as to details can be critically important when working with elders.
Treatment
Hypothermia requires immediate medical attention but while waiting for help to arrive the following are recommended:
- Use gentle, limited movements and only when necessary. No massage or rubbing. Excessive, vigorous or jarring movements may trigger cardiac arrest.
- Move out of the cold. Move to a warm, dry location if possible. Otherwise shield from cold and wind and keep in a horizontal position if possible.
- Remove wet clothing, cutting away if necessary.
- Cover with blankets, using layers of dry blankets or coats; cover the head, leaving only the face exposed.
- Insulate the person’s body from the cold ground by placing the person on the back on a blanket or other warm surface.
- Monitor breathing. A person with severe hypothermia may appear unconscious, with no apparent signs of a pulse or breathing. If the person’s breathing has stopped or appears dangerously low or shallow, begin CPR immediately (if trained).
- Provide warm beverages if the affected person is alert and able to swallow. Provide a warm, sweet, nonalcoholic, noncaffeinated beverage to help warm the body.
- Use warm, dry compresses. Use a first-aid warm compress (a plastic fluid-filled bag that warms up when squeezed) or a makeshift compress of warm water in a plastic bottle or a dryer-warmed towel. Apply a compress only to the neck, chest wall, or groin.
- Do not apply a warm compress to the arms or legs as heat applied to the arms and legs forces cold blood back toward the heart, lungs and brain, causing the core body temperature to drop, which can be fatal.
- Do not apply direct heat such as hot water, a heating pad, or a heating lamp. The extreme heat can damage the skin or, even worse, cause irregular heartbeats so severe that they can cause the heart to stop. (Mayo Clinic, n.d.)
Once at a medical facility, treatment may include:
- Passive rewarming
- Blood rewarming
- Warm intravenous fluids
- Airway rewarming
- Irrigation (Mayo Clinic, n.d.)
Cardiovascular Changes
[This section is taken largely from NIA, 2018 & CDC, 2015.]
The heart is a strong muscle responsible for pumping blood to the rest of the body, and when healthy a normal adult heart is about the size of a clenched fist. The right side of the heart pumps blood to the lungs to obtain oxygen and the left side receives this oxygen-rich blood and pumps it via the arteries throughout the body. Each side has two chambers—atrium at the top and ventricle at the bottom—all controlled by an electrical system that controls the heart rate and coordinates contraction of the chambers.
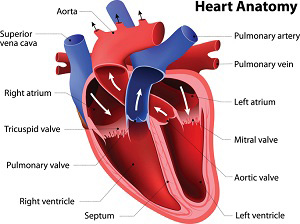
Source: NIH, 2018.
Adults age 65 and older are much more likely than younger people to experience a heart attack or a stroke or to develop coronary heart disease (heart disease) or heart failure. Changes to the heart and blood vessels can be caused by age and, while one’s heart rate at rest does not change significantly with normal aging, older hearts cannot beat as fast during stressful times or during physical activity.
Over many years, fatty deposits can build up on artery walls and cause heart disease but a number of actions can be taken to mitigate this. The most common aging change is arteriosclerosis—hardening of the arteries—which can cause hypertension (high blood pressure), and is more common with aging.
Hypertension joins other risk factors, including increased age, to increase the possibility of developing atherosclerosis—buildup of fatty deposits, or plaques, in the walls of the arteries over many years. A number of these risk factors are modifiable so atherosclerosis is not necessarily a normal part of aging.
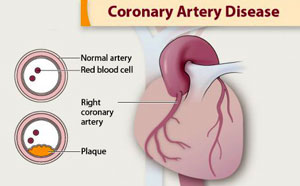
Source: CDC.
Coronary artery disease is caused by plaque buildup in the wall of the arteries that supply blood to the heart (called coronary arteries). Plaque is made up of cholesterol deposits. Plaque buildup causes the inside of the arteries to narrow over time. This process is called atherosclerosis.
The buildup of fatty deposits over time hardens and narrows the arteries, limiting oxygen-rich blood flow to the organs and other parts of the body. When the plaque buildup takes place in the coronary arteries and reduces blood flow to the heart muscle, heart disease develops. This can weaken and/or damage the heart and lead to heart failure. Heart damage can come from heart attacks, long-standing hypertension, and chronic heavy alcohol use. There are other age-related changes to the heart, including:
- Changes in the electrical system that lead to arrhythmias—rapid, slowed, or irregular heartbeat—and/or the need for a pacemaker. The valves that control blood flow between the chambers can become thicker and stiffer, which can constrict the flow of blood from the heart or become leaky.
- Chambers of the heart may increase in size. The heart wall thickens so the amount of blood a chamber can hold may decrease despite the increased overall heart size. The heart may fill more slowly. The main cause of thickening of the heart wall is long-standing hypertension and it can increase the risk of atrial fibrillation, a common heart rhythm problem in older people.
- With increasing age, people experience increased sensitivity to salt, which can cause increased blood pressure and/or edema (swelling) of the ankles or feet.
Other factors that can weaken the heart muscle include thyroid disease or chemotherapy, and there are heart disease risks one cannot control such as family history. However, heart-healthy lifestyle choices can help avoid or delay serious illness.
Ischemic Heart Disease
[This section is taken largely from NHLBI, n.d.]
Heart disease is a catch-all phrase for a variety of conditions that affect the heart’s structure and function. Ischemic heart disease occurs when the arteries of the heart cannot deliver enough oxygen-rich blood to the heart. It is the leading cause of death in the United States, with most deaths occurring from coronary heart disease (CHD), also known as coronary artery disease (CAD)—the most common type of ischemic heart disease.
Coronary heart disease is caused by the buildup of plaque inside the coronary arteries. This buildup can partly or totally block blood flow in the large arteries of the heart. Some types of this condition may be caused by disease or injury affecting how the arteries work in the heart. Coronary microvascular disease (CMD) is another type of ischemic heart disease. It occurs when the heart’s tiny arteries do not function normally.
Symptoms of ischemic heart disease may differ from person to person even if they have the same type of ischemic heart disease. However, because many people have no symptoms, they do not know they have heat disease until they experience complications such as a heart attack or sudden cardiac arrest.
