Here I lie in my hospital bed
Tell me, sister morphine, when are you coming round again?
Oh, I don’t think I can wait that long
Oh, you see that my pain is so strong
The scream of the ambulance is soundin’ in my ear
Tell me, sister morphine, how long have I been lying here?
What am I doing in this place?
Why does the doctor have no face?
Marianne Faithfull, Sister Morphine
The United States is in the midst of an unprecedented drug overdose epidemic. Since 1999 prescription drug overdose death rates have quadrupled (CDC, 2016b). In 2009, for the first time in U.S. history, drug overdose deaths outnumbered motor vehicle deaths (CDC, 2013a). Since pain was coined “the fifth vital sign” in the 1990s, sales of prescription opioids in the Unites States have quadrupled (see below) (Bartels et al., 2016).
Source: CDC, 2016b.
This increase in the prescription of opioids for pain management has been accompanied by a dramatic rise in prescription opioid-associated morbidity and mortality. In 2010 more than 16,000 deaths were attributed to prescription opioids, making them a leading cause of injury death in the general population (Bartels et al., 2016). There are now more deaths from opioid-related overdoses than from all other illicit drugs combined. Emergency department visits, substance treatment admissions, and economic costs associated with opioid abuse have all soared (CDC, 2013a).
Some startling statistics illustrate the magnitude of the abuse problem. Between 1997 and 2011 the U.S. population increased only 16%, however the number of prescription pain medications sold by pharmacies increased significantly more than that. Between 1997 and 2011:
- Oxycodone sales increased by 1,259%
- Hydrocodone sales increased by 356%
- Methadone sales increased by 1,099%
- Fentanyl sales increased by 711%
- Morphine sales increased by 246%
- Buprenorphine sales increased from 17 grams in 2002 to 1,639 kg in 2011 (McDonald & Carlson, 2013)
USA Opioid Consumption (mg/capita), 2000–2014
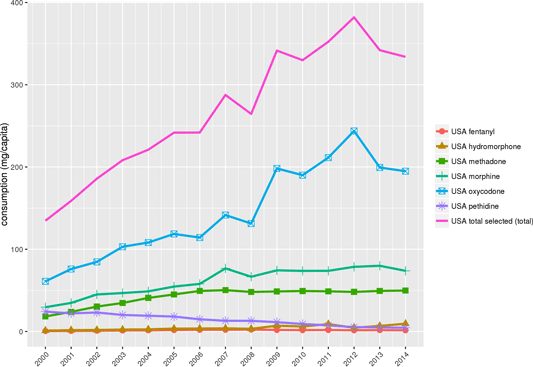
Sources: International Narcotics Control Board; World Health Organization population data
By: Pain and Policy Studies Group, University of Wisconsin/WHO Collaborating Center, 2016.
The increased availability of opioid analgesics means they are being used in ways that are unsafe or unintended. OxyContin, for example, which was designed as a slow-release, oral medication is now being crushed, then snorted or injected, with lethal consequences. To combat this, new formulations are being designed to deter some of these abuses. For example, a new formulation of OxyContin releases from 21% to 48% less opioid when tampered with (milled, manually crushed, dissolved, and boiled) than the original version (Raffa et al., 2012).
Paradoxically, despite an enormous rise in spending and prescription, there is limited evidence to support the efficacy of opioids in chronic noncancer pain management. In a European survey on chronic pain, 15% of respondents felt that their medications were not very, or not at all, effective (Xu & Johnson, 2013). A systematic review by Chou and colleagues suggested limited efficacy of long-term opioid therapy over short-term treatment or placebo, while an evidence review by the Institute of Medicine concluded that the effectiveness of opioids as pain relievers, especially over the long term, is somewhat unclear (Xu & Johnson, 2013).
A survey of pain management in sixteen European countries conducted in 2003 found that 28% of survey respondents used prescription opioids. Of particular interest, the countries reporting higher percentage of opioid use were no more satisfied with their pain control than those with lower prevalence of use (Xu & Johnson, 2013).
