The management of pain can be, and is, approached in a number of ways. Many people suffering from pain, particularly acute pain, successfully self-manage their pain. If this fails, a trip to primary care physician, emergency department, pain specialist, or complementary practitioner may help. If none of these solves the problem, surgery may be considered.
Broadly speaking, pain has been managed with either of two models: self-management or pain medicine. The self-management model—especially for chronic pain—is supported by strong evidence and has the benefit of involving patients in their own care. The pain medicine model, which includes primary and specialty care, is supported by relatively weak evidence, particularly in chronic pain care, and often fails to involve the recipient as an active participant. Although the pain medicine model has weaker demonstrated efficacy, it is widely used because of a strong business model, industry support, and focus of training in healthcare professionals (NIH, 2013).
Three Approaches to Pain Management
- The Self-Management Model
- The Pain Medicine Model
- The Integrative Medicine Model
Increasingly, however, pain medicine approaches are being combined with self-management and complementary practices into what is referred to as integrative medicine. In this model, pain is viewed holistically, and assessed and treated in conjunction with psychological, medical, social, spiritual, and environmental influences. Currently, an integrative approach to pain care is encouraged for all patients (PPSG, 2014b).
Self-Management of Pain
Self-management is defined as a strategy used by the patient to manage or minimize the impact of a chronic condition on everyday life. The basic tenets of self-management include:
- Active participation by the patient
- Treatment of the whole person, not just the disease
- Empowerment of the patient (NIH, 2013)
Although some people seek professional help immediately, most try to self-manage their pain. Self-management approaches include talking to friends, searching the internet, or attending group classes or programs intended to educate a person about pain management. Self-management also includes exercise, ice, heat, positioning, limiting activity, over-the-counter (OTC) medications, and education. In many cases, self-management is highly successful.
Pain Medicine Model
The pain medicine model is widely accepted and widely used. It is based upon the idea that pain is an acute, treatable disease. This approach usually begins with the primary care physician. Primary care physicians may make a referral to a pain specialist or pain clinic.
Primary Care
Primary care practitioners are an early step in the pain care journey, treating 52% of chronic pain patients in the United States based on a national mail survey of primary care physicians, physician pain specialists, chiropractors, and acupuncturists (IOM, 2011).
Primary care involves several management strategies, usually coordinated by a general medicine specialist. Primary care clinicians provide the initial assessment or diagnosis and serve as a starting point for specialty services, including prescription medications and referrals to imaging, physical and occupational therapy, or other integrative practitioners (IOM, 2011).
Once the primary care clinician has completed the initial assessment, effective medical management, especially with chronic pain, ideally involves a multi-disciplinary team. The development of a comprehensive treatment plan is important, utilizing appropriate pharmacologic and nonpharmacologic interventions. Treatments should be regularly re-evaluated for effectiveness, adjusted as needed, with side effects quickly addressed. The treatment plan should include a complete assessment and a clearly written plan of care (PPSG, 2014b).
Primary care clinicians assist patients in making decisions about specialty services and elective procedures. They are also responsible for the majority of pain medicine prescriptions. In 2007 analgesics were the drug category most frequently mentioned in data on office visits to physicians. In 2008 analgesics constituted 10.1% of all drugs prescribed for adults (ranking a close second to antidepressants, at 10.8%) (IOM, 2011).
Specialty Care
Specialty practice in pain management is a growing part of the medical profession, and the American Medical Association recognizes pain medicine as a discrete specialty. Most pain specialists come from anesthesiology, with a smaller number coming from physical and rehabilitation medicine, occupational medicine, psychiatry, and neurology (IOM, 2011). Physicians who are board certified in these specialty areas can become certified in pain medicine.
From 2000 to 2009, pain medicine certificates were issued to 1,874 anesthesiologists, 1,337 physiatrists, and 277 psychiatrists and neurologists, based on a common curriculum and a jointly developed examination administered by the American Board of Anesthesiology (IOM, 2011).
Acute Pain Services
Many hospitals have developed acute pain services (APS), the goal of which is to provide consistent pain management for individual patients throughout the course of their hospital stay. Hospitals with formally organized acute pain services are more likely to follow a formal written post operative pain protocol than hospitals without acute pain services (Nasir et al., 2011).
A survey of the structure and function of acute pain services in 200 non-teaching and 101 teaching hospitals throughout the United States found that acute pain services vary significantly, with university/academic institutions being more likely to offer these services than private or Veteran’s Administration (VA) hospitals. However, even in those hospitals with formal acute pain services, many lacked consensus regarding the use of pain management protocols as well as optimal outcome measures for assessing post operative pain therapy (Nasir et al., 2011).