There are three main types of ischemic heart disease:
- Obstructive coronary artery disease
- Nonobstructive coronary artery disease
- Coronary microvascular disease
Coronary artery disease affects the large arteries on the surface of the heart and many people have both obstructive and nonobstructive forms of this disease. Coronary microvascular disease affects the tiny arteries in the heart muscle. It may occur with or without coronary artery disease.
There are many risk factors for ischemic heart disease. The risk increases with the type and number of risk factors and how serious they are. Some risk factors—such as high blood pressure and high blood cholesterol—can be changed through heart-healthy lifestyle changes. Other risk factors, such as sex, older age, family history and genetics, and race and ethnicity, cannot be changed.
Genetic or lifestyle factors cause plaque to build up in the arteries as a person ages. In men, the risk for ischemic heart disease starts to increase around age 45. Before menopause, women have a lower risk for ischemic heart disease than men. After around age 55, however, the risk increases at the same rate in both women and men. This is likely because the protective effects of the female hormone estrogen diminish after menopause. Also, changes in the small blood vessels of the heart with age increase the risk for coronary microvascular disease.
It is important to know the symptoms of heart attack (myocardial infarction, or MI). Call 911 at the first sign of heart attack symptoms—these individuals should not drive themselves to the hospital. Treatment works best when it’s given right after symptoms occur, so acting fast can save lives and limit damage to the heart.
Heart attack symptoms vary from person to person and are often different for women than men, but they can include:
- Chest pain or discomfort. This involves uncomfortable pressure, squeezing, fullness, or pain in the center or left side of the chest that can be mild or strong. This discomfort or pain often lasts more than a few minutes or goes away and then comes back.
- Upper body discomfort in one or both arms, the back, neck, jaw, or upper part of the stomach.
- Shortness of breath, which may occur with or before chest discomfort.
- Nausea, vomiting, light-headedness or sudden dizziness, or breaking out in a cold sweat.
- Sleep problems, fatigue (tiredness), and lack of energy.
Stroke
[This section taken is taken largely from NINDS, 2018 and NHLBI, n.d.-a.]
A stroke, sometimes called a “brain attack,” occurs when the blood supply to part of the brain is suddenly interrupted or when a blood vessel in the brain bursts, spilling blood into the spaces surrounding brain cells.
An ischemic stroke occurs when an artery supplying the brain with blood becomes blocked, suddenly decreasing or stopping blood flow and ultimately causing a brain infarction. This type of stroke accounts for approximately 80% of all strokes. Blood clots are the most common cause of artery blockage and brain infarction.
The Brain During an Embolic Stroke
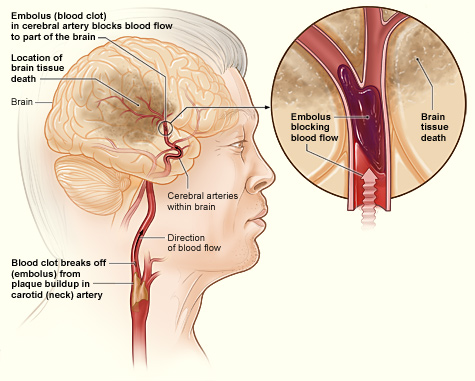
Source: NHLBI, n.d.-a
When an artery in the brain bursts, blood spews out into the surrounding tissue and upsets not only the blood supply but also the delicate chemical balance neurons require to function. This is called a hemorrhagic stroke. Such strokes account for approximately 20% of all strokes.
Ruptured Aneurysm with Associated Bleeding in the Brain
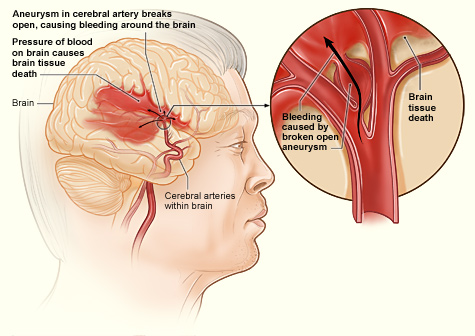
Source: NHLBI, n.d.-a
Stroke strikes all age groups, from fetuses still in the womb to centenarians. However, older people have a higher risk for stroke than the general population and the risk for stroke increases with age. For every decade after the age of 55, the risk of stroke doubles, and two-thirds of all strokes occur in people over age 65. People over 65 also have a seven-fold greater risk of dying from stroke than the general population. The incidence of stroke is increasing proportionately with the increase in the elder population, and when the baby boomers move into the over-65 age group, stroke and other diseases will take on even greater significance in the healthcare field.
Gender plays a role in risk for stroke. Men have a higher risk for stroke, but more women die from stroke. The stroke risk for men is 1.25 times that for women. But men do not live as long as women, so men are usually younger when they have strokes and therefore have a higher rate of survival than women. In other words, even though women have fewer strokes than men, women are generally older when they have their strokes and are more likely to die from them.
Race and ethnicity also play a role in stroke incidence and risk. Stroke incidence among African Americans is almost double that of whites, and twice as many African Americans die from them. Although African Americans between the ages of 45 and 55 have 4 to 5 times the stroke death rate of whites, after age 55 the stroke mortality rate for whites increases and is equal to that of African Americans. African Americans also have a higher incidence of stroke risk factors than do whites. Hispanics, Native Americans, and Asian Americans all have incidence and mortality rates similar to those of whites.
Symptoms of a stroke are easy to spot. They include sudden numbness or weakness, especially on one side of the body; sudden confusion or trouble speaking or understanding speech; sudden trouble seeing in one or both eyes; sudden trouble walking, dizziness, or loss of balance or coordination; or sudden severe headache with no known cause. All of the symptoms of stroke appear suddenly, and often there is more than one symptom at the same time. Thus, stroke can usually be distinguished from other causes of dizziness or headache, symptoms which are common to other problems as well.

Source: National Institutes of Health.
Risk factors for stroke include:
- Hypertension
- Heart disease
- Diabetes
- Cigarette smoking
- Heavy alcohol consumption
- High blood cholesterol levels
- Illicit drug use
- Genetic or congenital conditions (particularly vascular abnormalities)
People with more than one risk factor have what is called “amplification of risk,” which means that multiple risk factors compound destructive effects, and cause overall risk to be greater than simply adding up the individual risk factors.
Many older adults already have increased problems with hypertension, heart disease, diabetes, and maintaining healthy cholesterol levels. Forty to seventy percent of adults over age 65 have high blood pressure—the most powerful risk factor for stroke—making their risk for stroke 4 to 6 times higher than for those without hypertension.