Prescribing rates for opioids vary widely across states. In 2012 healthcare providers in the highest-prescribing state wrote almost 3 times as many opioid painkiller prescriptions per person as those in the lowest prescribing state (CDC, 2016b). Health issues that cause people pain do not vary much from place to place, and do not explain this variability in prescribing. Some factors that may influence prescribing rates include:
- Healthcare providers in different parts of the country do not agree on when to prescribe opioid painkillers and how much to prescribe.
- Some of the increased demand for prescription opioids is from people who use them non-medically, who sell them, or who obtain them from multiple prescribers.
- Many states report problems with for-profit, high-volume pain clinics (so-called pill mills) that prescribe large quantities of painkillers to people who don’t need them medically (CDC, 2016b).
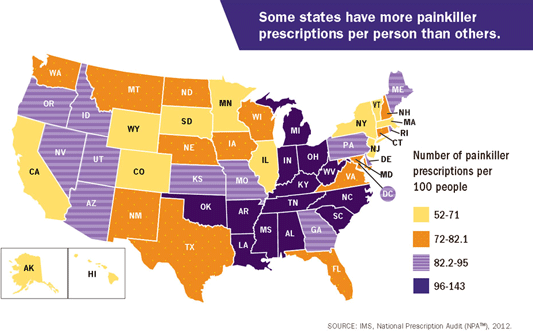
CDC, 2016b
Prescription Drug Abuse
Prescription drug abuse is the use of a medication without a prescription, in a way other than as prescribed, or for the experience or feelings elicited. According to several national surveys, prescription medications, such as those used to treat pain, attention deficit disorders, and anxiety, are being abused at a rate second only to marijuana among illicit drug users. The consequences of this abuse have been steadily worsening, reflected in increased treatment admissions, emergency room visits, and overdose deaths (NIDA, 2014b).
Prescription drug abuse can include taking a drug prescribed for someone else, taking more of the medication than was prescribed, taking medication more frequently than was directed, or altering the formulation (crushing, snorting) so as to obtain a greater amount of active agent than was originally intended (NIDA, 2012b).
Opioid pain medication use presents serious risks, including overdose and opioid use disorder. From 1999 to 2014, more than 165,000 persons died from overdose related to opioid pain medication in the United States. In the past decade, while the death rates for the top leading causes of death such as heart disease and cancer have decreased substantially, the death rate associated with opioid pain medication has increased markedly. Sales of opioid pain medication have increased in parallel with opioid-related overdose deaths. The Drug Abuse Warning Network estimated that >420,000 ED visits were related to the misuse or abuse of narcotic pain relievers in 2011, the most recent year for which data are available (CDC, 2016a).
Although clinical criteria have varied over time, opioid use disorder is a problematic pattern of opioid use leading to clinically significant impairment or distress. This disorder is manifested by specific criteria such as unsuccessful efforts to cut down or control use and use resulting in social problems and a failure to fulfill major role obligations at work, school, or home. This diagnosis has also been referred to as “abuse or dependence” and “addiction” in the literature, and is different from tolerance (diminished response to a drug with repeated use) and physical dependence (adaptation to a drug that produces symptoms of withdrawal when the drug is stopped), both of which can exist without a diagnosed disorder (CDC, 2016a).
In 2013, on the basis of DSM-IV diagnosis criteria, an estimated 1.9 million people abused or were dependent on prescription opioid pain medication. Having a history of a prescription for an opioid pain medication increases the risk for overdose and opioid use disorder, highlighting the value of guidance on safer prescribing practices for clinicians. For example, a recent study of patients aged 15 to 64 years receiving opioids for chronic noncancer pain and followed for up to 13 years revealed that 1 in 550 patients died from opioid-related overdose at a median of 2.6 years from their first opioid prescription, and 1 in 32 patients who escalated to opioid dosages >200 morphine milligram equivalents (MME) died from opioid-related overdose (CDC, 2016a).
Did You Know. . .
Enough prescription painkillers were prescribed in 2010 to medicate every American adult around-the-clock for one month (CDC, n.d.).