The personnel comprising the typical acute pain service included:
- Anesthesiologists (95%)
- Advanced practice nurses (45%), registered nurses (32.5%), pharmacists (11.3%)
- Physician assistants (8.8%)
- Physical medicine and rehabilitation physicians (6.3%)
- Surgeons (5%)
- Neurologists (3.8%)
- Others (oncologists, social workers, and psychologists) (Nasir et al., 2011)
Treating Pain in the Emergency Department
The emergency department has become a common place to seek treatment for pain. The very nature of the ED means that in most cases the average emergency medicine specialist is primarily concerned with differential diagnosis, ruling out life-threatening disease, and providing stabilizing interventions. For the patient, though, the priorities are likely to include pain management (Thomas, 2013).
In a telephone survey of 500 adults, the American Chronic Pain Association sought to understand the ED experience of those with chronic or recurrent pain. Almost one-half reported “complete” or “a great deal” of pain relief during the ED visit, while 78% endorsed as “somewhat or definitely true” that “the ED staff understood how to treat my pain.” Although more than three-fourths of patients felt that receiving additional information on pain management or referrals to specialists was extremely or very important, only one-half reported receiving them. A significant minority (11%) reported that the “ED staff made me feel like I was just seeking drugs.” The majority (76%) were somewhat to completely satisfied with their treatment, while 24% were neutral or completely dissatisfied. Age, recurrent pain, waiting time, imaging, receiving analgesics, and pain relief predicted patient satisfaction (Todd et al., 2010).
When older adults are treated for pain in the ED, the usual issue is less one of assessment than one of concern for side effects; older patients are simply more likely than younger patients to suffer untoward side effects of many popular ED analgesics such as opioids. A balancing of the risks and benefits of analgesia in older patients is important, and should be discussed with patients and families. The challenge of geriatric analgesia can often be overcome through use of opioid-sparing analgesic regimens or employment of specific therapies (eg, regional nerve blocks for hip fractures) (Thomas, 2013).
Interventional and Surgical Treatments
Interventional techniques are minimally invasive procedures that place drugs in targeted areas or ablate target nerves. This category includes some surgical techniques such as laser or endoscopic discectomy, intrathecal infusion pumps, and spinal cord stimulators, used for the diagnosis and management of chronic, persistent, or intractable pain (Manchikanti et al., 2010).
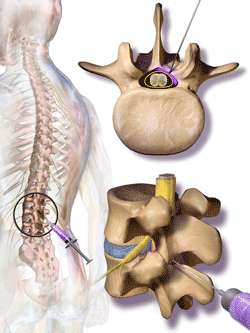
Steroids are injected into the cerebrospinal fluid in the canal surrounding the spine. Nerves branch out from the spine. The nerve roots, which may be compressed, are at the base of the nerves. Source: Blausen.com staff. “Blausen gallery 2014.” Wikiversity Journal of Medicine.
Epidural injections, in which steroids and anti-inflammatories are injected directly into the epidural space of the spinal cord are the most commonly performed procedures in interventional pain management, comprising 46% of all interventional techniques. The most commonly performed procedures are lumbosacral interlaminar or caudal epidural injections. Facet joint interventions are the second most commonly performed procedures, constituting 38% of all interventional techniques in 2011 (Manchikanti et al., 2010).
Conventional thermal radiofrequency (CT-RF) is another minimally invasive procedure in which a thermal lesion is created by applying radiofrequency energy through an electrode placed in the vicinity of the target neural structure. It has been used for some time in cardiac electrophysiology and tumor ablation although its use in the treatment of pain is recent. A variation—water-cooled radiofrequency (WC-RF) ablation—allows a larger volume of the tissue to be heated and the resultant thermal lesion is substantially larger than with conventional thermal radiofrequency (Malik et al., 2011). These techniques are most commonly applied to the intervertebral disc and sacroiliac joints.
There is growing evidence of a disproportionate increase in these interventional techniques and the usefulness of some has been criticized. Analysis of various spinal interventional techniques indicates that there has been an overall increase in interventions of 177% per 100,000 Medicare fee-for-service population with the highest increases seen for sacroiliac joint injections at 331%, facet joint interventions at 308%, epidurals at 130% (Manchikanti et al., 2013).
A systematic review of interventional therapies for low back and radicular pain concluded: “Few nonsurgical interventional therapies for low back pain have been shown to be effective in randomized, placebo-controlled trials.” A systematic review of 18 randomized controlled trials found no strong evidence for or against using injection therapy to treat subacute or chronic low back pain (IOM, 2011).
A review of 30 trials determined that corticosteroid injections (and traction) were not found to be beneficial and are not recommended for lumbosacral radicular syndrome (IOM, 2011). Implantation of spinal cord stimulation and intrathecal drug delivery systems (so-called pain pumps) require routine monitoring, replacement of devices over time, refilling of drug reservoirs, and a balancing of high costs and maintenance requirements against benefits (IOM, 2011).
Although interventional techniques are often considered to be surgical procedures, more invasive procedures such as joint replacement, spinal fusion, and disc replacement are also commonly and successfully used to relieve pain. These types of surgeries often occur after other conservative treatments have failed to relieve the pain.