Managing risk factors and observing a healthy lifestyle is just as critical for older adults as for younger people. Working with healthcare providers to manage high blood pressure, heart disease, cholesterol levels, and diabetes in conjunction with quitting smoking and illicit drug use, and decreasing excess consumption of alcohol, are all important. In addition, keeping physically active, maintaining a healthy weight, managing stress, and making heart-healthy eating choices all help to reduce risk—for cardiovascular events of all kinds.
Urinary Changes
The kidneys along with the ureters, bladder, and urethra make up the urinary system. The kidneys filter the blood, help remove wastes and extra fluid from the body, and help control the body’s chemical balance. With age, the kidneys and bladder change, which can affect their function.
The number of nephrons (the filtering units of the kidneys) decreases with age and the kidneys are less able to filter waste from the blood. Blood vessels that supply the kidneys become stiffer, causing the kidneys to filter blood more slowly. The overall amount of kidney tissue also decreases and there is a reduced capacity for renal regeneration in the face of acute renal insults (MedlinePlus, 2019).
Changes to the bladder affect both the bladder wall and muscles. With a toughening of the bladder wall tissue it becomes less stretchy and the bladder cannot hold as much urine as it could previously. Bladder muscles also weaken. Blockage of the urethra can happen in both men and women. If the bladder or vagina has prolapsed (fallen out of position) it can block a woman’s urethra, while in men blockage can be caused by an enlarged prostate gland (MedlinePlus, 2019).
Healthy aging can still involve effects on kidney function from illness, medicines, or other conditions. Common problems for older adults include:
- Bladder control issues—leakage or incontinence (not being able to hold it) and retention (not being able to completely empty the bladder)
- Bladder or other urinary tract infections (UTIs)
- Chronic kidney disease (MedlinePlus, 2018)
Urinary Tract Infections
Urinary tract infections (UTIs) occur when bacteria enter and infect the urinary tract. UTIs can affect several parts of the urinary tract, but the most common type of UTI is a bladder infection (also known as cystitis). Most are not serious and can be treated with antibiotics or antifungals (depending on infection source) and the body can sometimes fight the bacteria without any problems; however, the infection can cause discomfort and may sometimes spread to the kidneys. Kidney infections (also known as pyelonephritis) are less common but more serious (CDC, 2015).
Symptoms of UTI vary by age, gender, and whether a catheter is present. Among young women, UTI symptoms typically include a frequent and intense urge to urinate and a painful, burning feeling in the bladder or urethra during urination. The amount of urine per void may be very small (NIDDK, 2017). Other symptoms include:
- Cloudy, dark, bloody, or foul-smelling urine
- Low grade fever in some people
- Pressure or cramping in lower abdomen or back
If the infection has spread to the kidneys:
- Chills and shaking or night sweats
- Fatigue and a general ill feeling
- Fever above 101°F (38.3°C)
- Pain in the side, back, or groin
- Flushed, warm, or reddened skin
- Mental changes or confusion
- Nausea and vomiting
- Very bad abdominal pain (sometimes) (MedlinePlus, 2018a)
Women are more likely than men to get UTIs and older adults are more likely than younger ones. Other conditions that may affect older adults and also increase risk for UTIs including: increased susceptibility to infections, reduced mobility, urinary incontinence or retention, urinary catheter placement, prostate enlargement, and dementia, or other conditions interfering with personal hygiene (CDC, 2015; MedlinePlus, 2018, 2018a,b).
It is important to note that for older adults mental changes or confusion often are the only signs of a UTI; however, it is also important to note that this is a common indication of the onset of other acute illnesses in older adults and signals the need for attention to all relevant details for diagnosis (MedlinePlus, 2018a; Flaherty, 2011).
Urinary Incontinence
Incontinence is often seen as part of aging, and while it is more common in older people (especially women), it can occur for many other reasons, and it can contribute to skin breakdown and infection and also to (UTIs). UTIs, vaginal infection or irritation, constipation, and some medications can cause bladder control problems that last a short time. When incontinence lasts longer, it may be due to (NIA, 2017d):
- Weak bladder muscles
- Overactive bladder muscles
- Weak pelvic floor muscles
- Damage to nerves that control the bladder from diseases such as multiple sclerosis, diabetes, or Parkinson’s disease
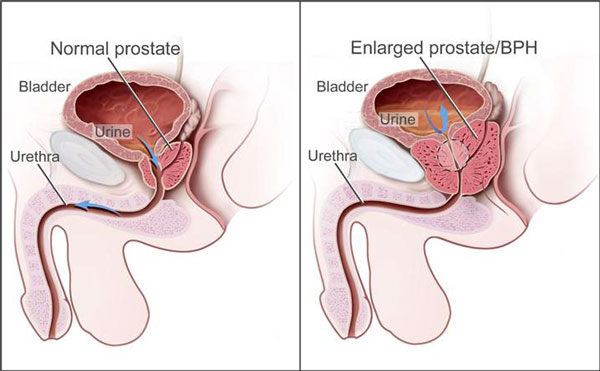
- Blockage from an enlarged prostate in men
- Diseases such as arthritis that may make it difficult to get to the bathroom in time
- Pelvic organ prolapse, which is when pelvic organs shift out of their normal place into the vagina
In men, most incontinence is related to the prostate gland and may be caused by:
- Prostatitis—a painful inflammation of the prostate gland
- Injury or damage to nerves or muscles from surgery
- An enlarged prostate gland, which can lead to BPH (NIA, 2017d)
During urination, muscles in the bladder tighten to move urine into the urethra. At the same time, the muscles around the urethra relax and let the urine pass out of the body. When the muscles in and around the bladder don’t work the way they should, urine can leak. Incontinence typically occurs if the muscles relax without warning (NIA, 2017d).
A healthcare provider should be consulted to determine the cause of urinary incontinence, and urine and blood tests should be done to rule out infection. Tests may also be done to determine how well the bladder is emptying. The patient may be asked to keep a daily diary to track times of urination or leakage (NIA, 2017d).
There are different types of urinary incontinence and the healthcare provider can tailor treatment based on which type or types the patient is experiencing (NIA, 2017d):
- Stress incontinence happens when urine leaks as pressure is put on the bladder, for example, during exercise, coughing, sneezing, laughing, or lifting heavy objects. It is the most common type of bladder control problem in younger and middle-aged women. It may also begin around the time of menopause.