Several factors have been put forth to explain the rise in opioid prescriptions for chronic noncancer pain that began in the 1980s and became dominant one decade later:
- Reservations against alternative pain therapies, especially those related to adverse events associated with long-term use of NSAIDs
- Aggressive and, at times, misleading product marketing by the manufacturers
- A widespread belief that opioid therapy carries a low risk of addiction potential (Xu & Johnson, 2013)
Overdose and Poisoning
Poisoning is now the leading cause of death from injuries in the United States, and nearly 9 out of 10 poisoning deaths are caused by drugs.
Margaret Warner, 2011
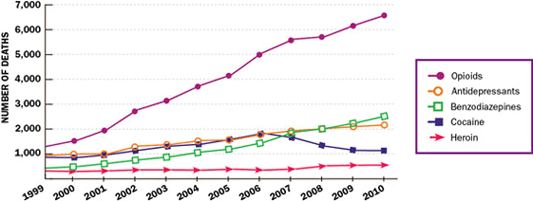
From 1999 to 2011, the age-adjusted rate for opioid-analgesic poisoning deaths nearly quadrupled. However, the increase in rates seems to be slowing. For opioid-analgesic poisoning deaths, there was an 18% increase each year from 1999 through 2006 but only a 3% increase each year from 2006 through 2011 (NCHS, 2014).
Deaths from opioid analgesics often involve other drugs. Benzodiazepines have been reported frequently in deaths involving opioid analgesics. Over the past decade, there has been an upward trend in the presence of benzodiazepines in opioid-analgesic poisoning deaths. In 1999 benzodiazepines were involved in 13% of the opioid analgesic poisoning deaths; by 2011, 31% of the opioid analgesic-related drug-poisoning deaths also involved benzodiazepines (NCHS, 2014).
Age-adjusted drug-poisoning and opioid-analgesic poisoning death rates: United States, 1999–2011
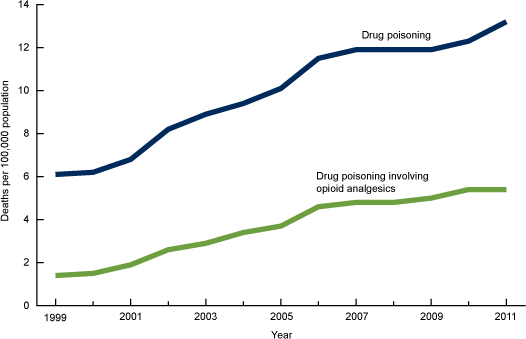
Source: NCHS, 2014.
Intertwined Epidemics: Prescription Opioids and Heroin
The enormous increase in the availability of prescription pain medications is drawing new users to these drugs and changing the geography and age-grouping of opiate-related overdoses. Prescription opioid-related overdoses currently represent the second leading cause of injury-related death in the United States and the leading cause of death for 35- to 54-year-olds. This has led to an increase in healthcare utilization that is troubling for both its high social and healthcare-related costs (Unick et al., 2013).
While many drugs and medicines have potential for overdose, the use of both prescription opioids and heroin (often taken in combination with other medicines and drugs) has increased since 1999. With increased use of opioids, communities have seen increases in overdose hospitalizations and deaths and need for treatment. Data on the sales of legally prescribed medicines (opioids in particular) and data on overdose hospitalizations and deaths can be used to illustrate the progression of an epidemic of overdose hospitalizations and deaths (OHA, 2014).
Most of the current cases of opioid-related overdoses can be traced to two fronts: (1) illegal heroin consumption, and (2) the illicit use or misuse of prescription opioids. Given the differences in the sources of opioids and the financial and social costs associated with overdose cases, it is important to understand the dynamics of the opioid-related overdose epidemic and the changing characteristics of opiate abusers (Unick et al., 2013).
The rise in prescription opioid-related overdose deaths has been particularly alarming in rural areas; between 1999 and 2004 prescription opioid-related overdose deaths increased 52% in large urban counties and a staggering 371% in non-urban counties (Unick et al., 2013).
