No clinician working alone, regardless of how talented, can prevent all falls. Rather, fall prevention requires the active engagement of many individuals, including the multiple disciplines and teams involved in caring for the patient.
Preventing Falls in Hospitals (AHRQ, 2018)
Patient Falls
Fall prevention is a matter of concern with elders whether they are in hospitals or other institutions, out in public places, or in their own homes. Prevention “requires the active engagement of many individuals” in every situation and that includes the individual, their caregivers, and their healthcare providers (AHRQ, 2018). According to AHRQ, a patient fall is defined as “an unplanned descent to the floor with or without injury to the patient.” Such falls can result in fractures, lacerations, or internal bleeding, requiring additional healthcare. Research has shown that close to one-third of falls are preventable (AHRQ, 2018).
Falls happen for a number of reasons including:
- Person is weak, tired or ill
- Person is not physically fit
- Person may have problems seeing
- Medicines may cause weakness, sleepiness, confusion or dizziness
- Slippery or wet floors or stairs
- Obstructed pathways
- Darkness (Joint Commission, 2018)
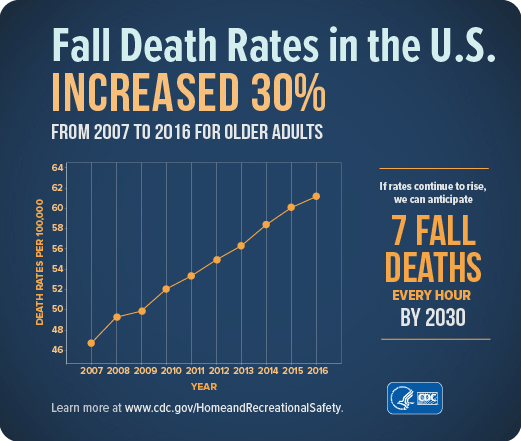
Treating fall injuries is very costly. In 2015 medical costs for falls totaled more than $50 billion. Because the U.S. population is aging, both the number of falls and the costs to treat fall injuries are likely to rise. Every year 3 million older people are treated in EDs because of falls and over 800,000 patients are hospitalized because of a fall injury—most commonly broken hips and head injuries (CDC, 2017h, 2016c).
The average hospital cost for a fall injury is more than $30,000 and the costs go up with age. In 2015 total medical costs for falls were more than $50 billion and Medicare and Medicaid shouldered 75% of these costs (CDC, 2017h).
Falls Resulting in Death
Preventing Patient Falls
Falls within care settings are especially concerning. The Joint Commission Center for Transforming Healthcare notes that hundreds of thousands of patients fall in hospitals every year and 30% to 35% experience an injury. The estimated average cost for a fall with injury is about $14,056 (JCC, 2019).
Hospital staff have a complex and potentially conflicting set of patient care goals. They need to treat the problem that prompted the patient’s admission, keep the patient safe, and help the patient to maintain or recover physical and mental function. Thus, fall prevention must be balanced against other priorities (AHRQ, 2018).
Fall prevention involves managing a patient’s underlying fall risk factors (eg, problems with walking and transfers, medication side effects, confusion, frequent toileting needs) while working within the hospital’s physical design and environment. A number of practices have been shown to reduce the occurrence of falls, but these practices are not used systematically in all hospitals (AHRQ, 2018).
Fall prevention requires an interdisciplinary approach to care. Some aspects of fall prevention care are highly routinized, while others must be tailored to each patient’s specific situation. Fall prevention requires the active engagement of all the multiple disciplines and teams involved in caring for the patient. This sort of coordination for high-quality prevention requires an organizational culture and operational practices that promote teamwork and communication, as well as individual expertise (AHRQ, 2018).
Fall prevention activities also need to be balanced with other considerations, such as minimizing restraints and maintaining patients’ mobility, to provide the best possible care to the patient. Therefore, improvement in fall prevention requires a system focus to make needed changes (AHRQ, 2018).
What can individuals do to reduce their risk of falls? The Joint Commission provides guidelines targeted toward patients at home and in hospitals or nursing facilities.
At-home guidelines include:
- Turn on the lights when you enter a room. Do not walk in the dark.
- Make sure your pathway is clear.
- Use the handrails on staircases.
- Sit in chairs that do not move and have arm rests to help when you sit down and stand up.
- Wear shoes that have firm, flat, non-slip soles. Avoid shoes that do not have backs on them.
- Replace the rubber tips on canes and walkers when they become worn. (Joint Commission, 2018)
In-patient guidelines include:
- Use your call button to ask for help getting out of bed if you feel unsteady.
- Ask for help going to the bathroom or walking around the room or in hallways.
- Wear non-slip socks or footwear.
- Lower the height of the bed and the side rails.
- Talk to your doctor if your medicine makes you sleepy, light-headed, sluggish or confused. Ask how to reduce these side effects or if you can take another medicine. (Joint Commission, 2018)
Agency for Healthcare Research and Quality
The AHRQ’s text, Patient Safety and Quality: An Evidence-Based Handbook for Nurses, released in 2008, includes a chapter specific to patient falls in various care settings, with a discussion of fall risk assessment tools and prevention strategies (see table below) (Currie, 2008).
Recommendations for Acute and Long-Term Care |
|
|---|---|
Evidence-based practice recommendations |
Research implications |
Fall Prevention |
|
|
|
Injury prevention |
|
|
|
Also, updated in 2018 was AHRQ’s Preventing Falls in Hospitals: A Toolkit for Improving Quality of Care, which discusses the development of a complete program for hospitals, including such practices as rounding protocols (AHRQ, 2018).
Joint Commission Center for Transforming Healthcare
The Joint Commission released its Targeted Solutions Tool for Patient Falls with Injury in August 2015. The tool is an innovative application that guides healthcare organizations through a step-by-step process to accurately measure their organization’s actual performance, identify their barriers to excellent performance, and direct them to proven solutions that are customized to address their particular barriers. According to the Commission, organizations that followed its standardized approach reduced the rate of patient falls by 35% and falls with injury by 62% (JCC, 2019).
Tens of thousands of patients fall in healthcare facilities every year and many of these falls result in moderate to severe injuries. Find out how the participants in the Center for Transforming Healthcare’s seventh project are working to keep patients safe from falls.
CDC’s STEADI: Older Adult Fall Prevention
CDC created the evidence-based STEADI (Stopping Elderly Accidents, Deaths, and Injuries) initiative to help healthcare providers incorporate fall prevention into routine care for older adults. STEADI provides screening tools, guidelines for talking with patients, assessment forms and procedures, a medication review framework, educational materials and resources, handouts to give to patients, and online trainings for healthcare providers. Information can be accessed on the CDC’s STEADI website (CDC, 2016d).
The CDC says that when healthcare professionals see a patient 65 and older they should always ask these three questions:
- Have you fallen in the past year?
- Do you feel unsteady when standing or walking?
- Do you worry about falling?
A yes answer to any of these questions indicates an increased risk of falling and further assessment is recommended. Falls are not an inevitable part of aging. Healthcare providers can help a patient reduce their chances of falling by identifying the risk level, identifying modifiable risk factors, and offering effective interventions (CDC, 2019b).