- Urge incontinence happens when people have a sudden need to urinate and are not able to hold their urine long enough to get to the toilet in time. It is often, but not only, a problem for people who have diabetes, Alzheimer’s disease, Parkinson’s disease, multiple sclerosis, or stroke.
- Overflow incontinence happens when small amounts of urine leak from a bladder that is always full. A man can have trouble emptying his bladder if an enlarged prostate is blocking the urethra. Diabetes and spinal cord injury can also cause this type of incontinence.
- Functional incontinence happens in many older people who have normal bladder control. They just have a problem getting to the toilet because of arthritis or other disorders that make it hard to move quickly. (NIA, 2017d)
Treatment options include medicines, estrogen creams, injecting a substance to help close the bladder opening, medical devices, nerve stimulation, and surgery. In addition, there are several ways a person can improve bladder control, including pelvic muscle exercises (Kegel exercises), biofeedback, timed voiding, and certain lifestyle changes (NIA, 2017d).
There are four categories of medications that can cause or worsen urinary incontinence; however, their effects vary from person to person and are not necessarily the same in men and women. These include medications for hypertension and depression, along with diuretics and sleeping pills. Healthcare providers need to be aware of all medications, including OTC and supplements, that a patient is taking when evaluating for treatment (WebMD, 2018).
Prostate Changes and Prostate Cancer
The prostate is a small gland that is part of the male reproductive system and is located just below the bladder and in front of the rectum. It surrounds the urethra and is about the size of a walnut in a man in his twenties. As a man ages, the prostate tends to increase in size and may be the size of a lemon by age 60. This can squeeze the urethra and decrease urine flow. This is called benign prostatic hyperplasia (BPH), and it is not the same as prostate cancer (CDC, 2018a; NCI, n.d.)
Prostate cancer is the second most common cancer among men in the United States (after skin cancer) but most who have it are older than 65 and do not die from it. Prostate cancer tends to grow slowly compared with most other cancers, and cell changes can begin 10 to 30 years before a tumor is large enough to cause symptoms. More than half of all American men have some cancer in their prostate glands by the age of 80. Most of them never pose a problem and may never cause symptoms or become a serious health threat (NCI, n.d.).
Risk factors include age, race, family history, and diet. Men over age 50 have a higher risk, and African American men have the highest risk. It tends to start younger and grow faster in African American men than in men of other races. Asian American men have the lowest rates of prostate cancer. Men with a father or brother who had prostate cancer have a risk 2 to 3 times that of men with no family history of the disease. Finally, the risk may be higher for men who consume high-fat diets.
Symptoms of prostate cancer can include:
- Trouble passing urine
- Frequent urge to pass urine, especially at night
- Weak or interrupted urine stream
- Pain or burning when passing urine
- Blood in the urine or semen
- Painful ejaculation
- Nagging pain in the back, hips, or pelvis
Some of the symptoms of BPH are similar to those for prostate cancer, so they should be reported to a man’s healthcare provider for evaluation and treatment. For most men, screening for prostate cancer may not be necessary, but if a man has risk factors then a doctor can help make that decision (CDC, 2018a; NCI, n.d.).
Respiratory Changes
The lungs bring oxygen from the air into the body and remove carbon dioxide from the body, sending it back into the air. During breathing, inhaled air travels through the airways to the lungs. Airways are composed of stretchy tissue supported by bands of muscle and other tissue that wrap around them to keep them open. The respiratory tract also warms and moistens the incoming air, regulates air flow, removes airborne particles, and cools the entire organism.
A number of age-related changes affect the respiratory system, including changes to:
- Bones and muscles of the spine
- Lung tissue
- Nervous system
- Immune system
The bones and muscles of the chest and spine become thinner and change shape, which can change the ribcage’s shape and impact its ability to expand and contract when breathing. The diaphragm (the muscle that supports breathing) becomes weaker and may prevent a person from breathing enough air in or out. These changes can cause a reduction in oxygen level or a failure to remove enough carbon dioxide and can cause shortness of breath and tiredness (MedlinePlus, 2018c).
Muscles and other tissues around airways are designed to keep airways open but with age they can lose that ability and allow airways to close easily. Air sacs can also lose their shape and become baggy as a person ages. Both of these changes can allow air to be trapped in the lungs so that too little oxygen gets into the blood and not enough carbon dioxide gets out, making it hard to breathe (MedlinePlus, 2018c).
With age, the part of the brain that controls breathing may lose some function, which can also mean that not enough oxygen gets in or carbon dioxide out and breathing is difficult. Nerves in the airways that trigger coughing can also become less sensitive, making it hard to cough up particles or germs that then collect in the lungs (MedlinePlus, 2018c).
Finally, the immune system can get weaker with age and may not be able to fight off lung infections or other diseases, and the lungs may be less able to recover from exposure to smoke or other harmful particles (MedlinePlus, 2018c).
All of these changes increase the risks faced by older people for:
- Lung infections (ie, pneumonia and bronchitis)
- Shortness of breath
- Low oxygen level
- Abnormal breathing patterns, which can cause other conditions such as sleep apnea (MedlinePlus, 2018c)
Endocrine Changes
The endocrine system is made up of glands that secrete hormones that regulate the body’s growth and development, metabolism (digestion, elimination, breathing, blood circulation, maintenance of body temperature), sexual function, reproduction, and mood. With age, some hormones increase or decrease, some target organs become less receptive, and hormones may be broken down more slowly (MedlinePlus, 2018d, 2019).
Despite age-related changes that affect nearly every gland, the endocrine system functions well in most older people. However, some changes do occur because of damage to cells during the aging process, accumulated effects of medical issues, or genetically programmed cellular changes. These changes may alter:
- Hormone production and secretion
- Hormone metabolism (how quickly excess hormones are broken down and leave the body)
- Hormone levels circulating in blood
- Target cell or target tissue response to hormones
- Rhythms in the body, such as the menstrual cycle (Endocrine Society, 2018)
Increasing age is thought to be related to the development of type II diabetes, which is the most common endocrine disease in the United States (MedlinePlus, 2019). Diabetes is a disorder that causes repeated episodes of inappropriately high concentrations of glucose in the bloodstream. This chronic hyperglycemia gradually produces tissue damage, notably to eyes, kidneys, nerves, heart, and blood vessels. With aging, the target cell response time becomes slower, especially in people who might be at risk for this disorder.