Significant increases in drug overdose death rates were seen in the Northeast, Midwest and South census regions. In 2014 the five states with the highest rates of death due to drug overdose were West Virginia, New Mexico, New Hampshire, Kentucky, and Ohio. States with statistically significant increases in the rate from 2013 to 2014 included Alabama, Georgia, Illinois, Indiana, Maine, Maryland, Massachusetts, Michigan, New Hampshire, New Mexico, North Dakota, Ohio, Pennsylvania, and Virginia (CDC, 2016b).
Drug Overdose Increase, 2013–2014
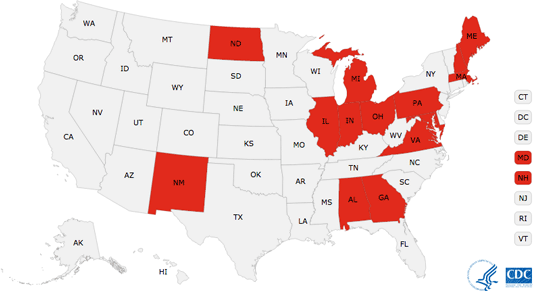
Statistically significant drug overdose death rate increase from 2013 to 2014, U.S. states.
There is an evolving flux between prescription opioid use and heroin use in urban areas. Ethnographic work from Montreal shows that individuals at risk for heroin use have begun shifting to injecting prescription opioids. Additional evidence from Baltimore and Washington State suggests a high prevalence of prescription abuse in injection drug using populations, often preceding heroin use. Interestingly, recent changes to the formulation of OxyContin, the brand name long-acting form of oxycodone, have been linked to a self-reported rise in heroin use. What these studies suggest is that prescription opioid misuse and heroin use are intertwined (Unick et al., 2013).
Abuse Among Adolescents and Young Adults
Adolescents and young adults are especially vulnerable to prescription drug abuse, particularly opioids and stimulants. According to the Monitoring the Future (MTF) survey, an ongoing study of the behavior and attitudes of American youth involving nearly 45,000 8th, 10th, and 12th grade students, with regard to illicit drugs, annual prevalence declined for synthetic marijuana, heroin, MDMA (ecstasy, Molly), sedatives, and nonmedical use of any prescription drug. Annual prevalence of using any illicit drug remained essentially unchanged in all three grades in 2015 (Johnston et al., 2015).
Psychotherapeutic drugs now make up a significantly larger part of the overall U.S. drug problem than was true 10 to 15 years ago. This is in part because use increased for many prescription drugs over that period, and in part because use of a number of street drugs has declined substantially since the mid- to late-1990s. It seems likely that young people are less concerned about the dangers of using these prescription drugs outside of medical regimen because they are widely used for legitimate purposes. (Indeed, the low levels of perceived risk for sedatives and amphetamines observed among 12th graders illustrate this point.) Also, prescription psychotherapeutic drugs are now being advertised directly to the consumer, which implies that they are both widely used and safe to use. Fortunately, the use of most of these drugs has either leveled or begun to decline in the past few years. The proportion of 12th graders misusing any of these prescription drugs (eg, amphetamines, sedatives, tranquilizers, or narcotics other than heroin) in the prior year continued to decline in 2015 down from its high in 2005 (Johnston et al., 2015).
Amphetamine use without a doctor’s orders—currently the second most widely used class of illicit drugs after marijuana—continued a gradual decline in 2015 in all grades, though the one-year declines did not reach statistical significance. Use of narcotics other than heroin without a doctor’s orders (measured only in 12th grade) also continued a gradual decline begun after 2009 (Johnston et al., 2015).
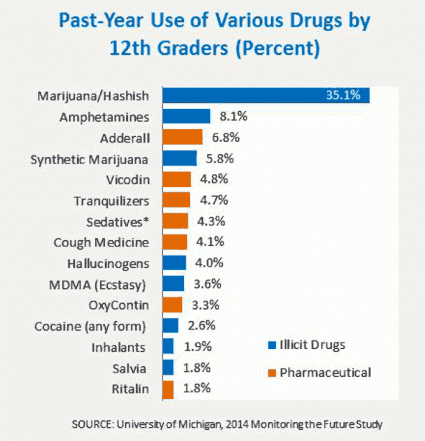
Source: National Institute on Drug Abuse, 2015.