With population aging, the number of adults over 65 is increasing, and it is estimated that 33% of adults 65 and older have diabetes. This elder population is also more likely than younger people to develop complications related to diabetes, such as hypoglycemia, kidney failure, and heart disease (Endocrine Society, 2019).
The American Diabetes Association estimates that, in 2015, 30.3 million Americans (9.4% of the population) had diabetes and 7.2 million of them do not know they have it. Of Americans age 65 and older, 25.2% (12 million) have diabetes (diagnosed and undiagnosed). Another 84.1 million people over age 18 have prediabetes, a condition with increased blood sugar levels that are not yet elevated enough to be called diabetes. The rate of diagnosed diabetes in adults is lowest among non-Hispanic whites at 7.4% and highest among American Indians/Alaskan Natives at 15.1% (ADA, 2018).
The aging population presents challenges for treating endocrine disorders for several reasons. Disorder manifestation in older patients is often atypical, presents as nonspecific geriatric symptoms, or is believed to be a function of “old age” by patients. The symptoms of an endocrine illness may be mistaken for a medication problem or the worsening of a comorbid illness. Older patients may have no particular symptoms and only biochemical evidence of a condition. Treatment of older patients must take all of these things into account and be cognizant of issues of polypharmacy. It has been suggested that endocrine disorders in seniors may be best treated using an interdisciplinary care model (Matsumoto & Robertson, 2016).
Gastrointestinal Changes
The digestive system is made up of the gastrointestinal tract—also called the GI tract or digestive tract— and the liver, pancreas, and gallbladder. The GI tract is a series of hollow organs joined in a long, twisting tube from the mouth to the anus. Digestion is the process by which food and drink are broken down into their smallest parts so the body can use them for energy, growth, and cell repair (NIDDK, 2017a).
The digestive system is less affected by aging than other organ systems, nevertheless aging is a factor and older adults are more likely to develop diverticulosis and digestive tract disorders like constipation as a medication side effect (Ruiz, 2017).
Gastroesophageal reflux disease (GERD) occurs when the lower esophageal sphincter does not close properly and stomach contents leak back (reflux) into the esophagus. Heartburn that occurs more than twice a week may be considered GERD, and it can eventually lead to more serious health problems (MedlinePlus, 2019a).
Food intake may decrease in the older adult for several reasons. An older person’s ill-fitting dentures or tooth decay can make chewing difficult. Decreased saliva production causes dry mouth, which may increase tooth decay and even make swallowing more difficult. Taste becomes less acute, making food less appetizing.
Decreased intestinal motility and slower stomach emptying can lead to altered absorption of nutrients and medications. Decreased physical activity, decreased intestinal motility, and a lessened urge to defecate can lead to constipation.
Constipation
Nearly everyone becomes constipated at one time or another, but older people are more likely than younger people to become constipated. Constipation is estimated to affect 2% to 27% of the general population in the United States—but 20% to 74% of older patients—and is highest among institutionalized individuals (Chokhavatia et al., 2016).
Constipation is a symptom, not a disease. An individual may be constipated if there are fewer bowel movements than usual, it takes a long time to pass stools, and the stools are hard. There is no correct number of daily or weekly bowel movements. Being regular is different for each person. For some, it can mean bowel movements twice a day and for others having movements three times a week is normal.
The cause of constipation is not always known. It may be poor diet, not getting enough exercise, or using laxatives too often. Reasons for constipation include:
- Diet low in fiber, vegetables, fruits, and whole grains
- Loss of interest in cooking and eating
- Dental problems
- Lack of water and other fluids
- Overuse of laxatives and enemas
- Lack of exercise
- Holding back or ignoring the urge to have a bowel movement
In addition, constipation can result from medical conditions such as stroke, diabetes, a blockage in the intestines, or Irritable bowel syndrome (IBS), and from medications used to treat depression, antacids containing aluminum or calcium, iron supplements, some antihistamines, certain painkillers, some hypertension drugs (including diuretics), and some drugs used to treat Parkinson’s disease (NIDDK, 2018; NIA, 2013, MedlinePlus, 2019b).
When serious causes of constipation have been ruled out, dietary and lifestyle changes can be tried for problems with constipation. Fiber should be added to the diet by eating more fresh fruits and vegetables, either cooked or raw, and more whole-grain cereals and breads.
If the diet does not include natural fiber, a small amount of bran may be added to baked goods, cereal, and fruit. This may cause some bloating and gas in the beginning, so diet changes should be made slowly to allow the system to adapt. Fiber products such as psyllium seed may be used and are found in the grocery store.
Drinking more water and juice—at least three 12-oz glasses of water each day unless medically contraindicated—and staying active helps prevent constipation and is also important for overall health.
If these changes don’t work, laxatives may be considered. If constipation continues to be a problem, it is important to seek medical advice. A change in bowel habits, blood in the stool, abdominal pain, or recent unexplained weight loss may be signs of a more serious problem (NIA, 2013).
Older adults regularly taking narcotic pain medications frequently experience constipation that is often underrecognized and undertreated. Opioid pain medications slow movement of stool through the intestinal tract and the stool becomes hard and more difficult to expel. The usual treatments of fiber, fluids, and exercise are not sufficient and traditional laxatives are no always effective or appropriate. Some prescription drugs have become available but the complexity of the situation in older patients calls for careful attention from healthcare professionals to resolve individual cases (Chokhavatia et al., 2016).
Other Gastrointestinal Problems
- Gallstones—formed from hardened digestive fluid in the gallbladder—are very common, affecting 10% to 15% of the U.S. population, and being over age 40 increases the risk of developing them. They can cause abdominal pain, especially in the right upper abdomen and right upper back (NIDDK, 2017c).
- Loss of muscle strength with aging can lead to diverticular disease. Diverticulosis is very common and occurs in 10% of people over age 40 and in 50% of people over age 60. Although most people have few or no symptoms, the diverticula may become infected (diverticulitis) or cause bleeding (WebMD, 2018a).
- The risk for colorectal cancer increases dramatically after age 50 and about 90% of all colorectal cancers are diagnosed in adults over age 55 (NCI, 2019). Symptoms can include rectal bleeding, constipation or loose stools, weight loss, abdominal pain, and fatigue. It is generally recommended that all individuals have a colonoscopy every 10 years beginning at age 50, and younger or more often depending on family and personal history. Alternative tests may be appropriate for certain patients (NIDDK, 2017b).
Sensory Changes
As the senses become less acute with age, less information can be gathered and processed about the world around us. The prevalence of sensory impairments is increasing as life expectancy increases. In order to maintain independent living, health, and quality of life for older adults it is important to minimize the impact of sensory impairments.
Data shows the critical interplay of sensory deficits in older adults with other deficiencies and overall quality of life. Vision impairment, which correlates with depression, poor quality of life, cognitive decline, and mortality, occurs in 18% of adults age 70 and older. Hearing impairment, associated with slower gait speed, poor cognition, and mortality, is found in 33% of the same age group.
Loss of smell and taste, both of which have been associated with compromised nutrition and in-patient mortality, affect many adults 70 and older. In addition, multisensory impairment is not uncommon; 67% of older adult Americans have two or more sensory deficits, while only 6% have none (Correia et al., 2016).
Hearing
Hearing loss is one of the most common conditions affecting older adults. Approximately 1 in 3 people between 65 and 74 and nearly half of those older than 75 have hearing loss, making it hard to understand and follow a doctor’s advice, respond to warnings, and hear doorbells and alarms. Hearing loss can also make it difficult to enjoy talking with friends and family.
Many people lose their hearing slowly as they age, a condition known as presbycusis. Presbycusis most commonly arises from gradual changes in the inner ear as a person ages, but may also result from changes in the middle ear or from complex changes along the nerve pathways leading to the brain.
Age-related hearing loss most often occurs in both ears and affects them equally. Because the loss of hearing is gradual, people may not realize that their hearing is diminishing. Doctors do not know why this condition affects people differently but it seems to run in families.
Years of exposure to noise that is either too loud or lasts too long can result in noise-induced hearing loss. This kind of noise exposure can damage the ears’ sensory hair cells, which do not grow back, so hearing is diminished. Most older people with hearing loss have a combination of age-related and noise-induced hearing loss.
Conditions more common in older people, such as high blood pressure or diabetes, can contribute to hearing loss. But it can also be caused by viral or bacterial infections, heart conditions or stroke, head injuries, tumors, and certain medicines toxic to sensory cells in the ear (eg, some used in chemotherapy) (NIDCD, 2018, 2018a).
Vision
Ninety percent of blindness caused by diabetes is preventable.
CDC, 2017g
As people age, their risk increases for eye diseases and conditions such as age-related macular degeneration, cataracts, diabetic retinopathy, dry eye, glaucoma, and low vision. But vision loss is not inevitable; if eye diseases are detected and treated early, vision loss is often preventable (NEI, n.d.). It is estimated that by 2050 the number of Americans with age-related eye diseases will double. Many eye diseases have no early signs or symptoms to warn people but they can be detected in their early states by a comprehensive dilated eye exam done by an eyecare professional (CDC, 2017f).
Blindness or vision problems are among the top ten disabilities among adults aged 18 and older. Vision loss has serious consequences for the individual as well as those who care for and about people who have compromised vision because it impedes the ability to read, drive, prepare meals, watch television, and attend to personal affairs. Reduced vision among mature adults has been shown to result in social isolation, family stress, and ultimately a greater tendency to experience other health conditions or die prematurely (CDC, 2017f).
Presbyopia is a common type of vision disorder that occurs naturally in people as they age. It results in the inability to focus up close and is associated with refraction (bending of light) in the eye. Presbyopia is easily corrected with glasses (NEI, 2010).
Eye Anatomy: Normal and with Presbyopia
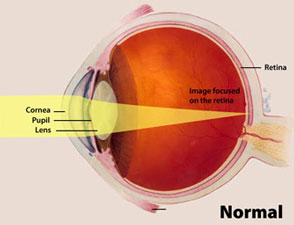
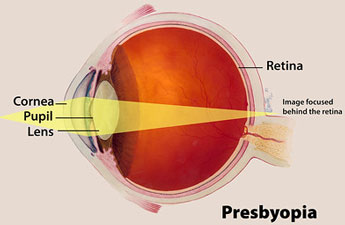
Source: National Eye Institute, National Institutes of Health.
Age-Related Macular Degeneration (AMD) is a common eye condition and a leading cause of vision loss among people age 50 and older. It causes damage to the macula, a small spot near the center of the retina and the part of the eye needed for sharp, central vision, which lets people see objects that are straight ahead. In some cases, AMD advances so slowly that people notice little change in their vision. In others, the disease progresses faster and may lead to a loss of vision in one or both eyes (NEI, 2018).
Normal Vision and Effect of Macular Degeneration

Source: National Eye Institute, National Institutes of Health.
A cataract is a clouding of the lens in the eye that affects vision and generally is related to aging. By age 80, more than half of all Americans either have a cataract or have had cataract surgery. A cataract can occur in one or both eyes and cannot spread from one eye to the other (NEI, 2015).
With age, some of the protein that makes up the lens may clump together and start to cloud a small area of the lens, causing a cataract. Over time the cataract may grow larger and cloud more of the lens. Researchers suspect that there are several causes of cataract (eg, smoking, diabetes) or it may be that the protein in the lens changes from the wear and tear it takes over the years (NEI, 2015).
Glaucoma is a group of diseases that damage the eye’s optic nerve and can result in vision loss and blindness. However, with early detection and treatment, serious vision loss may be prevented (NEI, 2015b).
Drainage System of the Eye
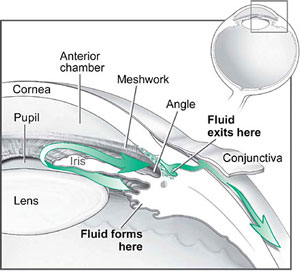
Source: NIH, n.d.
Several large studies have shown that eye pressure is a major risk factor for optic nerve damage. In the front of the eye is a space called the anterior chamber. Aqueous humor flows continuously in and out of the chamber and nourishes nearby tissues. The fluid leaves the chamber at the open angle where the cornea and iris meet. When the fluid reaches the angle, it flows through a spongy meshwork, like a drain, and leaves the eye.