Abuse Among Middle-Aged and Older Adults
Prescription opioid-related overdoses rates are increasing the most in middle-aged individuals. Older adults represent another area of concern. Although older adults currently comprise just 13% of the population, they account for more than one-third of total outpatient spending on prescription medications in the United States. Older patients are more likely to be prescribed long-term and multiple prescriptions, which could lead to misuse or abuse (NIDA, 2014b).
The high rates of comorbid illnesses in older populations, age-related changes in drug metabolism, and the potential for drug interactions may make any of these practices more dangerous than in younger populations. Further, a large percentage of older adults also use over-the-counter medicines and dietary supplements, which (in addition to alcohol) could compound any adverse health consequences resulting from prescription drug abuse (NIDA, 2014b).
Gender Differences in Opioid Abuse
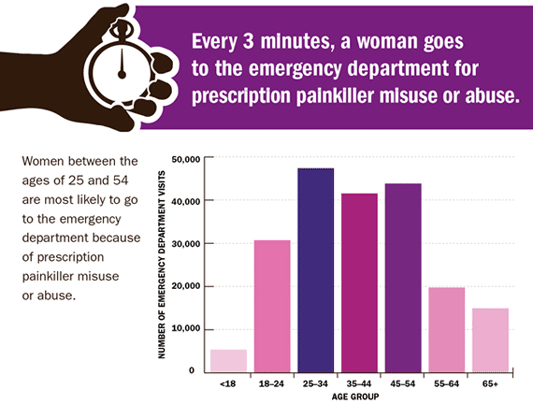
Overall, adult men and women have roughly similar rates of nonmedical use of prescription drugs, although some studies suggest that women are more likely than men to be prescribed prescription drugs, particularly narcotics and anti-anxiety drugs. Adolescent females are more likely than males to use psychotherapeutic drugs nonmedically. Research has also suggested that women are at increased risk for nonmedical use of narcotic analgesics and tranquilizers such as benzodiazepines (CDC, 2013b).
Prescription pain medication overdoses are increasing among women. Although men are still more likely to die of prescription painkiller overdoses (more than 10,000 deaths in 2010), the gap between men and women is closing. Deaths from prescription painkiller overdose among women have risen more sharply than among men; since 1999 the percentage increase in deaths was more than 400% among women compared to 265% in men. This rise relates closely to increased prescribing of these drugs during the past decade (CDC, 2013b).
Deaths of Women from Prescription Painkillers, 1999–2010
Prescription painkiller deaths among women have increased dramatically since 1999. Source: CDC, 2013b.
Prescription Painkillers: Growing Problem Among Women
- More than 5 times as many women died from prescription painkiller overdoses in 2010 than in 1999.
- Women between the ages of 25 and 54 are more likely than other age groups to go to the emergency department from prescription painkiller misuse or abuse.
- Women ages 45 to 54 have the highest risk of dying from a prescription painkiller overdose.*
- Non-Hispanic white and American Indian or Alaska Native women have the highest risk of dying from a prescription painkiller overdose.
- Prescription painkillers are involved in 1 in 10 suicides among women.
*Death data include unintentional, suicide, and other deaths. Emergency department visits only include suicide attempts if an illicit drug was involved in the attempt.
Prescription Painkillers Affect Women Differently than Men
- Women are more likely to have chronic pain, be prescribed prescription painkillers, be given higher doses, and use them for longer time periods than men.
- Women may become dependent on prescription painkillers more quickly than men.
- Women may be more likely than men to engage in “doctor shopping” (obtaining prescriptions from multiple prescribers).
- Abuse of prescription painkillers by pregnant women can put an infant at risk. Cases of neonatal abstinence syndrome (NAS)—which is a group of problems that can occur in newborns exposed to prescription painkillers or other drugs while in the womb—grew by almost 300% in the United States between 2000 and 2009.
Source: CDC, 2013b.
Source: CDC.