In open-angle glaucoma, even though the drainage angle is “open,” the fluid passes too slowly through the meshwork drain. Since the fluid builds up, the pressure inside the eye rises to a level that may damage the optic nerve. When the optic nerve is damaged from increased pressure, open-angle glaucoma and vision loss may result. That’s why controlling pressure inside the eye is important.
Another risk factor for optic nerve damage relates to blood pressure. Thus, it is important to make sure general blood pressure remains at a proper level (NEI, 2015b).
Visual Result of Glaucoma

Normal vision and vision impaired by glaucoma. Source: National Eye Institute, National Institutes of Health.
Diabetic retinopathy is the most common diabetic eye disease and a leading cause of blindness among working-age adults. It is caused by changes in the blood vessels of the retina (NEI, 2015c). Diabetic retinopathy can cause blood vessels in the retina to leak fluid or hemorrhage, distorting vision. In its most advanced stage, new abnormal blood vessels proliferate on the surface of the retina, which can lead to scarring and cell loss in the retina (NEI, 2015c).
Visual Result of Diabetic Retinopathy

Normal vision and vision impaired by diabetic retinopathy. Source: National Eye Institute, National Institutes of Health.
Optic nerve atrophy in older adults is most commonly caused by poor blood flow, which damages the optic nerve. Vision becomes dim, the field of vision is reduced, the ability to see fine detail is lost, and colors seem faded. Over time the pupil is less able to react to light and may eventually completely lose that ability. Damage to the optic nerve is permanent and treatment consists of treating the underlying cause and preventing further damage, as well as protecting the other eye (Medline Plus, 2018f).
It is important for older adults to have yearly eye exams to detect problems in the early stages. Blood pressure should be monitored and exercise and a healthy diet are important. Smoking and sun exposure have been linked to both cataracts and macular degeneration. Sunglasses with 100% UVA and UVB protection should be worn.
Recent research has found that vision loss precedes loss of mental capacity and suggests that maintaining eye health could help protect cognition in older adults, lending more urgency to the need to protect vision as we age (Zheng et al., 2018).
Smell and Taste
Smell and taste are closely linked in the brain, but they are actually distinct sensory systems. True tastes are detected by taste buds on the tongue and the roof of the mouth, as well as in the throat region, and are limited to sweet, salty, sour, bitter, savory—and perhaps a few other sensations. The loss of smell is much more common than the loss of taste, and many people mistakenly believe they have a problem with taste, when they are really experiencing a problem with their sense of smell.
Our sense of smell helps us enjoy life and is also a warning system that alerts to danger signals such as a gas leak, spoiled food, or a fire. Any loss in our sense of smell can have a negative effect on our quality of life. It can also be a sign of more serious health problems.
Roughly 1% to 2% of people in North America say that they have a smell disorder. Problems with the sense of smell increase with age and are more common in men than women. In one study, nearly one-quarter of men ages 60 to 69 had a smell disorder, while about 11% of women in that age range reported a problem. Many people who have smell disorders also notice problems with their sense of taste (NIDCD, 2017).
Sense of smell that declines with age is called presbyosmia and is not preventable.
Age is only one of the many reasons for problems with smell. Most people who develop a problem with smell have recently had an illness or injury. The most common causes are the common cold and chronic nasal or sinus infection.
Problems with the sense of smell can also be a sign of other serious health conditions. A smell disorder can be an early sign of Parkinson’s disease, Alzheimer’s disease, multiple sclerosis, and (rarely) brain tumor. It can also accompany or be a sign of obesity, diabetes, hypertension, and malnutrition.
When smell is impaired, people often change their eating habits. Some may eat too little and lose weight while others may eat too much and gain weight. Food becomes less enjoyable and people may use too much salt or sugar to improve the taste, a practice that can worsen certain medical conditions such as high blood pressure, kidney disease, or diabetes. In severe cases, loss of smell can lead to depression.
It is important to identify and treat the underlying cause of a smell disorder. Certain antibiotics, some blood pressure pills, some cholesterol-lowering drugs, and some antifungal medications can cause problems with smell. The sense of smell usually returns to normal when the medicine is stopped.
Surgery to remove nasal obstructions such as polyps can restore airflow. Some people recover their ability to smell when the illness causing their olfactory problem is resolved. Occasionally, a person may recover the sense of smell spontaneously.
People with head and neck cancers who receive radiation treatment to the nose and mouth commonly experience problems with their sense of smell and taste as a side effect. Older people who have lost their larynx (voice box) commonly complain of poor ability to smell and taste (NIDCD, 2017; NIA, 2015).
Nineteen percent of Americans over age 40 report some alteration in their sense of taste, and this rises to 27% in people age 80 and older. About 5% of Americans experience dysgeusia, an often-persistent problem in which tastes are distorted; a majority (64%) of sufferers are women (NIDCD, 2019).
Chewing, drinking, and digesting foods releases tiny molecules that stimulate special sensory cells in the mouth and throat. Taste cells are clustered in the taste buds located mainly on the tongue, roof of the mouth, and the lining of the throat. Taste cells respond to at least one of five basic taste qualities: sweet, sour, bitter, salty and umami (savory). When people are born they have about 10,000 taste buds but may start to lose them after age 50 (NIDCD, 2017a; NIA, 2015).
Taste quality works in conjunction with another mechanism called the common chemical sense, which involves nerve endings on the moist surfaces of the eyes, nose, mouth, and throat that let you experience things like the coolness of mint or the burning of chili peppers. Other nerves create sensations of heat, cold, and texture. All of these work together with a food’s aroma to produce the perception of flavor, which allows one to distinguish one food from another (NIDCD, 2017a).
When people chew food, it releases aromas that activate the sense of smell by way of a channel connecting the roof of the throat to the nose. If a stuffy nose or other condition is blocking the channel, odors don’t reach the nose’s sensory cells and much enjoyment of flavor is lost, making food seem bland and flavorless. Most of the time when people think they have a taste disorder they actually have a smell disorder (NIDCD, 2017a).
The most common taste disorder is phantom taste perception. A reduced ability to taste the five qualities affects some people, and some cannot detect any tastes but that is a rare condition. Some people are born with tasted disorders but most begin after an injury or illness. Causes can include:
- Upper respiratory and middle ear infections
- Radiation therapy for cancers of the head and neck
- Exposure to certain chemicals, such as insecticides and some medications, including some common antibiotics and antihistamines
- Head injury
- Some surgeries to the ear, nose, and throat (such as middle ear surgery) or extraction of the third molar (wisdom tooth)
- Poor oral hygiene and dental problems.
Touch
Touch is the first sense that babies develop in the womb and it is necessary for the continued physical and emotional development of humans. Studies have shown that children deprived of human touch were more likely to become aggressive and violent than children raised with a loving and nurturing parent. Massage therapy has been shown to be beneficial in reducing anxiety and decreasing episodes of defiance in adolescents with behavioral disorders.
The sense of touch allows one to be aware of pain, temperature, pressure, vibration, and body position. Nerve endings (receptors) in skin, muscles, tendons, joints, and internal organs detect these sensations. Sensations can be reduced or changed with aging. Sometimes this is due to decreased blood flow to the nerve endings or the spinal cord or brain, which transmit and interpret signals from the nerves. Various health problems can also affect sensation changes, including lack of certain nutrients, brain surgery, brain problems, confusion, or nerve damage from injury or chronic diseases such as diabetes (MedlinePlus, 2018g).
Changed sensations vary but can have a variety of negative effects, some particularly relevant to elders. A decreased sensitivity to temperature that makes it hard to distinguish between cool and cold or hot and warm can make a person more susceptible to frostbite, hypothermia, and burns. A decreased sensitivity to vibration, touch, or pressure increases the risk from pressure ulcers, while decreased pain sensitivity may mislead one into thinking an injury is not as severe as it actually is. Walking problems and fall risk increase if a person develops a reduced ability to understand where their body is in relation the floor (MedlinePlus, 2018g).
Sleep Changes
Sleep disorders are common in older adults and involve any disrupted sleep pattern, including problems falling or staying asleep, too much sleep, or abnormal behaviors with sleep. All adults need about the same amount of sleep—seven to eight hours per night—but older adults sleep less deeply and experience choppier sleep than younger people. A healthy 70-year-old may wake up several times per night without any connection to a disease.
Sleep disturbances in older adults can be due to:
- Alzheimer’s disease
- Alcohol
- Changes in the body’s natural internal clock, causing some people to fall asleep earlier in the evening
- Long-term (chronic) disease, such as heart failure
- Certain medicines, herbs, supplements, and recreational drugs
- Depression (depression is a common cause of sleep problems in people of all ages)
- Brain and nervous system conditions
- Being inactive
- Pain caused by diseases such as arthritis
- Stimulants such as caffeine and nicotine
- Frequent urination at night (MedlinePlus, 2018h)
Sleep patterns tend to change with age and most people find that they have a harder time falling asleep, wake more often during the night, and awaken earlier in the morning. Even though total sleep need doesn’t really change, if it is harder to fall asleep—then total time in bed may increase. Older people often wake up more abruptly and so feel they have become lighter sleepers. Older people spend less time in deep, dreamless sleep so they wake up more often—3 to 4 times per night on average. They are also more aware of being awake. These factors can make them feel sleep-deprived even if the amount of time asleep has not materially changed (MedlinePlus, 2018i).
Sleep problems are annoying and sleep deprivation contributes to accidents and depression. It can even cause confusion and mental changes, but fortunately, it is treatable and symptoms reduce with enough sleep. Sleep problems are also a common symptom of depression and it is best to see a healthcare provider to rule out depression and other health conditions as a cause. Most sleep disorders have treatments available and sleep medicines in particular may not be advisable for older patients, so seeing a healthcare provider is always a good first step (MedlinePlus, 2018i).
The most common sleep problems are:
- Insomnia (one of the more common in older people)
- Other sleep disorders, such as restless legs syndrome, narcolepsy, or hypersomnia
- Sleep apnea, where breathing stops for a time during sleep (MedlinePlus, 2018i)
Insomnia is trouble falling asleep, staying asleep through the night, or waking up too early in the morning. It can be caused by poor sleep or lifestyle habits, use of some medicines or drugs, health problems, and social or mental health issues such as stress, anxiety, or depression (MedlinePlus, 2018j).
Restless legs syndrome is a common condition in older adults and affects more than 15% of people 80 years and older. People with RLS experience uncomfortable feelings in their legs such as tingling, crawling, or pins and needles that are alleviated by moving the leg. This often makes it hard for them to fall asleep or stay asleep, and causes them to be sleepy during the day.
Obstructive sleep apnea occurs when air entering from the nose or mouth is either partly or completely blocked, usually because of obesity or extra tissue in the back of the throat and mouth. If these episodes occur frequently or are severe, they may cause a person’s sleep to be fragmented throughout the night. This may result in their being sleepy during the day.
Psychosocial Changes
Loss
All older adults experience loss with aging—loss of social status and self-esteem, loss of physical capacities, and the death of friends and loved ones. The loss of a spouse is common in late life. About 800,000 older Americans are widowed each year and bereavement is a natural response to the death of a loved one. The death of a spouse can also result in financial difficulties and loss of social contacts. Its features, almost universally recognized, include crying and sorrow, anxiety and agitation, insomnia, and loss of appetite (Moen et al., 2000).
The losses experienced by older adults often occur over short periods of time. Experiencing more than one loss at a time or over a short period of time can cause prolonged grieving. An older people who experiences loss may feel numb and overwhelmed and may also lack the support systems they once had. But, in the face of loss, many older people have the capacity to develop new adaptive strategies, even creative expression. Those experiencing loss may be able to move in a positive direction, either on their own, with the benefit of informal support from family and friends, or with formal support from mental health professionals.
Social Roles
Social roles are important components of self-concept. Older adults face many challenges, including the loss of careers, loss of family members and friends, changes in physical and mental abilities, difficulties in accessing affordable and high-quality healthcare, decreased financial security, and decreasing opportunities to remain engaged in society (Cornwell, 2008).
Remaining socially integrated in society has many benefits for the older adult. Although the oldest old have a smaller social network, they tend to have more contact with the core group. Social networks are important for older adults because they provide resources—such as access to information and other resources—that are crucial for successful aging and social support (Cornwell, 2008).
As people age they may become more dependent on family members for care and support, and adult children may feel that there has been a role reversal, concerned that they have become their parent’s parent. But it is difficult for an older adult to give up a lifetime of independence and, like any other adult, they want their decisions to be respected. It is important, even with an older person who has dementia, to make collaborative decisions about care, living arrangements, and outside help when needed.