Opioid Abuse and Chronic Pain
Diagnosed chronic pain patients make up less than 1% of the insured population in the United States but consume about 45% of all prescription opioids. It has been estimated that up to 40% of pain patients on chronic opioid therapy display aberrant drug-related behaviors (Raffa et al., 2012).
Chronic pain is defined as pain that typically lasts >3 months or past the time of normal tissue healing. Chronic pain can be the result of an underlying medical disease or condition, injury, medical treatment, inflammation, or an unknown cause (CDC, 2016b).
Prevention, assessment, and treatment of chronic pain are challenges for health providers and systems. Pain might go unrecognized, and patients, particularly members of racial and ethnic minority groups, women, elders, people with cognitive impairment, and those with cancer and at the end of life, can be at risk for inadequate pain treatment. Patients can experience persistent pain that is not well controlled. There are clinical, psychological, and social consequences associated with chronic pain including limitations in complex activities, lost work productivity, reduced quality of life, and stigma, emphasizing the importance of appropriate and compassionate patient care. Patients should receive appropriate pain treatment based on a careful consideration of the benefits and risks of treatment options (CDC, 2016b).
Chronic pain has been intertwined with substance abuse: 33% of individuals in a substance abuse program reported suffering from chronic pain and individuals in substance abuse treatment programs with chronic pain were significantly more likely to abuse opioids than those not reporting chronic pain. The term rational abuse has been put forth to describe chronic pain patients who abuse opioids because of undertreated pain, but very little is known about this population (Raffa et al., 2012).
Sales of opioid pain medication have increased in parallel with opioid-related overdose deaths. The Drug Abuse Warning Network estimated that >420,000 emergency department visits were related to the misuse or abuse of narcotic pain relievers in 2011, the most recent year for which data are available. Although clinical criteria have varied over time, opioid use disorder is a problematic pattern of opioid use leading to clinically significant impairment or distress (CDC, 2016b).
This disorder is manifested by specific criteria, such as unsuccessful efforts to cut down or control use, and use resulting in social problems and a failure to fulfill major role obligations at work, school, or home. This diagnosis has also been referred to as “abuse or dependence” and “addiction” in the literature, and is different from tolerance (diminished response to a drug with repeated use) and physical dependence (adaptation to a drug that produces symptoms of withdrawal when the drug is stopped), both of which can exist without a diagnosed disorder (CDC, 2016b).
Abuse of Methadone
Methadone is a synthetic narcotic first developed by German scientists during World War II to address a shortage of morphine. Methadone was introduced into the United States in 1947 as an analgesic (Dolophinel) and has emerged as a commonly prescribed medication for the management of pain. Methadone is also used for the treatment of opioid dependence, in which case it may be dispensed only in federally approved opioid treatment programs.
Drug Enforcement Administration (DEA) data suggest that abuse of methadone diverted from its intended purpose has contributed significantly to the rise in overdose deaths. Some individuals who abuse other narcotics have turned to methadone because of its availability.
Methadone has been associated with disproportionate numbers of overdose deaths relative to the frequency with which it is prescribed for pain. Methadone has been found to account for as much as a third of opioid-related overdose deaths involving single or multiple drugs in states that participated in the Drug Abuse Warning Network, which was more than any opioid other than oxycodone, despite representing <2% of opioid prescriptions outside of opioid treatment programs in the United States; further, methadone was involved in twice as many single-drug deaths as any other prescription opioid (MMWR, 2016).
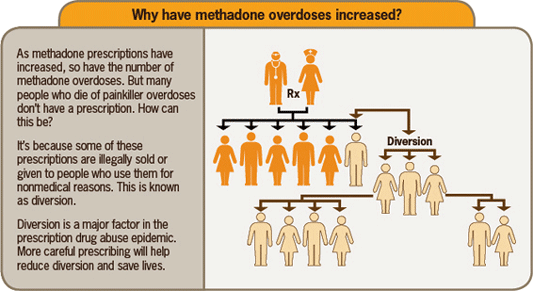
Source: CDC, 2012.
Methadone differs from most other opioids because of its long half-life, delayed onset, narrow therapeutic window, and interactions with drugs such as alcohol and benzodiazepines. Methadone is less expensive than other opioids and is increasingly being prescribed as a cost-effective alternative, partly due to pressure from insurance companies.
Abuse of Fentanyl
Fentanyl is a synthetic opioid analgesic that is similar to morphine but is 50 to 100 times more potent. It is a schedule II prescription drug, and it is typically used to treat patients with severe pain or to manage pain after surgery. It is also sometimes used to treat patients with chronic pain who are physically tolerant to other opioids.
Fentanyl can be absorbed through the skin (fentanyl patch), by IV injection, by mouth (for breakthrough cancer pain), and intranasally. There are two types of fentanyl:
- Pharmaceutical fentanyl, which is primarily prescribed to manage acute and chronic pain associated with advanced cancer
- Nonpharmaceutical fentanyl, which is illegally made, and is often mixed with heroin and/or cocaine—with or without the user’s knowledge—in order to increase the drug’s effect
A sharp increase has been noted in the number of fentanyl overdoses in recent years. Most of the increases in fentanyl deaths over the last three years do not involve prescription fentanyl but are related to illicitly made fentanyl that is being mixed with or sold as heroin—with or without the users’ knowledge—and increasingly as counterfeit pills. In July 2016, the DEA issued a new nationwide report indicating hundreds of thousands of counterfeit prescription pills have been entering the U.S. drug market since 2014, some containing deadly amounts of fentanyl and fentanyl analogs. The current fentanyl crisis continues to expand in size and scope across the United States (CDC, 2016b).
Number of Reported Law Enforcement Encounters Testing Positive for Fentanyl in the US: 2010–2015
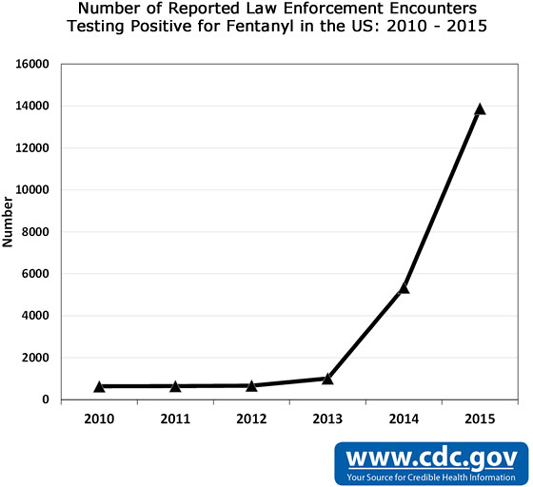
This graph uses data from the DEA National Forensic Laboratory Information System (NFLIS) on the number of law enforcement drug submissions that test positive for fentanyl from 2014 to 2015 as of July 1, 2016. Source: CDC.
Abuse of Buprenorphine (Subutex) and Suboxone
Buprenorphine (Subutex) and the combination of buprenorphine and naloxone (Suboxone) are used to treat opioid dependence. Buprenorphine alone and the combination of buprenorphine and naloxone work to prevent withdrawal symptoms when someone stops taking opioid drugs by producing similar effects to these drugs. In recent years, buprenorphine has surpassed methadone as a drug of diversion and abuse (Medline Plus, 2016).
Subutex, which contains only buprenorphine, is intended for use at the beginning of treatment. Suboxone, which contains both buprenorphine and naloxone (to decrease the potential for abuse by injection), and is used in the maintenance treatment of opiate addiction.
The National Forensic Laboratory Information System (NFLIS) collects results from law enforcement-encountered drug items submitted to and analyzed by state and local forensic laboratories across the country. In contrast to methadone, the number of buprenorphine reports in the year following its approval to treat opioid dependence increased from 90 in 2003 (one year after it was approved) to 10,537 in 2010. It has increased slowly each year since then, reaching a high of 11,992 in 2013 (CESAR, 2014).
In 2013 the majority of buprenorphine reports were from the Northeast United States census region, while the West had the lowest number (CESAR, 2014).
